Obstet Gynecol Sci.
2023 Sep;66(5):441-448. 10.5468/ogs.22310.
Delta neutrophil index in obese and non-obese polycystic ovary syndrome patients
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Afyonkarahisar University of Health Sciences Faculty of Medicine, Afyonkarahisar, Turkey
- KMID: 2545890
- DOI: http://doi.org/10.5468/ogs.22310
Abstract
Objective
We aimed to evaluate the usefulness of delta neutrophil index (DNI), a new inflammatory marker, in polycystic ovary syndrome (PCOS).
Methods
This retrospective case-control study was conducted at a tertiary health center. The DNI and other blood parameters obtained from the complete blood count examination of 227 individuals, consisting of 72 PCOS patients and 155 controls, were compared between the two groups. A receiver operating characteristic analysis was performed to examine the relationship between DNI and PCOS.
Results
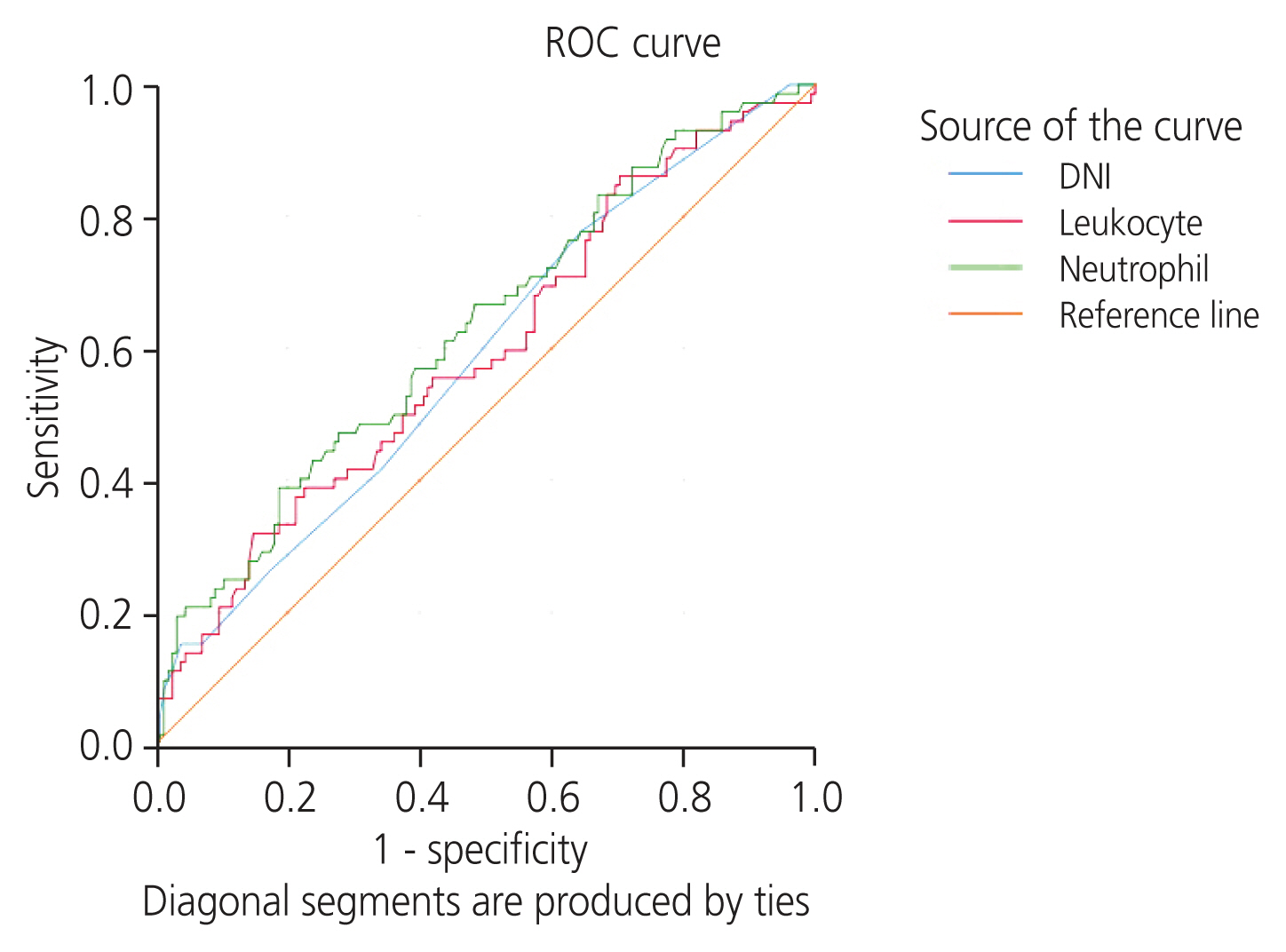
DNI, white blood cell (WBC) count, and neutrophil count were significantly higher in the PCOS group than in the control group (P=0.028, 0.011, and 0.037; respectively). DNI and WBC counts were significantly higher in nonobese-PCOS patients (P=0.018 and 0.041; respectively). When the obese-PCOS and obese-control groups were compared, only neutrophil count was significantly higher in obese-PCOS patients (P=0.016). Significance was observed at cut-off values of 0.015 (area under the curve [AUC]=0.588) (P=0.034; sensitivity, 78%; specificity, 35%; Youden’s index=0.133) for DNI: 9.35 (AUC=0.594) (P=0.022) for WBC; and 5.38 (AUC=0.628) (P=0.002) for neutrophils.
Conclusion
Higher DNI in PCOS patients and similar results in the non-obese-PCOS group were observed when obese and non-obese-PCOS patients were considered separately. However, the lack of difference in the obese-PCOS group strengthens the hypothesis that there is obesity-independent inflammation in PCOS.
Keyword
Figure
Reference
-
References
1. Azziz R, Woods KS, Reyna R, Key TJ, Knochenhauer ES, Yildiz BO. The prevalence and features of the polycystic ovary syndrome in an unselected population. J Clin Endocrinol Metab. 2004; 89:2745–9.2. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod. 2004; 19:41–7.3. Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013; 98:4565–92.4. Dandona P, Aljada A, Chaudhuri A, Bandyopadhyay A. The potential influence of inflammation and insulin resistance on the pathogenesis and treatment of atherosclerosis-related complications in type 2 diabetes. J Clin Endocrinol Metab. 2003; 88:2422–9.5. Abraham Gnanadass S, Divakar Prabhu Y, Valsala Gopalakrishnan A. Association of metabolic and inflammatory markers with polycystic ovarian syndrome (PCOS): an update. Arch Gynecol Obstet. 2021; 303:631–43.6. Guzelmeric K, Alkan N, Pirimoglu M, Unal O, Turan C. Chronic inflammation and elevated homocysteine levels are associated with increased body mass index in women with polycystic ovary syndrome. Gynecol Endocrinol. 2007; 23:505–10.7. Wang J, Gong P, Li C, Pan M, Ding Z, Ge X, et al. Correlation between leptin and IFN-γ involved in granulosa cell apoptosis in PCOS. Gynecol Endocrinol. 2020; 36:1051–6.8. Hatziagelaki E, Pergialiotis V, Kannenberg JM, Trakakis E, Tsiavou A, Markgraf DF, et al. Association between biomarkers of low-grade inflammation and sex hormones in women with polycystic ovary syndrome. Exp Clin Endocrinol Diabetes. 2020; 128:723–30.9. Escobar-Morreale HF, Luque-Ramírez M, González F. Circulating inflammatory markers in polycystic ovary syndrome: a systematic review and metaanalysis. Fertil Steril. 2011; 95:1048–58e1. –2.10. Çakıroğlu Y, Vural F, Vural B. The inflammatory markers in polycystic ovary syndrome: association with obesity and IVF outcomes. J Endocrinol Invest. 2016; 39:899–907.11. Shi Y, Han T, Cui L, Wu G, Zheng R, Xia M, et al. White blood cell differential counts in patients with polycystic ovary syndrome: a pilot study on Chinese women. Eur J Obstet Gynecol Reprod Biol. 2013; 170:162–4.12. Kratz A, Maloum K, O’Malley C, Zini G, Rocco V, Zelmanovic D, et al. Enumeration of nucleated red blood cells with the ADVIA 2120 hematology system: an international multicenter clinical trial. Lab Hematol. 2006; 12:63–70.13. Nierhaus A, Klatte S, Linssen J, Eismann NM, Wichmann D, Hedke J, et al. Revisiting the white blood cell count: immature granulocytes count as a diagnostic marker to discriminate between SIRS and sepsis--a prospective, observational study. BMC Immunol. 2013; 14:8.14. Kim OH, Cha YS, Hwang SO, Jang JY, Choi EH, Kim HI, et al. The use of delta neutrophil index and myeloperoxidase index for predicting acute complicated appendicitis in children. PLoS One. 2016; 11:e0148799.15. Seok Y, Choi JR, Kim J, Kim YK, Lee J, Song J, et al. Delta neutrophil index: a promising diagnostic and prognostic marker for sepsis. Shock. 2012; 37:242–6.16. Lim TS, Kim BK, Lee JW, Lee YK, Chang S, Kim SU, et al. Use of the delta neutrophil index as a prognostic factor of mortality in patients with spontaneous bacterial peritonitis: implications of a simple and useful marker. PLoS One. 2014; 9:e86884.17. Kong T, Park YS, Lee HS, Kim S, Lee JW, Yu G, et al. Value of the delta neutrophil index for predicting 28-day mortality in patients with acute pulmonary embolism in the emergency department. Shock. 2018; 49:649–57.18. Yune HY, Chung SP, Park YS, Chung HS, Lee HS, Lee JW, et al. Delta neutrophil index as a promising prognostic marker in out of hospital cardiac arrest. PLoS One. 2015; 10:e0120677.19. Peng Z, Sun Y, Lv X, Zhang H, Liu C, Dai S. Interleukin-6 levels in women with polycystic ovary syndrome: a systematic review and meta-analysis. PLoS One. 2016; 11:e0148531.20. Rosales C. Neutrophil: a cell with many roles in inflammation or several cell types? Front Physiol. 2018; 9:113.21. Ansari-Lari MA, Kickler TS, Borowitz MJ. Immature granulocyte measurement using the sysmex XE-2100. Relationship to infection and sepsis. Am J Clin Pathol. 2003; 120:795–9.22. Kim H, Kim Y, Lee HK, Kim KH, Yeo CD. Comparison of the delta neutrophil index with procalcitonin and C-reactive protein in sepsis. Clin Lab. 2014; 60:2015–21.23. Shin DH, Cho YS, Kim YS, Ahn HC, Oh YT, Park SO, et al. Delta neutrophil index: a reliable marker to differentiate perforated appendicitis from non-perforated appendicitis in the elderly. J Clin Lab Anal. 2018; 32:e22177.24. Cho HY, Jung I, Kim SJ, Park YW, Kim YH, Kwon JY. Increased delta neutrophil index in women with severe preeclampsia. Am J Reprod Immunol. 2017; 78:e12705.25. Cho HY, Jung I, Kwon JY, Kim SJ, Park YW, Kim YH. The delta neutrophil index as a predictive marker of histological chorioamnionitis in patients with preterm premature rupture of membranes: a retrospective study. PLoS One. 2017; 12:e0173382.26. Yilmaz MA, Duran C, Basaran M. The mean platelet volume and neutrophil to lymphocyte ratio in obese and lean patients with polycystic ovary syndrome. J Endocrinol Invest. 2016; 39:45–53.27. Herlihy AC, Kelly RE, Hogan JL, O’Connor N, Farah N, Turner MJ. Polycystic ovary syndrome and the peripheral blood white cell count. J Obstet Gynaecol. 2011; 31:242–4.28. Dasanu CA, Clark BA 3rd, Ichim TE, Alexandrescu DT. Polycystic ovary syndrome: focus on platelets and prothrombotic risk. South Med J. 2011; 104:174–8.29. Kabil Kucur S, Gozukara I, Aksoy A, Uludag EU, Keskin H, Kamalak Z, et al. How medical treatment affects mean platelet volume as a cardiovascular risk marker in polycystic ovary syndrome? Blood Coagul Fibrinolysis. 2015; 26:862–5.30. Margolis KL, Manson JE, Greenland P, Rodabough RJ, Bray PF, Safford M, et al. Leukocyte count as a predictor of cardiovascular events and mortality in postmenopausal women: the women’s health initiative observational study. Arch Intern Med. 2005; 165:500–8.31. Keskin Kurt R, Okyay AG, Hakverdi AU, Gungoren A, Dolapcioglu KS, Karateke A, et al. The effect of obesity on inflammatory markers in patients with PCOS: a BMI-matched case-control study. Arch Gynecol Obstet. 2014; 290:315–9.32. Ruan X, Dai Y. Study on chronic low-grade inflammation and influential factors of polycystic ovary syndrome. Med Princ Pract. 2009; 18:118–22.33. Phelan N, O’Connor A, Kyaw Tun T, Correia N, Boran G, Roche HM, et al. Leucocytosis in women with polycystic ovary syndrome (PCOS) is incompletely explained by obesity and insulin resistance. Clin Endocrinol (Oxf). 2013; 78:107–13.34. Papalou O, Livadas S, Karachalios A, Tolia N, Kokkoris P, Tripolitakis K, et al. White blood cells levels and PCOS: direct and indirect relationship with obesity and insulin resistance, but not with hyperandogenemia. Hormones (Athens). 2015; 14:91–100.35. Ibáñez L, Jaramillo AM, Ferrer A, de Zegher F. High neutrophil count in girls and women with hyperinsulinaemic hyperandrogenism: normalization with metformin and flutamide overcomes the aggravation by oral contraception. Hum Reprod. 2005; 20:2457–62.36. Silfeler DB, Kurt RK, Yengil E, Un B, Arica S, Baloglu A. Evaluation of mean platelet volume values in lean women with polycystic ovary syndrome. Pak J Med Sci. 2014; 30:589–92.37. Tola EN, Yalcin SE, Dugan N. The predictive effect of inflammatory markers and lipid accumulation product index on clinical symptoms associated with polycystic ovary syndrome in nonobese adolescents and younger aged women. Eur J Obstet Gynecol Reprod Biol. 2017; 214:168–72.38. Talukdar S, Oh DY, Bandyopadhyay G, Li D, Xu J, McNelis J, et al. Neutrophils mediate insulin resistance in mice fed a high-fat diet through secreted elastase. Nat Med. 2012; 18:1407–12.39. Mansuy-Aubert V, Zhou QL, Xie X, Gong Z, Huang JY, Khan AR, et al. Imbalance between neutrophil elastase and its inhibitor α1-antitrypsin in obesity alters insulin sensitivity, inflammation, and energy expenditure. Cell Metab. 2013; 17:534–48.40. Lord GM, Matarese G, Howard JK, Baker RJ, Bloom SR, Lechler RI. Leptin modulates the T-cell immune response and reverses starvation-induced immunosuppression. Nature. 1998; 394:897–901.41. van Rossum EF, Nicklas BJ, Dennis KE, Berman DM, Goldberg AP. Leptin responses to weight loss in postmenopausal women: relationship to sex-hormone binding globulin and visceral obesity. Obes Res. 2000; 8:29–35.42. Gilliver SC, Ashworth JJ, Mills SJ, Hardman MJ, Ashcroft GS. Androgens modulate the inflammatory response during acute wound healing. J Cell Sci. 2006; 119:722–32.43. Tchernof A, Després JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013; 93:359–404.44. Spritzer PM, Lecke SB, Satler F, Morsch DM. Adipose tissue dysfunction, adipokines, and low-grade chronic inflammation in polycystic ovary syndrome. Reproduction. 2015; 149:R219–27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Metformin and Rosiglitazone in Overweight or Obese Women with Polycystic Ovarian Syndrome
- Study on the Insulin Resistance According to Obesity in the Patients with Polycystic Ovarian Syndrome
- Metabolic effects of polycystic ovary syndrome in adolescents
- Adverse pregnancy outcomes with assisted reproductive technology in non-obese women with polycystic ovary syndrome: a case-control study
- Triglyceride Is a Useful Surrogate Marker for Insulin Resistance in Korean Women with Polycystic Ovary Syndrome