Ann Surg Treat Res.
2023 Aug;105(2):91-98. 10.4174/astr.2023.105.2.91.
Comparison of Medisonic with Harmonic HD 1000i and Sonicision ultrasonic energy device in laparoscopic gastrectomy: a pilot randomized clinical trial
- Affiliations
-
- 1Division of Gastrointestinal Surgery, Department of Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Robotic Surgery Center, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2545160
- DOI: http://doi.org/10.4174/astr.2023.105.2.91
Abstract
- Purpose
This study aimed to compare the clinical performance of Medisonic (Daiwha Corp.) to that of Harmonic HD 1000i (Ethicon Endo-Surgery Inc.) and Sonicision (Medtronic) in patients undergoing gastrectomy for gastric cancer.
Methods
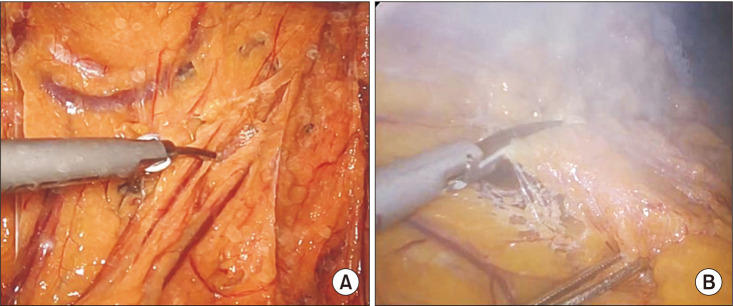
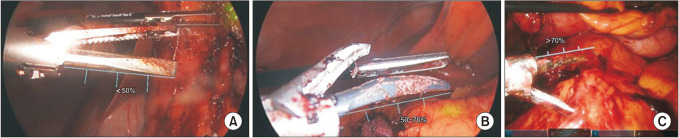
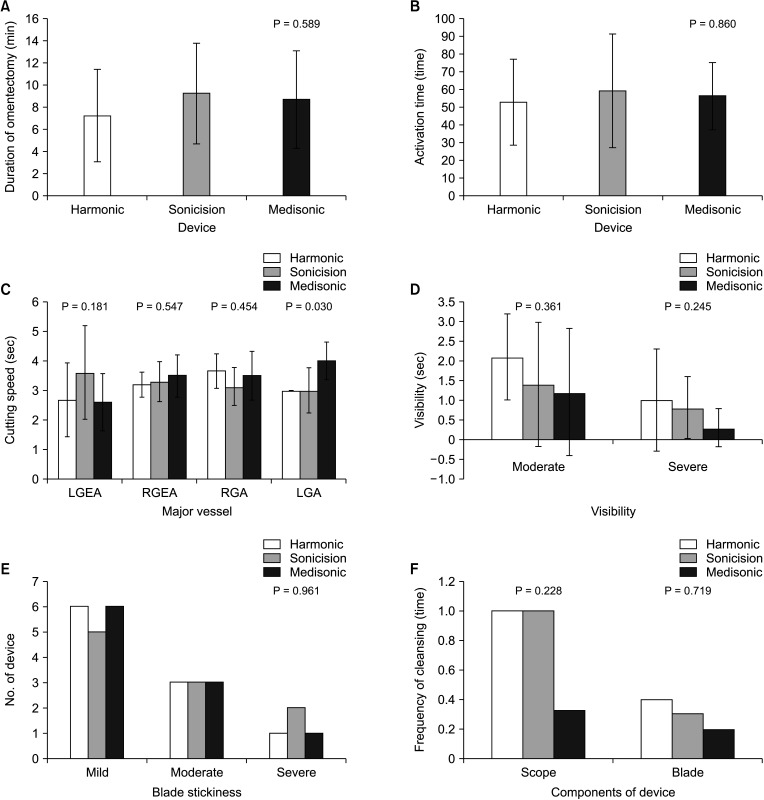
A total of 30 patients were enrolled in this prospective randomized study. The patients were randomly assigned to a Medisonic (M group, n = 10), Harmonic HD 1000i (H group, n = 10), or Sonicision (S group, n = 10) groups. Primary outcome was cutting speed and activation times during omentectomy. Other variables were visibility of surgical field, blade stickiness, and clinical outcomes, including operation-related complications.
Results
Clinicopathologic characteristics, including age, sex, body mass index, or stage were not different between the 3 groups. Operative outcomes, including operation time, estimated blood loss, and postoperative hospital stay were not different between the 3 groups. There was no significant difference in 30-day postoperative complications. The running time of omentectomy was 7.3, 9.2, and 8.7 minutes in the H, S, and M groups, respectively, with no statistical difference (P = 0.589). We also looked at the activation times during the omentectomy, and there was no statistical difference between the groups (52.6 times vs. 58.9 times vs. 56.2 times in the H, S, and M groups, respectively; P = 0.860).
Conclusion
Medisonic is safe and efficient to perform laparoscopic radical gastrectomy and is not inferior to Harmonic HD 1000i or Sonicision in terms of clinical outcomes and cutting/sealing function.
Keyword
Figure
Reference
-
1. Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020; 396:635–648. PMID: 32861308.
Article2. Johnston FM, Beckman M. Updates on management of gastric cancer. Curr Oncol Rep. 2019; 21:67. PMID: 31236716.
Article3. Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, et al. Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol. 2020; 38:3304–3313. PMID: 32816629.
Article4. Kim YN, Yoo YC, Guner A, Cho I, Kwon IG, Kim YN, et al. Comparison of perioperative surgical outcomes between a bipolar device and an ultrasonic device during laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2015; 29:589–595. PMID: 25015523.
Article5. Tsimoyiannis EC, Jabarin M, Tsimoyiannis JC, Betzios JP, Tsilikatis C, Glantzounis G. Ultrasonically activated shears in extended lymphadenectomy for gastric cancer. World J Surg. 2002; 26:158–161. PMID: 11865342.6. Lee SH, Nguyen TK, Ong WS, Haaland B, Tay GC, Tan NC, et al. Comparing the utility and surgical outcomes of harmonic focus ultrasonic scalpel with ligasure small jaw bipolar device in thyroidectomies: a prospective randomized controlled trial. Ann Surg Oncol. 2019; 26:4414–4422. PMID: 31512024.
Article7. Inoue K, Nakane Y, Michiura T, Yamada M, Mukaide H, Fukui J, et al. Ultrasonic scalpel for gastric cancer surgery: a prospective randomized study. J Gastrointest Surg. 2012; 16:1840–1846. PMID: 22833440.
Article8. Cheng H, Hsiao CW, Clymer JW, Schwiers ML, Tibensky BN, Patel L, et al. Gastrectomy and D2 lymphadenectomy for gastric cancer: a meta-analysis comparing the harmonic scalpel to conventional techniques. Int J Surg Oncol. 2015; 2015:397260. PMID: 26075090.
Article9. Huang Y, Mu GC, Qin XG, Lin JL, Liu C, Chen ZB, et al. The application of ultrasonic harmonic scalpel in the radical surgery of gastric cancer. Clin Transl Oncol. 2013; 15:932–937. PMID: 23519537.
Article10. Guideline Committee of the Korean Gastric Cancer Association (KGCA). Development Working Group & Review Panel. Korean practice guideline for gastric cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019; 19:1–48. PMID: 30944757.11. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021; 24:1–21. PMID: 32060757.12. Chen XL, Chen XZ, Lu ZH, Wang L, Yang K, Hu JK, et al. Comparison of ultrasonic scalpel versus conventional techniques in open gastrectomy for gastric carcinoma patients: a systematic review and meta-analysis. PLoS One. 2014; 9:e103330. PMID: 25079780.
Article13. Matthey-Gié ML, Gié O, Deretti S, Demartines N, Matter M. Prospective randomized study to compare lymphocele and lymphorrhea control following inguinal and axillary therapeutic lymph node dissection with or without the use of an ultrasonic scalpel. Ann Surg Oncol. 2016; 23:1716–1720. PMID: 26714939.
Article14. Suzuki K, Shimizu M, Sakagami T, Yagi M, Fujisawa T, Sawada S, et al. A comparison of short-term outcomes of neck dissection for head and neck cancers using Thunderbeatκ, LigaSureκ or treatment without an energy-based device: a case controlled study. Int J Surg. 2018; 58:60–64. PMID: 30248411.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Prospective, Randomized, Controlled Comparative Study of Three Energy Devices in Open Thyroid Surgery: Thunderbeat, Harmonic, and Ligasure
- Usefulness of cordless ultrasonic cutting energy devices in endoscopic nipple-sparing mastectomy: a retrospective study
- Current status of robotic gastrectomy for gastric cancer: A review of recent randomized controlled trials
- Late Onset Iatrogenic Diaphragmatic Hernia after Laparoscopy-Assisted Total Gastrectomy for Gastric Cancer
- Ultrasonic energy in endoscopic surgery