Intest Res.
2018 Jul;16(3):416-425. 10.5217/ir.2018.16.3.416.
The incidence and risk factors of venous thromboembolism in Japanese inpatients with inflammatory bowel disease: a retrospective cohort study
- Affiliations
-
- 1Division of Gastroenterology and Hematology/Oncology, Department of Medicine, Asahikawa Medical University, Asahikawa, Japan. fjym@asahikawa-med.ac.jp
- 2Department of Gastroenterology, Asahikawa City Hospital, Asahikawa, Japan.
- KMID: 2417654
- DOI: http://doi.org/10.5217/ir.2018.16.3.416
Abstract
- BACKGROUND/AIMS
Venous thromboembolism (VTE) is a major extraintestinal manifestation in inflammatory bowel disease (IBD), regarded as an independent risk factor for VTE according to reports from Western countries. However, the incidence and risk factors of VTE in Asian IBD patients are not fully understood. We aimed to reveal the incidence and risk factors of VTE in Japanese IBD inpatients.
METHODS
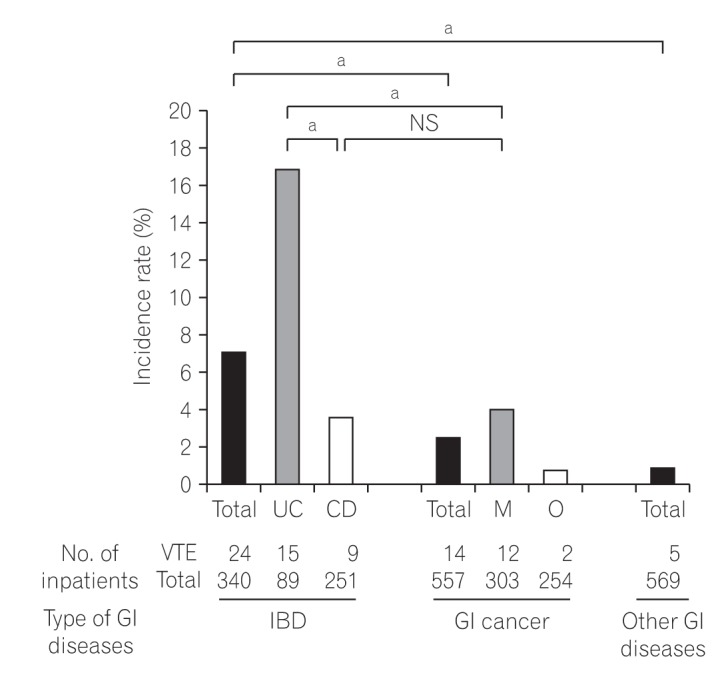
The incidence of VTE in inpatients with IBD (n=340), gastrointestinal cancers (n=557), and other gastrointestinal diseases (n=569) treated at our hospital from 2009 to 2013 was retrospectively investigated. The characteristics and laboratory data of IBD inpatients with and without VTE were compared in univariate and multivariate analyses. Clinical courses of VTE in IBD were surveyed.
RESULTS
VTE was detected in 7.1% of IBD inpatients, significantly higher than in gastrointestinal cancer inpatients (2.5%) and inpatients with other gastrointestinal diseases (0.88%). The incidence of VTE in ulcerative colitis (UC) patients (16.7%) was much higher than that in those with Crohn's disease (3.6%). In the univariate analysis, the risk factors were an older age, central venous catheter, prednisolone, surgery, low serum albumin, high serum C-reactive protein and D-dimer. According to a multivariate analysis, >50 years of age and surgery were the only risk factors. The in-hospital mortality rate of IBD inpatients with VTE was 4.2%.
CONCLUSIONS
The incidence of VTE with IBD, especially UC, was found to be high compared with other digestive disease, which was almost equivalent to that of Western countries. The efficacy of prophylaxis needs to be investigated in Asian IBD patients.
MeSH Terms
-
Asian Continental Ancestry Group*
C-Reactive Protein
Central Venous Catheters
Cohort Studies*
Colitis, Ulcerative
Crohn Disease
Gastrointestinal Diseases
Gastrointestinal Neoplasms
Hospital Mortality
Humans
Incidence*
Inflammatory Bowel Diseases*
Inpatients*
Multivariate Analysis
Prednisolone
Retrospective Studies*
Risk Factors*
Serum Albumin
Venous Thromboembolism*
C-Reactive Protein
Prednisolone
Serum Albumin
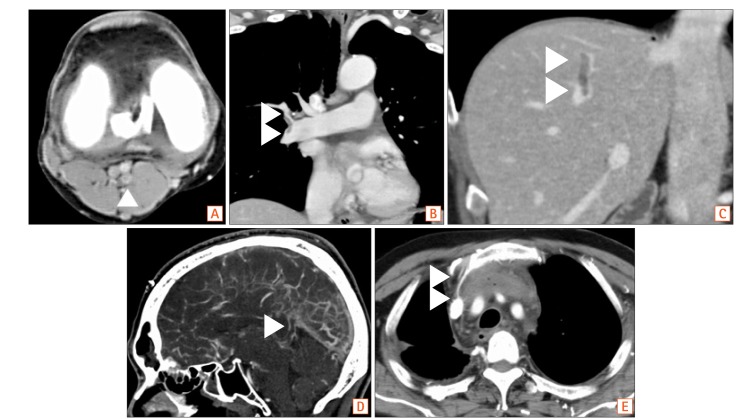
Figure
Cited by 2 articles
-
Incidence and risk factors for venous thrombosis among patients with inflammatory bowel disease in China: a multicenter retrospective study
Jing Liu, Xiang Gao, Ye Chen, Qiao Mei, Liangru Zhu, Jiaming Qian, Pinjin Hu, Qian Cao
Intest Res. 2021;19(3):313-322. doi: 10.5217/ir.2020.00017.Risk of venous thromboembolism with a central venous catheter in hospitalized Japanese patients with inflammatory bowel disease: a propensity score-matched cohort study
Yasuhiro Aoki, Hiroki Kiyohara, Yohei Mikami, Kosaku Nanki, Takaaki Kawaguchi, Yusuke Yoshimatsu, Shinya Sugimoto, Tomohisa Sujino, Kaoru Takabayashi, Naoki Hosoe, Haruhiko Ogata, Yasushi Iwao, Takanori Kanai
Intest Res. 2023;21(3):318-327. doi: 10.5217/ir.2022.00116.
Reference
-
1. Papa A, Papa V, Marzo M, et al. Prevention and treatment of venous thromboembolism in patients with IBD: a trail still climbing. Inflamm Bowel Dis. 2015; 21:1204–1213. PMID: 25581834.
Article2. Purnak T, Yuksel O. Overview of venous thrombosis in inflammatory bowel disease. Inflamm Bowel Dis. 2015; 21:1195–1203. PMID: 25581828.
Article3. Danese S, Papa A, Saibeni S, Repici A, Malesci A, Vecchi M. Inflammation and coagulation in inflammatory bowel disease: the clot thickens. Am J Gastroenterol. 2007; 102:174–186. PMID: 17100967.
Article4. Zitomersky NL, Verhave M, Trenor CC 3rd. Thrombosis and inflammatory bowel disease: a call for improved awareness and prevention. Inflamm Bowel Dis. 2011; 17:458–470. PMID: 20848518.
Article5. Talbot RW, Heppell J, Dozois RR, Beart RW Jr. Vascular complications of inflammatory bowel disease. Mayo Clin Proc. 1986; 61:140–145. PMID: 3080643.
Article6. Webberley MJ, Hart MT, Melikian V. Thromboembolism in inflammatory bowel disease: role of platelets. Gut. 1993; 34:247–251. PMID: 8432482.
Article7. Sloan WP Jr, Bargen JA, Gage RB. Life histories of patients with chronic ulcerative colitis: a review of 2,000 cases. Gastroenterology. 1968; 54(Suppl):819–822.
Article8. Miehsler W, Reinisch W, Valic E, et al. Is inflammatory bowel disease an independent and disease specific risk factor for thromboembolism? Gut. 2004; 53:542–548. PMID: 15016749.
Article9. Nguyen GC, Sam J. Rising prevalence of venous thromboembolism and its impact on mortality among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008; 103:2272–2280. PMID: 18684186.
Article10. Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010; 375:657–663. PMID: 20149425.
Article11. Sinagra E, Aragona E, Romano C, et al. The role of portal vein thrombosis in the clinical course of inflammatory bowel diseases: report on three cases and review of the literature. Gastroenterol Res Pract. 2012; 2012:916428. DOI: 10.1155/2012/916428. PMID: 23093957.
Article12. Cognat E, Crassard I, Denier C, Vahedi K, Bousser MG. Cerebral venous thrombosis in inflammatory bowel diseases: eight cases and literature review. Int J Stroke. 2011; 6:487–492. PMID: 22017824.
Article13. Sonoda K, Ikeda S, Mizuta Y, Miyahara Y, Kohno S. Evaluation of venous thromboembolism and coagulation-fibrinolysis markers in Japanese patients with inflammatory bowel disease. J Gastroenterol. 2004; 39:948–954. PMID: 15549447.
Article14. Scarpa M, Pilon F, Pengo V, et al. Deep venous thrombosis after surgery for inflammatory bowel disease: is standard dose low molecular weight heparin prophylaxis enough? World J Surg. 2010; 34:1629–1636. PMID: 20177681.
Article15. Alatri A, Schoepfer A, Fournier N, et al. Prevalence and risk factors for venous thromboembolic complications in the Swiss Inflammatory Bowel Disease Cohort. Scand J Gastroenterol. 2016; 51:1200–1205. PMID: 27211077.
Article16. Stadnicki A. Involvement of coagulation and hemostasis in inflammatory bowel diseases. Curr Vasc Pharmacol. 2012; 10:659–669. PMID: 22272910.
Article17. Chiarantini E, Valanzano R, Liotta AA, et al. Hemostatic abnormalities in inflammatory bowel disease. Thromb Res. 1996; 82:137–146. PMID: 9163067.
Article18. Kjeldsen J, Lassen JF, Brandslund I, Schaffalitzky de. Markers of coagulation and fibrinolysis as measures of disease activity in inflammatory bowel disease. Scand J Gastroenterol. 1998; 33:637–643. PMID: 9669637.
Article19. Weber P, Husemann S, Vielhaber H, Zimmer KP, Nowak-Göttl U. Coagulation and fibrinolysis in children, adolescents, and young adults with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1999; 28:418–422. PMID: 10204507.
Article20. Heit JA. The epidemiology of venous thromboembolism in the community: implications for prevention and management. J Thromb Thrombolysis. 2006; 21:23–29. PMID: 16475038.
Article21. Fichera A, Cicchiello LA, Mendelson DS, Greenstein AJ, Heimann TM. Superior mesenteric vein thrombosis after colectomy for inflammatory bowel disease: a not uncommon cause of postoperative acute abdominal pain. Dis Colon Rectum. 2003; 46:643–648. PMID: 12792441.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Venous Thromboembolism Risk in Asian Patients with Inflammatory Bowel Disease: A Population-Based Nationwide Inception Cohort Study
- Inflammatory bowel disease and superior mesenteric artery thromboembolism
- Prevention and Treatment of Thromboembolism in Patients with Inflammatory Bowel Disease
- Risk of venous thromboembolism with a central venous catheter in hospitalized Japanese patients with inflammatory bowel disease: a propensity score-matched cohort study
- Knowledge, Awareness and Risk of Occurrence of Venous Thromboembolism of Perinatal Women