Obstet Gynecol Sci.
2023 Jul;66(4):253-269. 10.5468/ogs.22175.
The complement system in preeclampsia: a review of its activation and endothelial injury in the triad of COVID-19 infection and HIV-associated preeclampsia
- Affiliations
-
- 1Optics and Imaging Centre, Dorris Duke Medical Research Institute, Nelson R. Mandela School of Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
- KMID: 2544382
- DOI: http://doi.org/10.5468/ogs.22175
Abstract
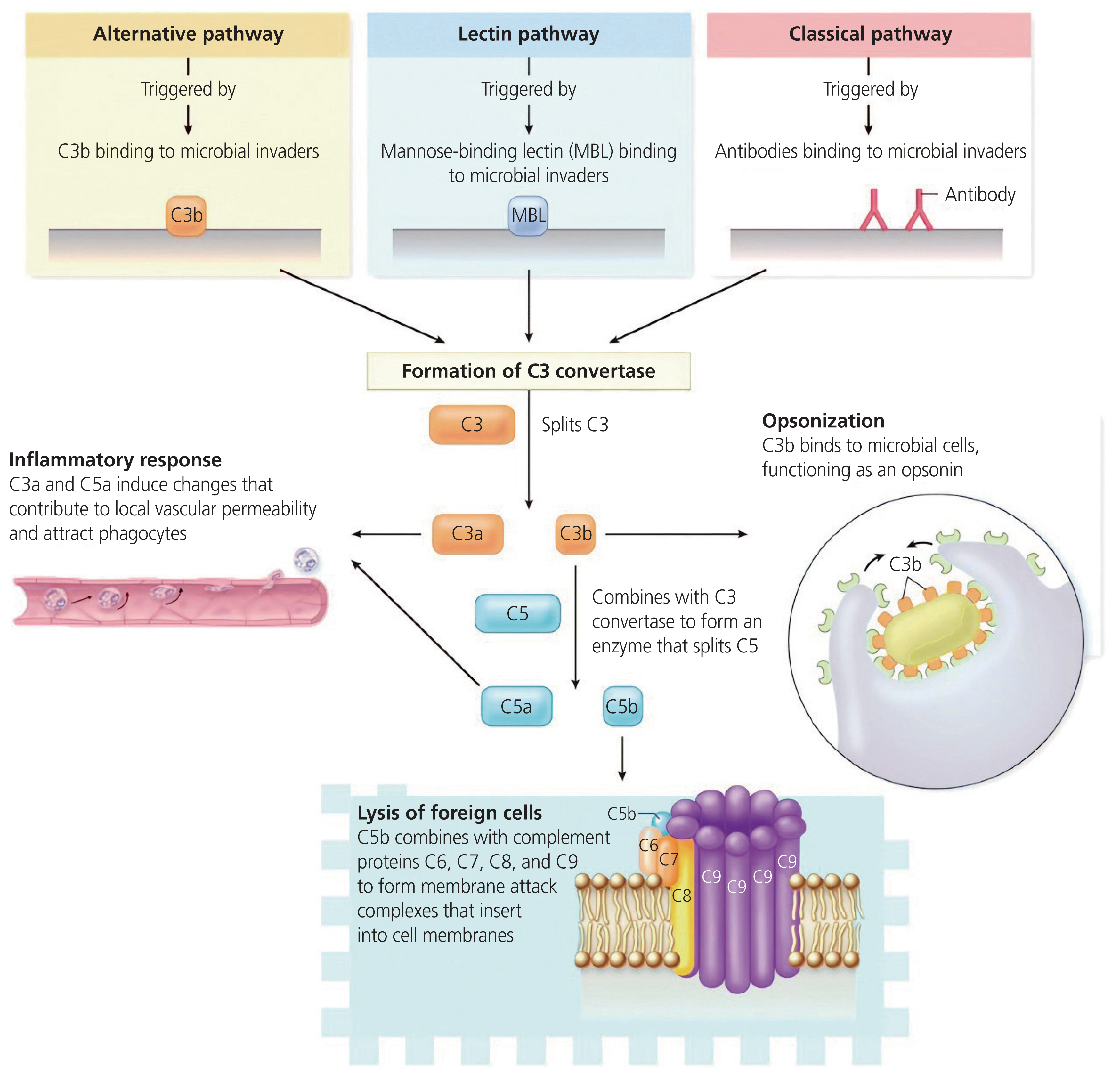
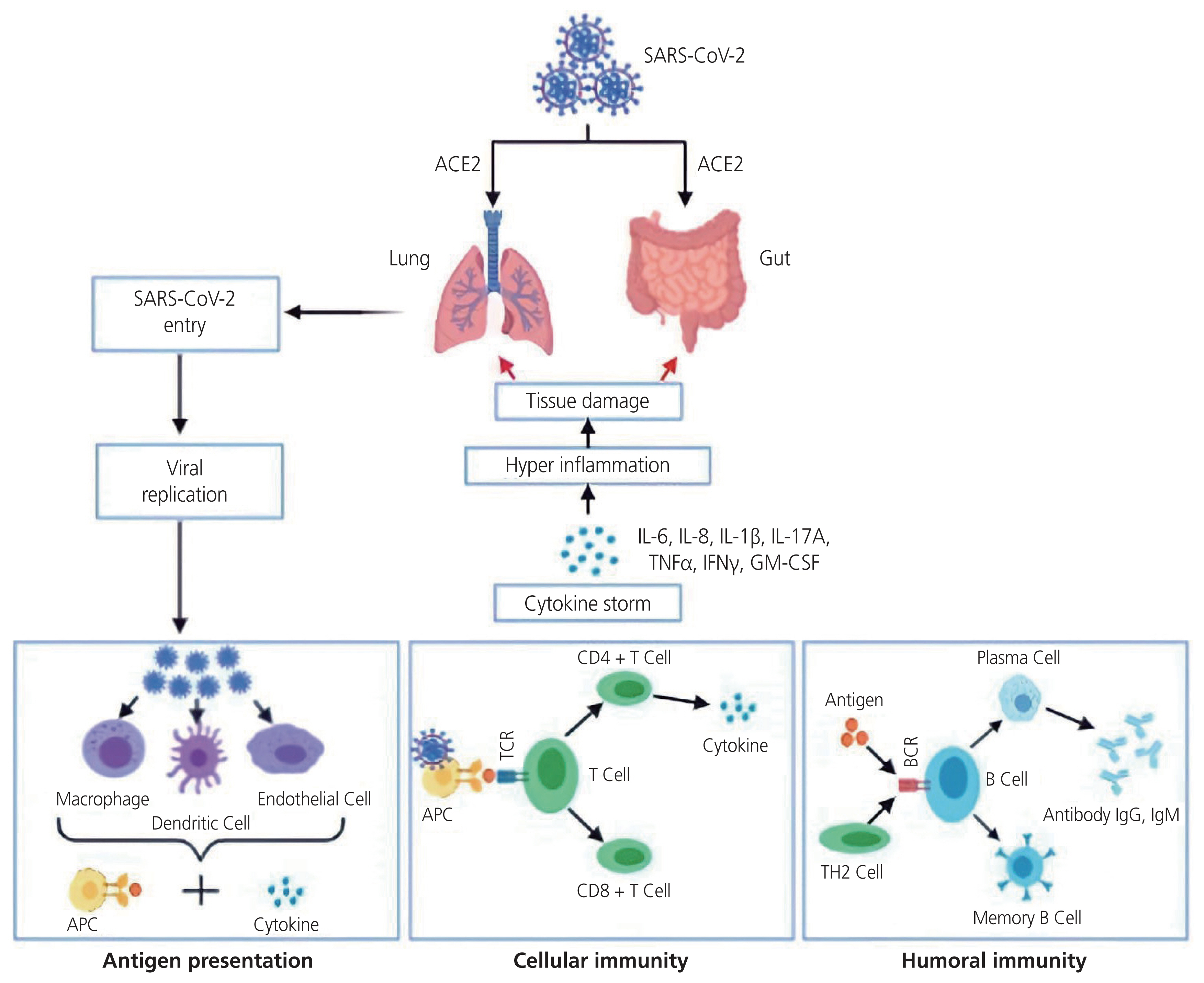
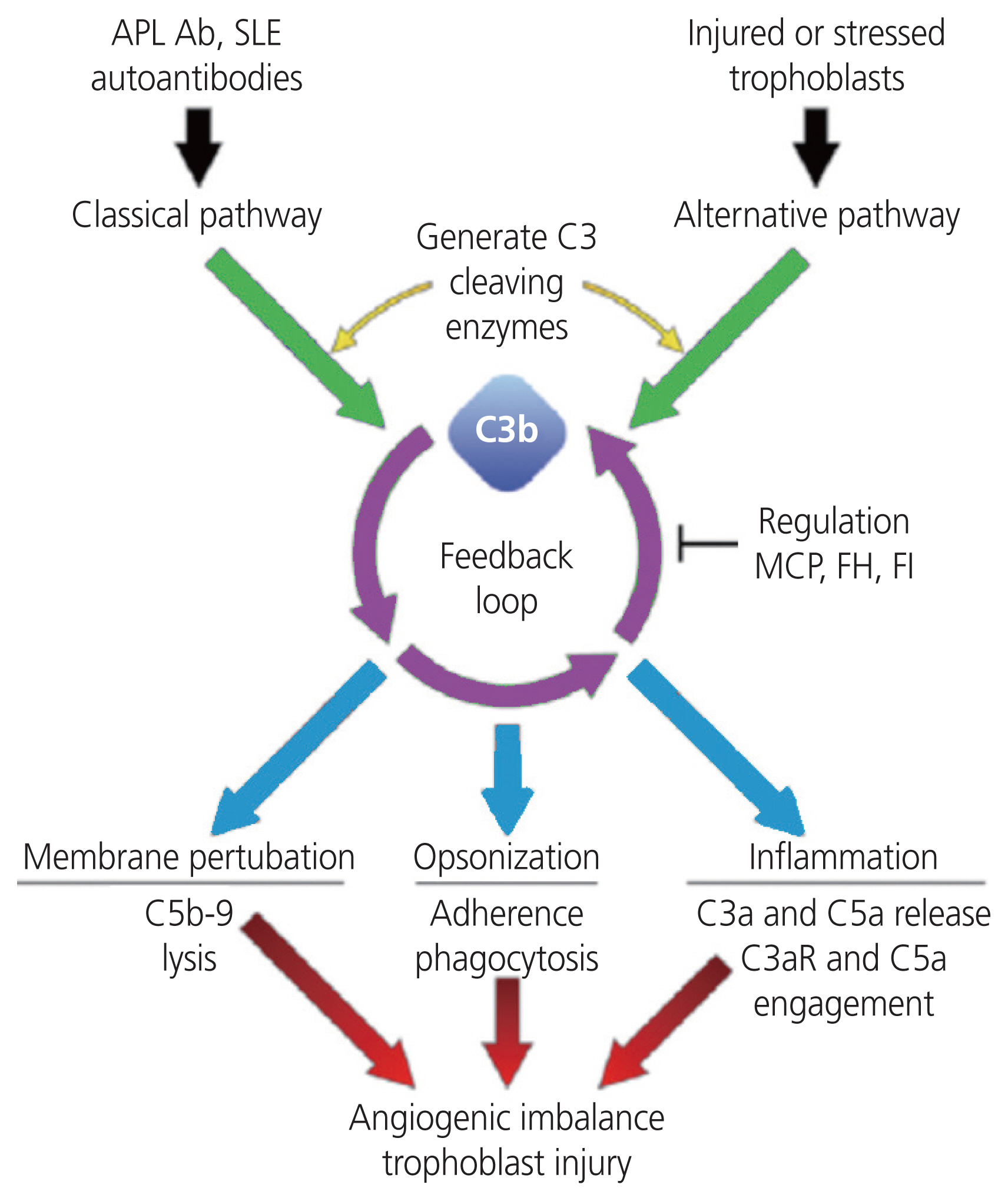
- This review assesses the complement system and its activation, with the pathological features of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), human immunodeficiency virus (HIV) infection and preeclampsia (PE). The complement system is the first defensive response by the host innate immune system to viral pathogens, including SARS-CoV-2. SARS-CoV-2 entry results in the release of pro-inflammatory cytokines and chemical mediators to create a “cytokine storm”. Endothelial cell (EC) dysfunction and cell-mediated injury are also present. These factors cause an exacerbated inflammatory state. During HIV infection and PE, various complement components are elevated, causing a hyper-inflammatory state. Furthermore, EC dysfunction and cell-mediated injury are also present. The similarities in pathological aspects of these three disorders may emanate from excessive complement activation. This review serves as a platform for further research on the complement system, coronavirus disease 2019, HIV infection and PE.
Keyword
Figure
Reference
-
References
1. Merle NS, Church SE, Fremeaux-Bacchi V, Roumenina LT. Complement system part I - molecular mechanisms of activation and regulation. Front Immunol. 2015; 6:262.
Article2. Lokki AI, Heikkinen-Eloranta J, Jarva H, Saisto T, Lokki ML, Laivuori H, et al. Complement activation and regulation in preeclamptic placenta. Front Immunol. 2014; 5:312.
Article3. Unaids. Global HIV & AIDS statistics-2020 fact sheet [Internet]. Washington, DC: UNAIDS;c2020. [cited 2022 May 1]. Available from: https://www.unaids.org/en/resources/fact-sheet.4. Maartens G, Celum C, Lewin SR. HIV infection: epidemiology, pathogenesis, treatment, and prevention. Lancet. 2014; 384:258–71.
Article5. Kalumba VM, Moodley J, Naidoo TD. Is the prevalence of pre-eclampsia affected by HIV/AIDS? A retrospective case-control study. Cardiovasc J Afr. 2013; 24:24–7.6. Rodriguez-Morales AJ, Bonilla-Aldana DK, Balbin-Ramon GJ, Rabaan AA, Sah R, Paniz-Mondolfi A, et al. History is repeating itself: probable zoonotic spillover as the cause of the 2019 novel coronavirus epidemic. Infez Med. 2020; 28:3–5.7. Pal M, Berhanu G, Desalegn C, Kandi V. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): an update. Cureus. 2020; 12:e7423.
Article8. Gavriilaki E, Brodsky RA. Severe COVID-19 infection and thrombotic microangiopathy: success does not come easily. Br J Haematol. 2020; 189:e227–30.
Article9. Java A, Apicelli AJ, Liszewski MK, Coler-Reilly A, Atkinson JP, Kim AH, et al. The complement system in COVID-19: friend and foe? JCI Insight. 2020; 5:e140711.
Article10. Risitano AM, Mastellos DC, Huber-Lang M, Yancopoulou D, Garlanda C, Ciceri F, et al. Complement as a target in COVID-19? Nat Rev Immunol. 2020; 20:343–4.
Article11. Vitiello A, La Porta R, D’Aiuto V, Ferrara F. Pharmacological approach for the reduction of inflammatory and prothrombotic hyperactive state in COVID-19 positive patients by acting on complement cascade. Hum Immunol. 2021; 82:264–9.
Article12. Gathiram P, Moodley J. Pre-eclampsia: its pathogenesis and pathophysiolgy. Cardiovasc J Afr. 2016; 27:71–8.
Article13. He YD, Xu BN, Song D, Wang YQ, Yu F, Chen Q, et al. Normal range of complement components during pregnancy: a prospective study. Am J Reprod Immunol. 2020; 83:e13202.
Article14. Shen B, Yi X, Sun Y, Bi X, Du J, Zhang C, et al. Proteomic and metabolomic characterization of COVID-19 patient sera. Cell. 2020; 182:59–72.e15.
Article15. Clarke W, Marzinke M. Contemporary practice in clinical chemistry. 4th ed.Baltimore: Academic Press;2020.16. Noris M, Remuzzi G. Overview of complement activation and regulation. Semin Nephrol. 2013; 33:479–92.
Article17. McDonald CR, Tran V, Kain KC. Complement activation in placental malaria. Front Microbiol. 2015; 6:1460.
Article18. Regal JF, Gilbert JS, Burwick RM. The complement system and adverse pregnancy outcomes. Mol Immunol. 2015; 67:56–70.
Article19. Conroy AL, McDonald CR, Gamble JL, Olwoch P, Natureeba P, Cohan D, et al. Altered angiogenesis as a common mechanism underlying preterm birth, small for gestational age, and stillbirth in women living with HIV. Am J Obstet Gynecol. 2017; 217:684.e1–684.e17.
Article20. Schmidt CQ, Lambris JD, Ricklin D. Protection of host cells by complement regulators. Immunol Rev. 2016; 274:152–71.
Article21. Beltrame MH, Catarino SJ, Goeldner I, Boldt AB, de Messias-Reason IJ. The lectin pathway of complement and rheumatic heart disease. Front Pediatr. 2015; 2:148.
Article22. Wang W, Xie X, Yuan T, Wang Y, Zhao F, Zhou Z, et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: a population-based study. BMC Pregnancy Childbirth. 2021; 21:364.
Article23. Collier AY, Molina RL. Maternal mortality in the United States: updates on trends, causes, and solutions. Neoreviews. 2019; 20:e561–74.
Article24. Rana S, Lemoine E, Granger JP, Karumanchi SA. Preeclampsia: pathophysiology, challenges, and perspectives. Circ Res. 2019; 124:1094–112.25. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018; 72:24–43.26. Phipps E, Prasanna D, Brima W, Jim B. Preeclampsia: updates in pathogenesis, definitions, and guidelines. Clin J Am Soc Nephrol. 2016; 11:1102–13.
Article27. Staff AC, Benton SJ, von Dadelszen P, Roberts JM, Taylor RN, Powers RW, et al. Redefining preeclampsia using placenta-derived biomarkers. Hypertension. 2013; 61:932–42.
Article28. McNally R, Alqudah A, Obradovic D, McClements L. Elucidating the pathogenesis of pre-eclampsia using in vitro models of spiral uterine artery remodelling. Curr Hypertens Rep. 2017; 19:93.
Article29. Li H, Ohta H, Tahara Y, Nakamura S, Taguchi K, Nakagawa M, et al. Artificial oxygen carriers rescue placental hypoxia and improve fetal development in the rat pre-eclampsia model. Sci Rep. 2015; 5:15271.
Article30. Tomimatsu T, Mimura K, Endo M, Kumasawa K, Kimura T. Pathophysiology of preeclampsia: an angiogenic imbalance and long-lasting systemic vascular dysfunction. Hypertens Res. 2017; 40:305–10.
Article31. Stats SA. Mid-year population estimates 2021 [Internet]. Pretoria: Stats SA;c2021. [cited 2022 Dec 12]. Available from: http://www.statssa.gov.za/publications/P0302/Mid%20year%20estimates%202021_presentation.pdf.32. Reshi P, Lone IM. Human immunodeficiency virus and pregnancy. Arch Gynecol Obstet. 2010; 281:781–92.
Article33. Siegfried N, van der Merwe L, Brocklehurst P, Sint TT. Antiretrovirals for reducing the risk of mother-to-child transmission of HIV infection. Cochrane Database Syst Rev. 2011; CD003510.
Article34. Fourie C, van Rooyen J, Pieters M, Conradie K, Hoekstra T, Schutte A. Is HIV-1 infection associated with endothelial dysfunction in a population of African ancestry in South Africa? Cardiovasc J Afr. 2011; 22:134–40.
Article35. Govender N, Naicker T, Moodley J. Maternal imbalance between pro-angiogenic and anti-angiogenic factors in HIV-infected women with pre-eclampsia. Cardiovasc J Afr. 2013; 24:174–9.36. Landi B, Bezzeccheri V, Guerra B, Piemontese M, Cervi F, Cecchi L, et al. HIV infection in pregnancy and the risk of gestational hypertension and preeclampsia. WJCD. 2014; 4:11.37. Kline ER, Sutliff RL. The roles of HIV-1 proteins and antiretroviral drug therapy in HIV-1-associated endothelial dysfunction. J Investig Med. 2008; 56:752–69.
Article38. World Health Organization. WHO coronavirus (COVID-19) dashboard [Internet]. Geneva: World Health Organization;c2023. [cited 2023 Aug 3]. Available from: https://covid19.who.int/.39. Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, et al. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ Res. 2020; 126:1456–74.
Article40. Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020; 94:e00127–20.
Article41. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020; 324:782–93.
Article42. Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health. 2020; 13:667–73.
Article43. Goel H, Gupta I, Mourya M, Gill S, Chopra A, Ranjan A, et al. A systematic review of clinical and laboratory parameters of 3,000 COVID-19 cases. Obstet Gynecol Sci. 2021; 64:174–89.
Article44. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–20.
Article45. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020; 46:846–8.
Article46. Huang S, Tian J, Liu C, Long Y, Cao D, Wei L, et al. Elevated C-reactive protein and complement C3 levels are associated with preterm birth: a nested case-control study in Chinese women. BMC Pregnancy Childbirth. 2020; 20:131.
Article47. Vardhana SA, Wolchok JD. The many faces of the anti-COVID immune response. J Exp Med. 2020; 217:e20200678.
Article48. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506.
Article49. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020; 395:1417–8.
Article50. Bryce C, Grimes Z, Pujadas E, Ahuja S, Beasley MB, Albrecht R, et al. Pathophysiology of SARS-CoV-2: targeting of endothelial cells renders a complex disease with thrombotic microangiopathy and aberrant immune response. The mount sinai COVID-19 autopsy experience. MedRxiv. 2020; May. 22. [Epub]. https://doi.org/10.1038/s41379-021-00793-y.
Article51. Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020; 98:219–27.
Article52. Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020; 220:1–13.
Article53. Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020; 18:1738–42.
Article54. Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020; 190:62.
Article55. Chatterjee P, Nagi N, Agarwal A, Das B, Banerjee S, Sarkar S, et al. The 2019 novel coronavirus disease (COVID-19) pandemic: a review of the current evidence. Indian J Med Res. 2020; 151:147–59.
Article56. Wastnedge EAN, Reynolds RM, van Boeckel SR, Stock SJ, Denison FC, Maybin JA, et al. Pregnancy and COVID-19. Physiol Rev. 2021; 101:303–18.
Article57. Enninga EA, Nevala WK, Creedon DJ, Markovic SN, Holtan SG. Fetal sex-based differences in maternal hormones, angiogenic factors, and immune mediators during pregnancy and the postpartum period. Am J Reprod Immuno. 2015; 73:251–62.
Article58. Mor G, Aldo P, Alvero AB. The unique immunological and microbial aspects of pregnancy. Nat Rev Immunol. 2017; 17:469–82.
Article59. Cugno M, Meroni PL, Gualtierotti R, Griffini S, Grovetti E, Torri A, et al. Complement activation in patients with COVID-19: a novel therapeutic target. J Allergy Clin Immunol. 2020; 146:215–7.60. Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, Martinez R, Bernstein K, et al. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020; 2:100118.
Article61. Mendoza M, Garcia-Ruiz I, Maiz N, Rodo C, Garcia-Manau P, Serrano B, et al. Pre-eclampsia-like syndrome induced by severe COVID-19: a prospective observational study. BJOG. 2020; 127:1374–80.
Article62. Shanes ED, Mithal LB, Otero S, Azad HA, Miller ES, Goldstein JA. Placental pathology in COVID-19. Am J Clin Pathol. 2020; 154:23–32.
Article63. Estrada-Chiroque LM, Orostegui-Arenas M, Burgos-Guanilo MDP, Amau-Chiroque JM. Clinical characteristics and maternal perinatal outcome in women with a confirmed diagnosis of COVID-19 in a hospital in Peru. Retrospective cohort study. Rev Colomb Obstet Ginecol. 2022; 73:28–38.
Article64. Coronado-Arroyo JC, Concepción-Zavaleta MJ, Zavaleta-Gutiérrez FE, Concepción-Urteaga LA. Is COVID-19 a risk factor for severe preeclampsia? Hospital experience in a developing country. Eur J Obstet Gynecol Reprod Biol. 2021; 256:502–3.
Article65. Todros T, Masturzo B, De Francia S. COVID-19 infection: ACE2, pregnancy and preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2020; 253:330.
Article66. Ahlberg M, Neovius M, Saltvedt S, Söderling J, Pettersson K, Brandkvist C, et al. Association of SARS-CoV-2 test status and pregnancy outcomes. JAMA. 2020; 324:1782–5.
Article67. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. Increased pregnancy problems with COVID-19-meta-analysis and letter to editor-April 2021. CMAJ. 2021; 193:E540–8.68. Brosnihan KB, Neves LA, Anton L, Joyner J, Valdes G, Merrill DC. Enhanced expression of ang-(1–7) during pregnancy. Braz J Med Biol Res. 2004; 37:1255–62.
Article69. West CA, Sasser JM, Baylis C. The enigma of continual plasma volume expansion in pregnancy: critical role of the renin-angiotensin-aldosterone system. Am J Physiol Renal Physiol. 2016; 311:F1125–34.
Article70. Merrill DC, Karoly M, Chen K, Ferrario CM, Brosnihan KB. Angiotensin-(1–7) in normal and preeclamptic pregnancy. Endocrine. 2002; 18:239–45.
Article71. Glowacka I, Bertram S, Herzog P, Pfefferle S, Steffen I, Muench MO, et al. Differential downregulation of ACE2 by the spike proteins of severe acute respiratory syndrome coronavirus and human coronavirus NL63. J Virol. 2010; 84:1198–205.
Article72. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191:145–7.
Article73. Inciardi RM, Solomon SD, Ridker PM, Metra M. Coronavirus 2019 disease (COVID-19), systemic inflammation, and cardiovascular disease. J Am Heart Assoc. 2020; 9:e017756.
Article74. Garovic VD, Hayman SR. Hypertension in pregnancy: an emerging risk factor for cardiovascular disease. Nat Clin Pract Nephrol. 2007; 3:613–22.
Article75. Alrahmani L, Willrich MAV. The complement alternative pathway and preeclampsia. Curr Hypertens Rep. 2018; 20:40.
Article76. Dusse LM, Rios DR, Pinheiro MB, Cooper AJ, Lwaleed BA. Pre-eclampsia: relationship between coagulation, fibrinolysis and inflammation. Clin Chim Acta. 2011; 412:17–21.
Article77. Kucukgoz Gulec U, Tuncay Ozgunen F, Baris Guzel A, Buyukkurt S, Seydaoglu G, Ferhat Urunsak I, et al. An analysis of C-reactive protein, procalcitonin, and D-dimer in pre-eclamptic patients. Am J Reprod Immunol. 2012; 68:331–7.
Article78. Bozkurt M, Yumru AE, Sahin L, Salman S. Troponin I and D-dimer levels in preeclampsia and eclampsia: prospective study. Clin Exp Obstet Gynecol. 2015; 42:26–31.
Article79. Gutiérrez García I, Pérez Cañadas P, Martínez Uriarte J, García Izquierdo O, Angeles Jódar Pérez M, García de Guadiana Romualdo L. D-dimer during pregnancy: establishing trimester-specific reference intervals. Scand J Clin Lab Invest. 2018; 78:439–42.
Article80. Posch W, Lass-Flörl C, Wilflingseder D. Innate immune responses in HIV-infection. Chang TL, editor. HIV-host interactions. 5th ed.Austria: InTechOpen;2011. p. 100–15.
Article81. Hladik F, McElrath MJ. Setting the stage: host invasion by HIV. Nat Rev Immunol. 2008; 8:447–57.
Article82. de Jong MA, Geijtenbeek TB. Langerhans cells in innate defense against pathogens. Trends Immunol. 2010; 31:452–9.
Article83. Roberts L, Passmore JA, Williamson C, Little F, Bebell LM, Mlisana K, et al. Plasma cytokine levels during acute HIV-1 infection predict HIV disease progression. AIDS. 2010; 24:819–31.
Article84. Ricklin D, Lambris JD. Complement in immune and inflammatory disorders: pathophysiological mechanisms. J Immunol. 2013; 190:3831–8.
Article85. Alqudah MA, Yaseen MM, Yaseen MM. HIV-1 strategies to overcome the immune system by evading and invading innate immune system. HIV AIDS Rev. 2016; 15:1–12.
Article86. Popko K, Gorska E, Stelmaszczyk-Emmel A, Plywaczewski R, Stoklosa A, Gorecka D, et al. Proinflammatory cytokines Il-6 and TNF-α and the development of inflammation in obese subjects. Eur J Med Res. 2010; 15(Suppl 2):120–2.
Article87. Pierik E, Prins JR, van Goor H, Dekker GA, Daha MR, Seelen MAJ, et al. Dysregulation of complement activation and placental dysfunction: a potential target to treat preeclampsia? Front Immunol. 2020; 10:3098.
Article88. Hsu P, Nanan RK. Innate and adaptive immune interactions at the fetal-maternal interface in healthy human pregnancy and pre-eclampsia. Front Immunol. 2014; 5:125.
Article89. Perez-Sepulveda A, Torres MJ, Khoury M, Illanes SE. Innate immune system and preeclampsia. Front Immunol. 2014; 5:224.
Article90. Ito Y, Matsuoka K, Uesato T, Sago H, Okamoto A, Nakazawa A, et al. Increased expression of perforin, granzyme B, and C5b-9 in villitis of unknown etiology. Placenta. 2015; 36:531–7.
Article91. Banadakoppa M, Balakrishnan M, Yallampalli C. Upregulation and release of soluble fms-like tyrosine kinase receptor 1 mediated by complement activation in human syncytiotrophoblast cells. Am J Reprod Immunol. 2018; 80:e13033.
Article92. Denny KJ, Coulthard LG, Finnell RH, Callaway LK, Taylor SM, Woodruff TM. Elevated complement factor C5a in maternal and umbilical cord plasma in preeclampsia. J Reprod Immunol. 2013; 97:211–6.
Article93. Rampersad R, Barton A, Sadovsky Y, Nelson DM. The C5b-9 membrane attack complex of complement activation localizes to villous trophoblast injury in vivo and modulates human trophoblast function in vitro. Placenta. 2008; 29:855–61.
Article94. Wadhwani P, Saha PK, Kalra JK, Gainder S, Sundaram V. A study to compare maternal and perinatal outcome in early vs. late onset preeclampsia. Obstet Gynecol Sci. 2020; 63:207–7.
Article95. Morgan BP. The membrane attack complex as an inflammatory trigger. Immunobiology. 2016; 221:747–51.
Article96. Derzsy Z, Prohászka Z, Rigó J Jr, Füst G, Molvarec A. Activation of the complement system in normal pregnancy and preeclampsia. Mol Immunol. 2010; 47:1500–6.
Article97. Girardi G. Complement activation, a threat to pregnancy. Semin Immunopathol. 2018; 40:103–11.
Article98. Regal JF, Burwick RM, Fleming SD. The complement system and preeclampsia. Curr Hypertens Rep. 2017; 19:87.
Article99. Gilbert JS, Banek CT, Katz VL, Babcock SA, Regal JF. Complement activation in pregnancy: too much of a good thing? Hypertension. 2012; 60:1114–6.
Article100. Yonekura Collier AR, Zsengeller Z, Pernicone E, Salahuddin S, Khankin EV, Karumanchi SA. Placental sFLT1 is associated with complement activation and syncytiotrophoblast damage in preeclampsia. Hypertens Pregnancy. 2019; 38:193–9.
Article101. Lynch AM, Salmon JE. Dysregulated complement activation as a common pathway of injury in preeclampsia and other pregnancy complications. Placenta. 2010; 31:561–7.
Article102. Burwick RM, Feinberg BB. Complement activation and regulation in preeclampsia and hemolysis, elevated liver enzymes, and low platelet count syndrome. Am J Obstet Gynecol. 2022; 226:S1059–70.
Article103. Girardi G, Yarilin D, Thurman JM, Holers VM, Salmon JE. Complement activation induces dysregulation of angiogenic factors and causes fetal rejection and growth restriction. J Exp Med. 2006; 203:2165–75.
Article104. Valencia CM, Burwick R, Velásquez JA, Silva JL, Gutiérrez-Marín J, Edna-Estrada F, et al. 67: improved diagnosis of preeclampsia with severe features and end organ injury using complement activation measurement in urine and plasma. Am J Obstet Gynecol. 2018; 218:S49–50.
Article105. Lynch AM, Wagner BD, Deterding RR, Giclas PC, Gibbs RS, Janoff EN, et al. The relationship of circulating proteins in early pregnancy with preterm birth. Am J Obstet Gynecol. 2016; 214:517.e1–517.e8.
Article106. Gralinski LE, Sheahan TP, Morrison TE, Menachery VD, Jensen K, Leist SR, et al. Complement activation contributes to severe acute respiratory syndrome coronavirus pathogenesis. mBio. 2018; 9:e01753–18.
Article107. Gao T, Hu M, Zhang X, Li H, Zhu L, Liu H, et al. Highly pathogenic coronavirus N protein aggravates lung injury by MASP-2-mediated complement over-activation. MedRxiv. 2020; Jun. 18. [Epub]. https://doi.org/10.1038/s41392-022-01133-5.
Article108. Rambaldi A, Gritti G, Micò MC, Frigeni M, Borleri G, Salvi A, et al. Endothelial injury and thrombotic microangiopathy in COVID-19: treatment with the lectin-pathway inhibitor narsoplimab. Immunobiology. 2020; 225:152001.
Article109. Li Y, Wang Y, Liu H, Sun W, Ding B, Zhao Y, et al. Urine proteome of COVID-19 patients. Urine (Amst). 2020; 2:1–8.
Article110. Diao B, Wang C, Wang R, Feng Z, Zhang J, Yang H, et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 infection. Nat Commun. 2021; 12:2506.
Article111. Magro G. Cytokine storm: is it the only major death factor in COVID-19 patients? Coagulation role. Med Hypotheses. 2020; 142:109829.
Article112. Ramlall V, Thangaraj PM, Meydan C, Foox J, Butler D, May B, et al. Identification of immune complement function as a determinant of adverse SARS-CoV-2 infection outcome. medRxiv. 2020. Jun. 6. [Epub]. https://doi.org/10.1101/2020.05.05.20092452.
Article113. Liszewski MK, Java A, Schramm EC, Atkinson JP. Complement dysregulation and disease: insights from contemporary genetics. Annu Rev Pathol. 2017; 12:25–52.
Article114. Ghai R, Waters P, Roumenina LT, Gadjeva M, Kojouharova MS, Reid KB, et al. C1q and its growing family. Immunobiology. 2007; 212:253–66.
Article115. Madhukaran SP, Alhamlan FS, Kale K, Vatish M, Madan T, Kishore U. Role of collectins and complement protein C1q in pregnancy and parturition. Immunobiology. 2016; 221:1273–88.
Article116. Clarke EV, Weist BM, Walsh CM, Tenner AJ. Complement protein C1q bound to apoptotic cells suppresses human macrophage and dendritic cell-mediated Th17 and Th1 T cell subset proliferation. J Leukoc Biol. 2015; 97:147–60.
Article117. Hoffmann M, Kleine-Weber H, Pöhlmann S. A multibasic cleavage site in the spike protein of SARS-CoV-2 is essential for infection of human lung cells. Mol Cell. 2020; 78:779–84.e5.
Article118. Yang W, Wang L, Tian T, Liu L, Jin L, Liu J, et al. Maternal hypertensive disorders in pregnancy and risk of hypoxic-ischemia encephalopathy. J Matern Fetal Neonatal Med. 2021; 34:1754–62.
Article119. Weetman AP. Immunity, thyroid function and pregnancy: molecular mechanisms. Nat Rev Endocrinol. 2010; 6:311–8.
Article120. Pazos M, Sperling RS, Moran TM, Kraus TA. The influence of pregnancy on systemic immunity. Immunol Res. 2012; 54:254–61.
Article121. Picone O, Bouthry E, Bejaoui-Olhmann Y, Cordier AG, Nedellec S, Letourneau A, et al. Determination of rubella virus-specific humoral and cell-mediated immunity in pregnant women with negative or equivocal rubella-specific IgG in routine screening. J Clin Virol. 2019; 112:27–33.
Article122. Lokki AI, Heikkinen-Eloranta JK, Laivuori H. The immunogenetic conundrum of preeclampsia. Front Immunol. 2018; 9:2630.
Article123. Teirilä L, Heikkinen-Eloranta J, Kotimaa J, Meri S, Lokki AI. Regulation of the complement system and immunological tolerance in pregnancy. Semin Immunol. 2019; 45:101337.
Article124. Tsafaras GP, Ntontsi P, Xanthou G. Advantages and limitations of the neonatal immune system. Front Pediatr. 2020; 8:5.
Article125. Ferrer-Oliveras R, Mendoza M, Capote S, Pratcorona L, Esteve-Valverde E, Cabero-Roura L, et al. Immunological and physiopathological approach of COVID-19 in pregnancy. Arch Gynecol Obstet. 2021; 304:39–57.
Article126. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395:507–13.
Article127. Muyayalo KP, Huang DH, Zhao SJ, Xie T, Mor G, Liao AH. COVID-19 and Treg/Th17 imbalance: potential relationship to pregnancy outcomes. Am J Reprod Immunol. 2020; 84:e13304.
Article128. Yu Q, Yu R, Qin X. The good and evil of complement activation in HIV-1 infection. Cell Mol Immunol. 2010; 7:334–40.
Article129. Burwick RM, Fichorova RN, Dawood HY, Yamamoto HS, Feinberg BB. Urinary excretion of C5b-9 in severe preeclampsia: tipping the balance of complement activation in pregnancy. Hypertension. 2013; 62:1040–5.130. Pillay Y, Moodley J, Naicker T. The role of the complement system in HIV infection and preeclampsia. Inflamm Res. 2019; 68:459–69.
Article131. Eisen S, Dzwonek A, Klein NJ. Mannose-binding lectin in HIV infection. Future Virol. 2008; 3:225–33.
Article132. Kacani L, Bánki Z, Zwirner J, Schennach H, Bajtay Z, Erdei A, et al. C5a and C5a(desArg) enhance the susceptibility of monocyte-derived macrophages to HIV infection. J Immunol. 2001; 166:3410–5.
Article133. Naicker T, Govender N, Abel T, Naidoo N, Moodley M, Pillay Y, et al. HIV associated preeclampsia: a multifactorial appraisal. Int J Mol Sci. 2021; 22:9157.
Article134. Lannaman K, Romero R, Chaiworapongsa T, Kim YM, Korzeniewski SJ, Maymon E, et al. Fetal death: an extreme manifestation of maternal anti-fetal rejection. J Perinat Med. 2017; 45:851–68.
Article135. Bulla R, Bossi F, Tedesco F. The complement system at the embryo implantation site: friend or foe? Front Immunol. 2012; 3:55.
Article136. Singh J, Ahmed A, Girardi G. Role of complement component C1q in the onset of preeclampsia in mice. Hypertension. 2011; 58:716–24.
Article137. Lynch AM, Gibbs RS, Murphy JR, Byers T, Neville MC, Giclas PC, et al. Complement activation fragment Bb in early pregnancy and spontaneous preterm birth. Am J Obstet Gynecol. 2008; 199:354.e1–8.
Article138. Burwick RM, Velásquez JA, Valencia CM, Gutiérrez-Marín J, Edna-Estrada F, Silva JL, et al. Terminal complement activation in preeclampsia. Obstet Gynecol. 2018; 132:1477–85.
Article139. Lillegard KE, Johnson AC, Lojovich SJ, Bauer AJ, Marsh HC, Gilbert JS, et al. Complement activation is critical for placental ischemia-induced hypertension in the rat. Mol Immunol. 2013; 56:91–7.
Article