J Korean Neurosurg Soc.
2023 Sep;66(5):573-581. 10.3340/jkns.2022.0211.
The Direction of Neurosurgery to Overcome the Living with COVID-19 Era : The Possibility of Telemedicine in Neurosurgery
- Affiliations
-
- 1Department of Neurosurgery, Uijeongbu St. Mary’s Hospital, School of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2545348
- DOI: http://doi.org/10.3340/jkns.2022.0211
Abstract
Objective
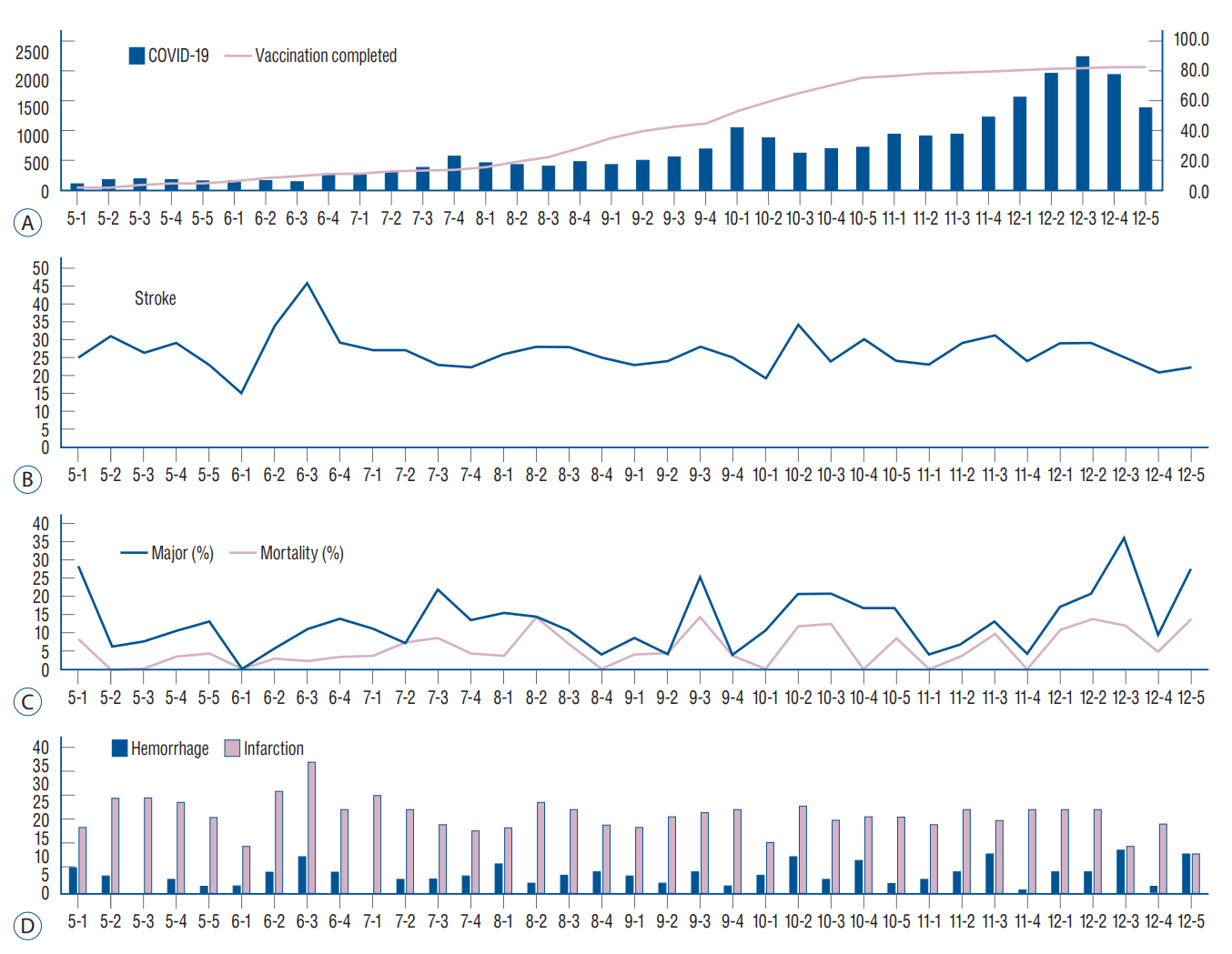
: Due to the implementation of vaccinations and the development of therapeutic agents, the coronavirus disease 2019 (COVID-19) pandemic that started at the end of 2019 has entered a new phase. As a result, neurosurgeons should reconsider the way they treat their patients. As the COVID-19 situation prolongs, the change in neurosurgical emergency patients according to the number of confirmed cases is no longer clear. Outpatient treatment by telephone was permitted according to government policy. In addition, visits to caregivers in the intensive care unit were limited.
Methods
: The electronic medical records of patients who had been treated over the phone for a month (during April 2020, while the hospital was closing) were reviewed. Meanwhile, according to the limited visits to the intensive care unit, a video meeting was held with the caregivers. After the video meeting, satisfaction was evaluated using a questionnaire.
Results
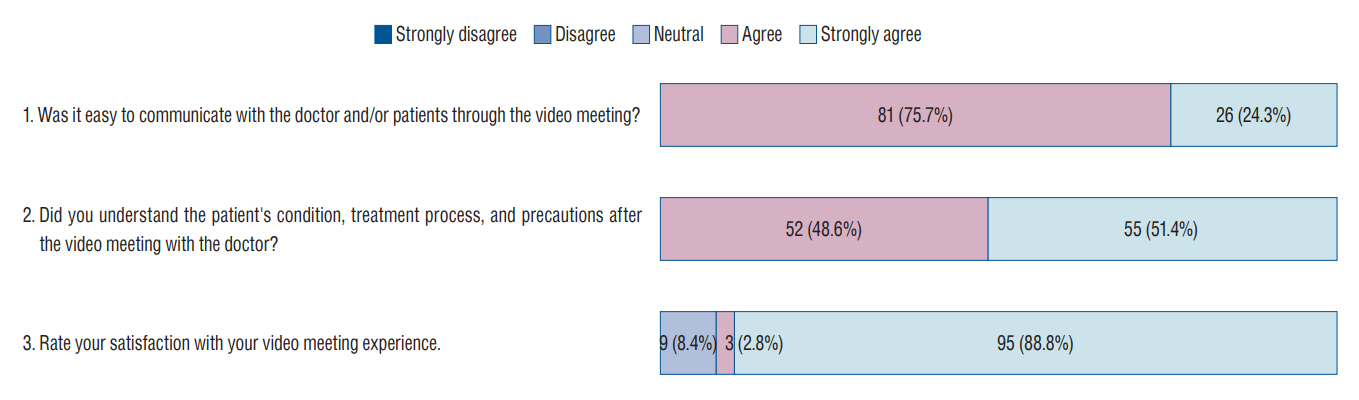
: During April 2020, 1021 patients received non-face-to-face care over the telephone. Among the patients, no critical medical problem occurred due to non-face-to-face care. From July 2021 to December 2021, 321 patients were admitted to the neurosurgical intensive care unit and 107 patients (33.3%) including their caregivers agreed to video visits. Twice a week, advance notice was given that access would be made through a mobile device and the nurse explained to caregivers how to use the mobile device. The time for the video meeting was approximately 20 minutes per patient. Based on the questionnaire, 81 respondents (75.7%) answered that they agreed, and 26 respondents (24.3%) answered that they strongly agreed that was easy to communicate through video meetings. Fifty-two (48.6%) agreed and 55 (51.4%) strongly agreed that they were easy to understand the doctor’s explanation. For overall satisfaction with this video meeting, three respondents (2.8%) gave 4/5 points and 95 respondents (88.8%) gave 5/5 points, and nine (8.4%) gave 3/5 points. Their reason was that there was not enough time.
Conclusion
: In situations where patient visits are limited, video meetings through a mobile device can provide sufficient satisfaction to caregivers. Telemedicine will likely become common in the near future. Health care professionals should prepare and respond to these needs and changes. Therefore, establishing a system with institutional support is necessary.
Keyword
Figure
Cited by 2 articles
-
Letter to Editor Regarding : “The Direction of Neurosurgery to Overcome the Living with COVID-19 Era : The Possibility of Telemedicine in Neurosurgery”
Borislav Kitov, Atanas Davarski, Polina Angelova, Ivo Kehayov
J Korean Neurosurg Soc. 2024;67(1):133-134. doi: 10.3340/jkns.2023.0116.Neurosurgery to Overcome the Living with COVID-19 Era
Hinpetch Daungsupawong, Viroj Wiwanitkit
J Korean Neurosurg Soc. 2024;67(4):483-484. doi: 10.3340/jkns.2023.0196.
Reference
-
References
1. Alessa T, Hawley MS, Hock ES, de Witte L. Smartphone apps to support self-management of hypertension: review and content analysis. JMIR Mhealth Uhealth. 7:e13645. 2019.2. Ashrafzadeh S, Hamdy O. Patient-driven diabetes care of the future in the technology era. Cell Metab. 29:564–575. 2019.3. Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 396:2019–2082. 2021.4. Chen J, Sun D, Zhang S, Shi Y, Qiao F, Zhou Y, et al. Effects of home-based telerehabilitation in patients with stroke: a randomized controlled trial. Neurology. 95:e2318–e2330. 2020.5. Chuo J, Macy ML, Lorch SA. Strategies for evaluating telehealth. Pediatrics. 146:e20201781. 2020.6. de Jong MJ, van der Meulen-de Jong AE, Romberg-Camps MJ, Becx MC, Maljaars JP, Cilissen M, et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 390:959–968. 2017.7. Eichberg DG, Basil GW, Di L, Shah AH, Luther EM, Lu VM, et al. Telemedicine in neurosurgery: lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery. 88:E1–e12. 2020.8. Jang S, Kim D, Yi E, Choi G, Song M, Lee EK. Telemedicine and the use of Korean medicine for patients with COVID-19 in South Korea: observational study. JMIR Public Health Surveill. 7:e20236. 2021.9. Jung EY, Kang HW, Park IH, Park DK. Proposal on the establishment of telemedicine guidelines for Korea. Healthc Inform Res. 21:255–264. 2015.10. Kahn EN, La Marca F, Mazzola CA. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 89:133–138. 2016.11. Kim HS. Towards telemedicine adoption in Korea: 10 practical recommendations for physicians. J Korean Med Sci. 36:e103. 2021.12. Lee MH, Jang SR, Lee TK. Comparative analysis of COVID-19 outbreak and changes in neurosurgical emergency patients. J Korean Neurosurg Soc. 65:130–137. 2022.13. Majmundar N, Ducruet AF, Wilkinson DA, Catapano JS, Patel J, Baranoski JF, et al. Telemedicine for endovascular neurosurgery consultation during the COVID-19 era: patient satisfaction survey. World Neurosurg. 158:e577–582. 2021.14. Mouchtouris N, Lavergne P, Montenegro TS, Gonzalez G, Baldassari M, Sharan A, et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 140:e387–e394. 2020.15. Olson CA, McSwain SD, Curfman AL, Chuo J. The current pediatric telehealth landscape. Pediatrics. 141:e20172334. 2018.16. Omboni S, Caserini M, Coronetti C. Telemedicine and M-health in hypertension management: technologies, applications and clinical evidence. High Blood Press Cardiovasc Prev. 23:187–196. 2016.17. Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: an international expert position paper. Hypertension. 76:1368–1383. 2020.18. Tchero H, Tabue Teguo M, Lannuzel A, Rusch E. Telerehabilitation for stroke survivors: systematic review and meta-analysis. J Med Internet Res. 20:e10867. 2018.19. Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 377:1585–1592. 2017.20. Wang Y, Xue H, Huang Y, Huang L, Zhang D. A systematic review of application and effectiveness of mHealth interventions for obesity and diabetes treatment and self-management. Adv Nutr. 8:449–462. 2017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to Editor Regarding : “The Direction of Neurosurgery to Overcome the Living with COVID-19 Era : The Possibility of Telemedicine in Neurosurgery”
- Neurosurgery to Overcome the Living with COVID-19 Era
- Delays in Intracerebral Hemorrhage Management Is Associated with Hematoma Expansion and Worse Outcomes: Changes in COVID-19 Era
- Towards Telemedicine Adoption in Korea: 10 Practical Recommendations for Physicians
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak