Intest Res.
2023 Jul;21(3):318-327. 10.5217/ir.2022.00116.
Risk of venous thromboembolism with a central venous catheter in hospitalized Japanese patients with inflammatory bowel disease: a propensity score-matched cohort study
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keio University School of Medicine, Tokyo, Japan
- 2Center for Diagnostic and Therapeutic Endoscopy, Keio University School of Medicine, Tokyo, Japan
- 3Center for Preventive Medicine, Keio University School of Medicine, Tokyo, Japan
- KMID: 2544755
- DOI: http://doi.org/10.5217/ir.2022.00116
Abstract
- Background/Aims
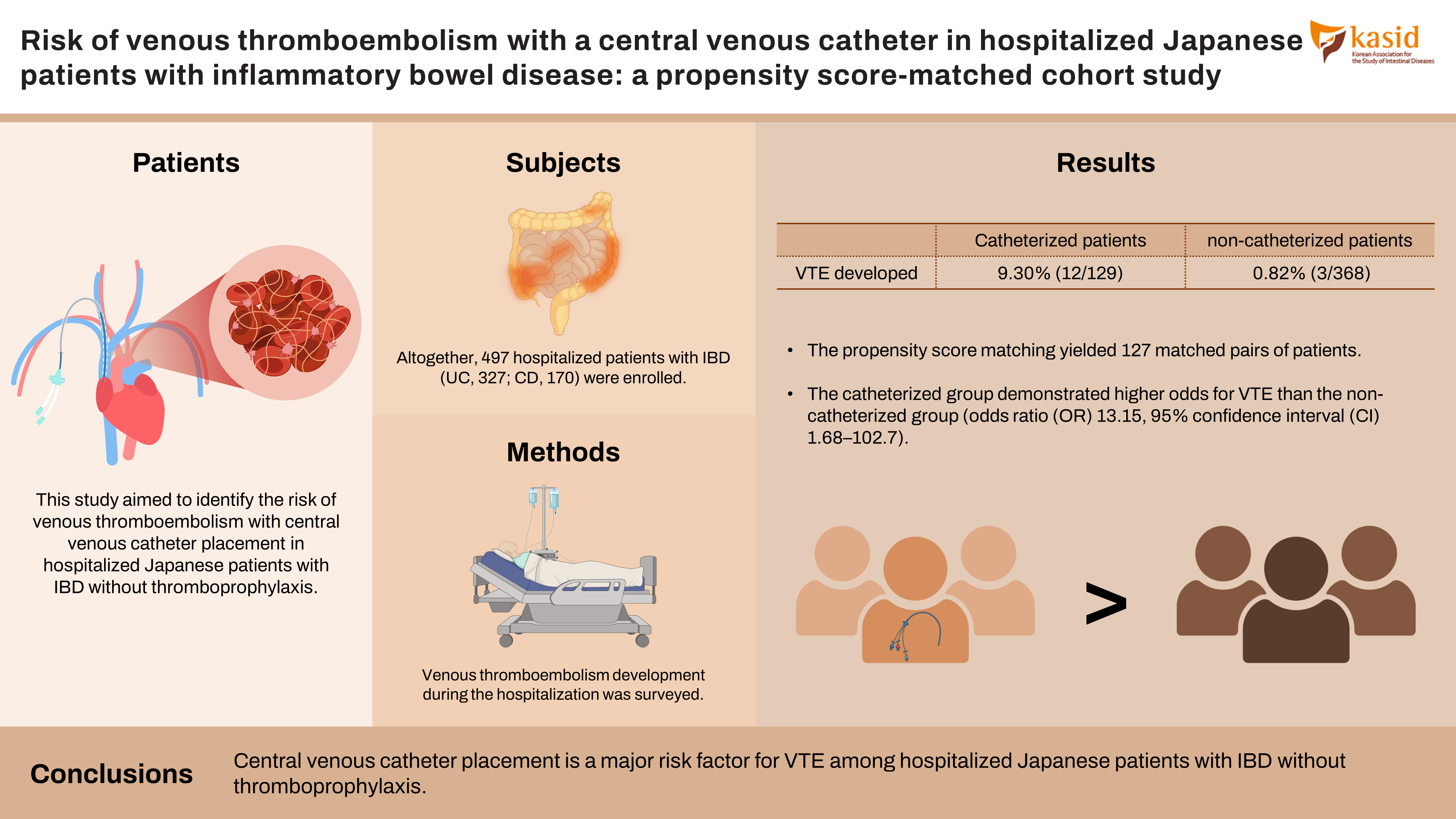
Thromboprophylaxis is recommended for hospitalized patients with inflammatory bowel disease (IBD) in Western countries, although it is selectively administered to high-risk patients in East Asia. A central venous catheter (CVC) is commonly placed in patients with IBD. Although CVC placement is considered a risk factor for venous thromboembolism (VTE), the degree of increased risk in patients with IBD is uncertain. This study aimed to identify the risk of VTE with CVC placement in hospitalized Japanese patients with IBD without thromboprophylaxis.
Methods
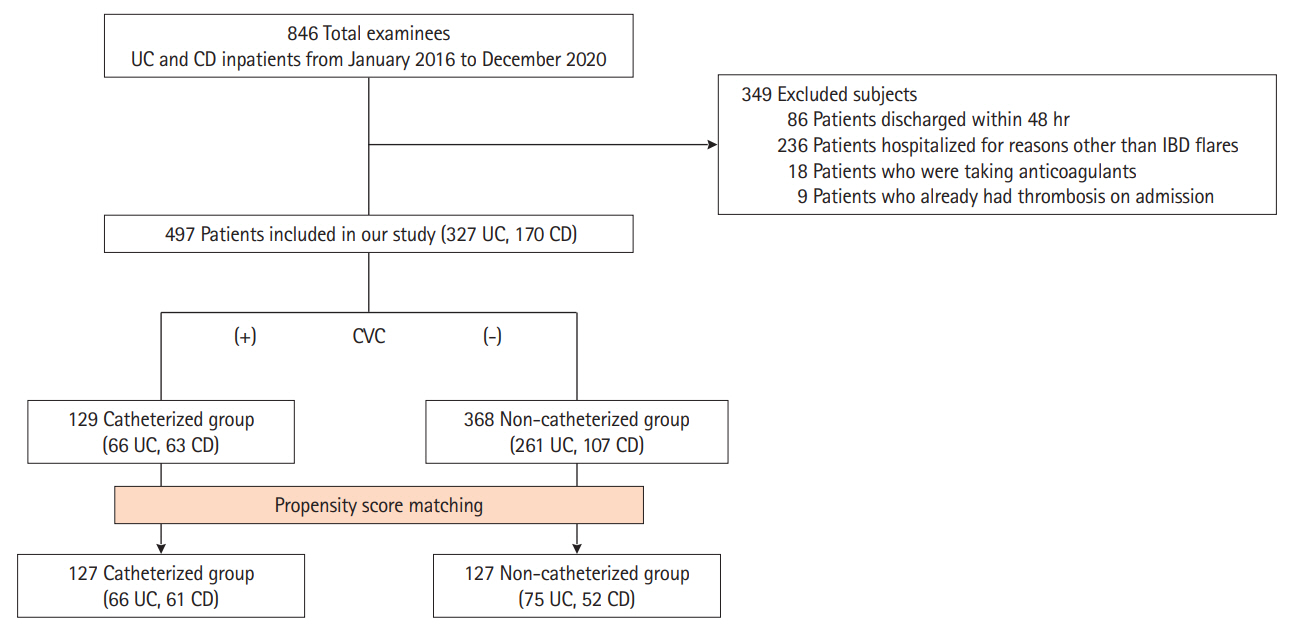
This retrospective cohort study included patients with ulcerative colitis or Crohn’s disease who were admitted for disease flares at Keio University Hospital between January 2016 and December 2020. Patients who already had thrombosis or were administered any antithrombotic treatment on admission were excluded. VTE development during the hospitalization was surveyed, and VTE risk associated with CVC indwelling was estimated using propensity score matching and inverse probability of treatment weighting analyses.
Results
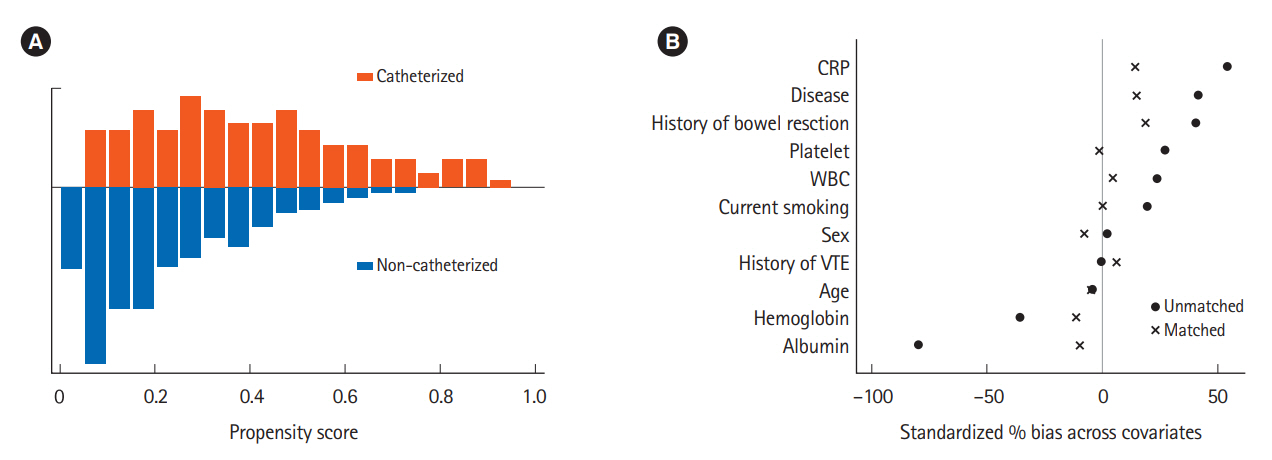
Altogether, 497 hospitalized patients with IBD (ulcerative colitis, 327; Crohn’s disease, 170) were enrolled. VTE developed in 9.30% (12/129) of catheterized patients and in 0.82% (3/368) of non-catheterized patients. The propensity score matching yielded 127 matched pairs of patients. The catheterized group demonstrated higher odds for VTE than the non-catheterized group (odds ratio, 13.15; 95% confidence interval, 1.68–102.70). A similar result was obtained in the inverse probability of treatment weighting analysis (odds ratio, 11.02; 95% confidence interval, 2.64–46.10).
Conclusions
CVC placement is a major risk factor for VTE among hospitalized Japanese patients with IBD without thromboprophylaxis.
Keyword
Figure
Reference
-
1. Olivera PA, Zuily S, Kotze PG, et al. International consensus on the prevention of venous and arterial thrombotic events in patients with inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2021; 18:857–873.
Article2. Bernstein CN, Nugent Z, Singh H. Persistently high rate of venous thromboembolic disease in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2021; 116:1476–1484.
Article3. Harbord M, Annese V, Vavricka SR, et al. The first European evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J Crohns Colitis. 2016; 10:239–254.4. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008; 103:2272–2280.5. Andrade AR, Barros LL, Azevedo MF, et al. Risk of thrombosis and mortality in inflammatory bowel disease. Clin Transl Gastroenterol. 2018; 9:142.6. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010; 375:657–663.7. Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019; 114:384–413.8. Lamb CA, Kennedy NA, Raine T, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019; 68(Suppl 3):s1–s106.
Article9. Weng MT, Park SH, Matsuoka K, et al. Incidence and risk factor analysis of thromboembolic events in East Asian patients with inflammatory bowel disease, a multinational collaborative study. Inflamm Bowel Dis. 2018; 24:1791–1800.
Article10. Chung WS, Lin CL, Hsu WH, Kao CH. Inflammatory bowel disease increases the risks of deep vein thrombosis and pulmonary embolism in the hospitalized patients: a nationwide cohort study. Thromb Res. 2015; 135:492–496.
Article11. Nakase H, Uchino M, Shinzaki S, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease 2020. J Gastroenterol. 2021; 56:489–526.
Article12. Ando K, Fujiya M, Watanabe K, et al. A nationwide survey concerning the mortality and risk of progressing severity due to arterial and venous thromboembolism in inflammatory bowel disease in Japan. J Gastroenterol. 2021; 56:1062–1079.
Article13. Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001; 85:430–434.
Article14. Kappelman MD, Horvath-Puho E, Sandler RS, et al. Thromboembolic risk among Danish children and adults with inflammatory bowel diseases: a population-based nationwide study. Gut. 2011; 60:937–943.
Article15. Citla Sridhar D, Abou-Ismail MY, Ahuja SP. Central venous catheter-related thrombosis in children and adults. Thromb Res. 2020; 187:103–112.
Article16. Bhakta A, Tafen M, Ahmed M, et al. Risk of catheter-associated deep venous thrombosis in inflammatory bowel disease. Dis Colon Rectum. 2014; 57:1379–1383.
Article17. Ohta Y, Arai M, Nakagawa T, et al. Comparison of a novel predictor of venous thromboembolic complications in inflammatory bowel disease with current predictors. J Gastroenterol Hepatol. 2019; 34:870–879.
Article18. Ando K, Fujiya M, Nomura Y, et al. The incidence and risk factors of venous thromboembolism in patients with inflammatory bowel disease: a prospective multicenter cohort study. Digestion. 2019; 100:229–237.
Article19. Ando K, Fujiya M, Nomura Y, et al. The incidence and risk factors of venous thromboembolism in Japanese inpatients with inflammatory bowel disease: a retrospective cohort study. Intest Res. 2018; 16:416–425.
Article20. JCS Joint Working Group. Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS 2009). Circ J. 2011; 75:1258–1281.21. Bang SM, Jang MJ, Kim KH, et al. Prevention of venous thromboembolism, 2nd edition: Korean Society of Thrombosis and Hemostasis Evidence-based Clinical Practice Guidelines. J Korean Med Sci. 2014; 29:164–171.
Article22. Pascual-Figal DA, Redondo B, Caro C, et al. Comparison of late mortality in hospitalized patients >70 years of age with systolic heart failure receiving beta blockers versus those not receiving beta blockers. Am J Cardiol. 2008; 102:1711–1717.
Article23. Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011; 10:150–161.
Article24. Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004; 23:2937–2960.
Article25. Austin PC. The performance of different propensity-score methods for estimating differences in proportions (risk differences or absolute risk reductions) in observational studies. Stat Med. 2010; 29:2137–2148.
Article26. Ananthakrishnan AN, Cagan A, Gainer VS, et al. Thromboprophylaxis is associated with reduced post-hospitalization venous thromboembolic events in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014; 12:1905–1910.
Article27. Weng MT, Tung CC, Wong JM, Wei SC. Should Asian inflammatory bowel disease patients need routine thromboprophylaxis? Intest Res. 2018; 16:312–314.
Article28. Nguyen GC, Bernstein CN, Bitton A, et al. Consensus statements on the risk, prevention, and treatment of venous thromboembolism in inflammatory bowel disease: Canadian Association of Gastroenterology. Gastroenterology. 2014; 146:835–848.
Article29. Imbrizi MR, Magro DO, Secundo TM, et al. Hypoalbuminemia as a risk factor for thromboembolic events in inflammatory bowel disease inpatients. Intest Res. 2019; 17:63–69.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The incidence and risk factors of venous thromboembolism in Japanese inpatients with inflammatory bowel disease: a retrospective cohort study
- Venous Thromboembolism Risk in Asian Patients with Inflammatory Bowel Disease: A Population-Based Nationwide Inception Cohort Study
- Prevention and Treatment of Thromboembolism in Patients with Inflammatory Bowel Disease
- Inflammatory bowel disease and superior mesenteric artery thromboembolism
- Knowledge, Awareness and Risk of Occurrence of Venous Thromboembolism of Perinatal Women