J Korean Med Sci.
2023 Jun;38(23):e176. 10.3346/jkms.2023.38.e176.
Exercise Frequency Reduction Is Associated With Higher Risk of Infection in Newly Diagnosed Diabetes: A Nationally Representative Cohort Study
- Affiliations
-
- 1Department of Biomedical Informatics, CHA University School of Medicine, CHA University, Seongnam, Korea
- 2Institute of Biomedical Informatics, CHA University School of Medicine, CHA University, Seongnam, Korea
- 3Department of Biomedical Sciences, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2543868
- DOI: http://doi.org/10.3346/jkms.2023.38.e176
Abstract
- Background
Exercise is an important method to control the progression of diabetes. Since diabetes compromises immune function and increases the risk of infectious diseases, we hypothesized that exercise may affect the risk of infection by its immunoprotective effects. However, population-based cohort studies regarding the association between exercise and the risk of infection are limited, especially regarding changes in exercise frequency. The aim of this study was to determine the association between the change in exercise frequency and the risk of infection among patients with newly diagnosed diabetes.
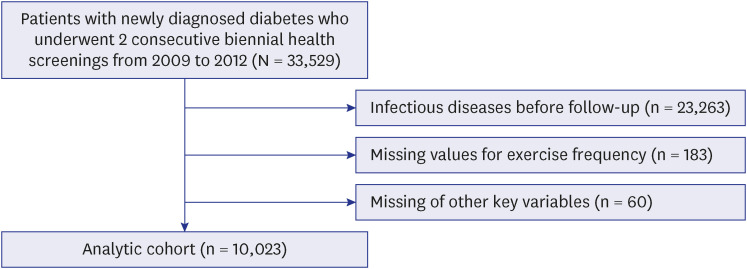
Methods
Data of 10,023 patients with newly diagnosed diabetes were extracted from the Korean National Health Insurance Service-Health Screening Cohort. Self-reported questionnaires for moderate-to-vigorous physical activity (MVPA) were used to classify changes in exercise frequency between two consecutive two-year periods of health screenings (2009–2010 and 2011–2012). The association between changes in exercise frequency and the risk of infection was evaluated using multivariable Cox proportional-hazards regression.
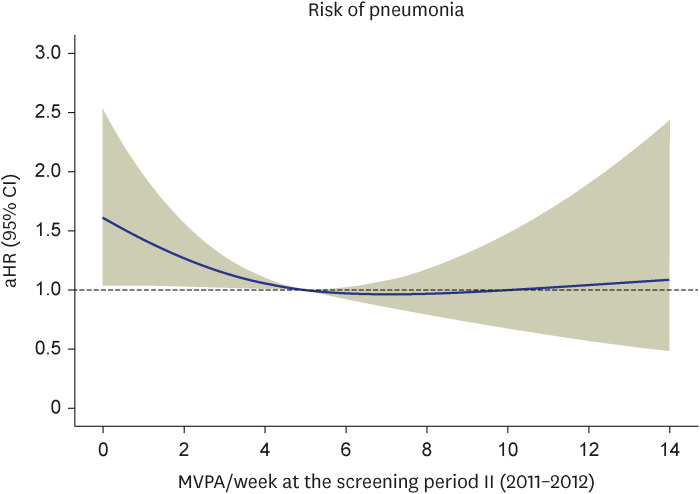
Results
Compared with engaging in ≥ 5 times of MVPA/week during both periods, a radical decrease in MVPA (from ≥ 5 times of MVPA/week to physical inactivity) was associated with a higher risk of pneumonia (adjusted hazard ratio [aHR], 1.60; 95% confidence interval [CI], 1.03–2.48) and upper respiratory tract infection (aHR, 1.15; 95% CI, 1.01–1.31). In addition, a reduction of MVPA from ≥ 5 to < 5 times of MVPA/week was associated with a higher risk of pneumonia (aHR, 1.52; 95% CI, 1.02–2.27), whereas the risk of upper respiratory tract infection was not higher.
Conclusion
Among patients with newly diagnosed diabetes, a reduction in exercise frequency was related to an increase in the risk of pneumonia. For patients with diabetes, a modest level of physical activity may need to be maintained to reduce the risk of pneumonia.
Keyword
Figure
Reference
-
1. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010; 87(1):4–14. PMID: 19896746.
Article2. Bae JH, Han KD, Ko SH, Yang YS, Choi JH, Choi KM, et al. Diabetes fact sheet in Korea 2021. Diabetes Metab J. 2022; 46(3):417–426. PMID: 35656565.
Article3. Lee Y, Lim H, Park S. Characteristics of non-obese diabetes in Korean population. Public Health Wkly Rep. 2017; 10(30):780–787.4. Kwon H, Kim W, Lee D, Park S. Current status and need for a Korean diabetes prevention study. Public Health Wkly Rep. 2015; 8:746–753.5. American Diabetes Association. 5. Lifestyle management: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019; 42(Suppl 1):S46–S60. PMID: 30559231.6. Shin WY, Lee T, Jeon DH, Kim HC. Diabetes, frequency of exercise, and mortality over 12 years: analysis of the National Health Insurance Service-Health Screening (NHIS-HEALS) database. J Korean Med Sci. 2018; 33(8):e60. PMID: 29441753.
Article7. Kim EJ, Ha KH, Kim DJ, Choi YH. Diabetes and the risk of infection: a national cohort study. Diabetes Metab J. 2019; 43(6):804–814. PMID: 31701687.
Article8. Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab. 2012; 16:Suppl 1. (Suppl1):S27–S36. PMID: 22701840.9. Seo JA. The Effects of Diabetes on Risk of Infection. J Korean Diabetes. 2017; 18(1):14–19.
Article10. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007; 335(7624):806–808. PMID: 17947786.
Article11. Jeong HG, Kim DY, Kang DW, Kim BJ, Kim CK, Kim Y, et al. Physical activity frequency and the risk of stroke: a nationwide cohort study in Korea. J Am Heart Assoc. 2017; 6(9):e005671. PMID: 28855168.
Article12. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID: 16224307.
Article13. Kunutsor SK, Seidu S, Laukkanen JA. Physical activity reduces the risk of pneumonia: systematic review and meta-analysis of 10 prospective studies involving 1,044,492 participants. Geroscience. 2022; 44(1):519–532. PMID: 34822066.
Article14. Barrett B, Hayney MS, Muller D, Rakel D, Ward A, Obasi CN, et al. Meditation or exercise for preventing acute respiratory infection: a randomized controlled trial. Ann Fam Med. 2012; 10(4):337–346. PMID: 22778122.
Article15. Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q, et al. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021; 55(19):1099–1105. PMID: 33849909.
Article16. Leveille SG, Gray S, LaCroix AZ, Ferrucci L, Black DJ, Guralnik JM. Physical inactivity and smoking increase risk for serious infections in older women. J Am Geriatr Soc. 2000; 48(12):1582–1588. PMID: 11129746.
Article17. Hirata Y, Tomioka H, Sekiya R, Yamashita S, Kaneda T, Kida Y, et al. Association of hyperglycemia on admission and during hospitalization with mortality in diabetic patients admitted for pneumonia. Intern Med. 2013; 52(21):2431–2438. PMID: 24190147.
Article18. Burstein R, Polychronakos C, Toews CJ, MacDougall JD, Guyda HJ, Posner BI. Acute reversal of the enhanced insulin action in trained athletes. Association with insulin receptor changes. Diabetes. 1985; 34(8):756–760. PMID: 3894119.
Article19. Martins M, Boavida JM, Raposo JF, Froes F, Nunes B, Ribeiro RT, et al. Diabetes hinders community-acquired pneumonia outcomes in hospitalized patients. BMJ Open Diabetes Res Care. 2016; 4(1):e000181.
Article20. Nieman DC, Sakaguchi CA. Physical activity lowers the risk for acute respiratory infections: Time for recognition. J Sport Health Sci. 2022; 11(6):648–655. PMID: 35995362.
Article21. Williams PT. Dose-response relationship between exercise and respiratory disease mortality. Med Sci Sports Exerc. 2014; 46(4):711–717. PMID: 24002349.
Article22. Fondell E, Lagerros YT, Sundberg CJ, Lekander M, Bälter O, Rothman KJ, et al. Physical activity, stress, and self-reported upper respiratory tract infection. Med Sci Sports Exerc. 2011; 43(2):272–279. PMID: 20581713.
Article23. Jacobs DR Jr, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993; 25(1):81–91. PMID: 8423759.
Article24. Sylvia LG, Bernstein EE, Hubbard JL, Keating L, Anderson EJ. Practical guide to measuring physical activity. J Acad Nutr Diet. 2014; 114(2):199–208. PMID: 24290836.
Article25. Pujalte GG, Costa LM, Clapp AD, Presutti RJ, Sluzevich JC. More than skin deep: dermatologic conditions in athletes. Sports Health. 2023; 15(1):74–85. PMID: 35034516.
Article26. Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Health Sci. 2019; 8(3):201–217. PMID: 31193280.
Article27. Nieman DC. Exercise is medicine for immune function: implication for COVID-19. Curr Sports Med Rep. 2021; 20(8):395–401. PMID: 34357885.
Article28. Alibegovic AC, Højbjerre L, Sonne MP, van Hall G, Stallknecht B, Dela F, et al. Impact of 9 days of bed rest on hepatic and peripheral insulin action, insulin secretion, and whole-body lipolysis in healthy young male offspring of patients with type 2 diabetes. Diabetes. 2009; 58(12):2749–2756. PMID: 19720789.
Article29. Hoff P, Belavý DL, Huscher D, Lang A, Hahne M, Kuhlmey AK, et al. Effects of 60-day bed rest with and without exercise on cellular and humoral immunological parameters. Cell Mol Immunol. 2015; 12(4):483–492. PMID: 25382740.
Article30. Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012; 2(2):1143–1211. PMID: 23798298.
Article31. Murphy EA, Davis JM, Carmichael MD, Gangemi JD, Ghaffar A, Mayer EP. Exercise stress increases susceptibility to influenza infection. Brain Behav Immun. 2008; 22(8):1152–1155. PMID: 18616997.
Article32. Kim EA. Social distancing and public health guidelines at workplaces in Korea: responses to coronavirus disease-19. Saf Health Work. 2020; 11(3):275–283. PMID: 32837740.
Article33. Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. 2014; 383(9911):69–82. PMID: 23890997.
Article34. Song SO, Song YD, Nam JY, Park KH, Yoon JH, Son KM, et al. Epidemiology of type 1 diabetes mellitus in Korea through an investigation of the national registration project of type 1 diabetes for the reimbursement of glucometer strips with additional analyses using claims data. Diabetes Metab J. 2016; 40(1):35–45. PMID: 26912154.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk for Newly Diagnosed Type 2 Diabetes Mellitus after COVID-19 among Korean Adults: A Nationwide Matched Cohort Study
- Comparison of New-Onset Diabetes Mellitus among Patients with Atrial Fibrillation or Atrial Flutter
- Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
- Maintaining Physical Activity Is Associated with Reduced Major Adverse Cardiovascular Events in People Newly Diagnosed with Diabetes
- Diabetes, Frequency of Exercise, and Mortality Over 12 Years: Analysis of the National Health Insurance Service-Health Screening (NHIS-HEALS) Database