Anesth Pain Med.
2023 Apr;18(2):148-158. 10.17085/apm.22240.
Effect of sevoflurane-remifentanil and propofol-remifentanil anesthesia on glycocalyx shedding during deep inferior epigastric perforator flap breast reconstruction: a prospective randomized, controlled trial
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea
- 2Biostatistics Collaboration Unit, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2543656
- DOI: http://doi.org/10.17085/apm.22240
Abstract
- Background
The endothelial glycocalyx (EG) is an important structure that regulates vascular homeostasis. Deep inferior epigastric perforator (DIEP) flap is expected to cause substantial EG breakdown owing to the long procedural duration and ischemia– reperfusion injury. This prospective, randomized, controlled study aimed to compare syndecan-1 levels during sevoflurane-remifentanil and propofol-remifentanil anesthesia in patients who underwent DIEP flap breast reconstruction.
Methods
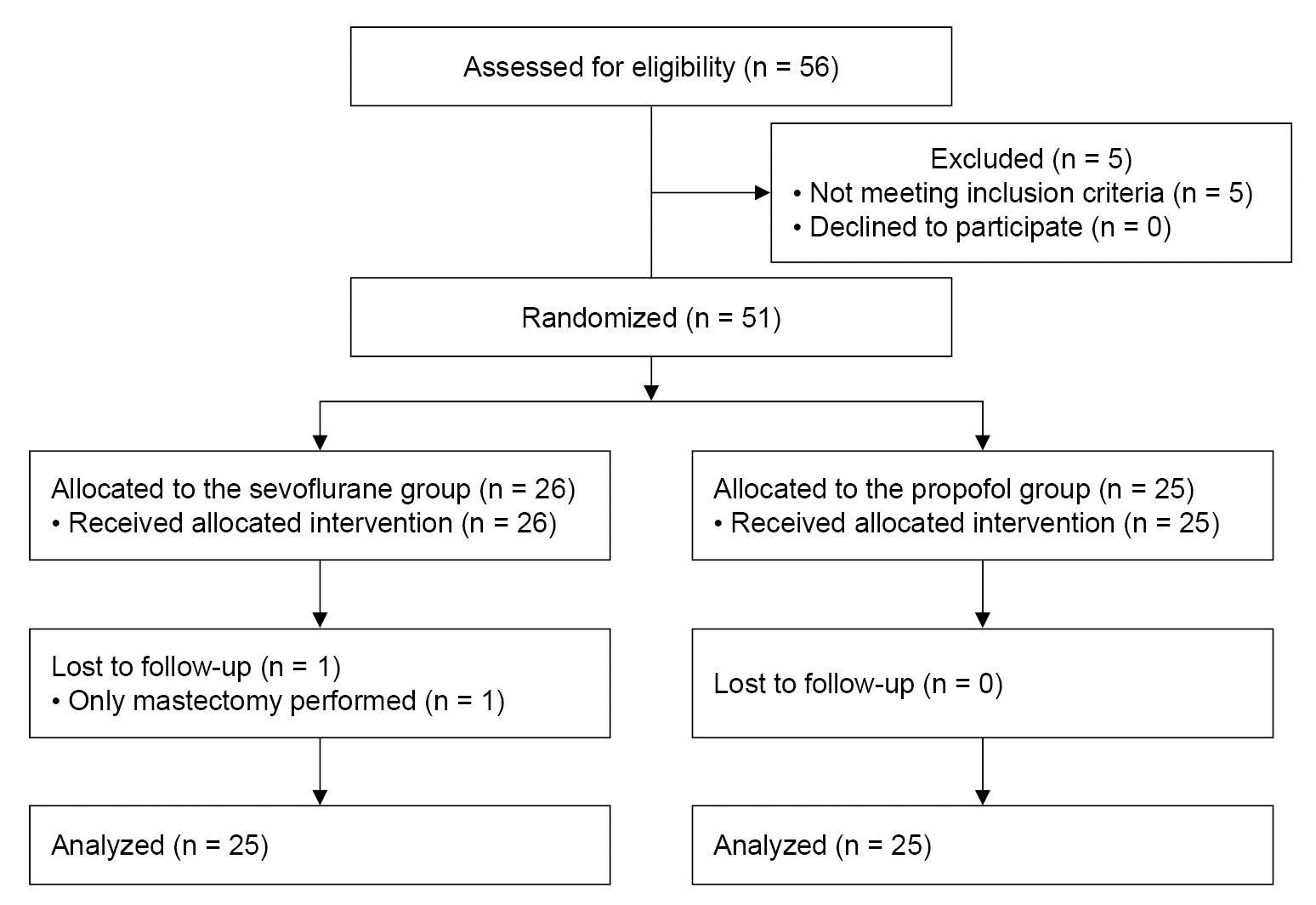
Fifty-one patients were randomized to either sevoflurane (n = 26) or propofol (n = 25) groups. Anesthesia was maintained with remifentanil in combination with either sevoflurane or propofol. The primary endpoint was the concentration of serum syndecan-1 measured at 1 h after surgery.
Results
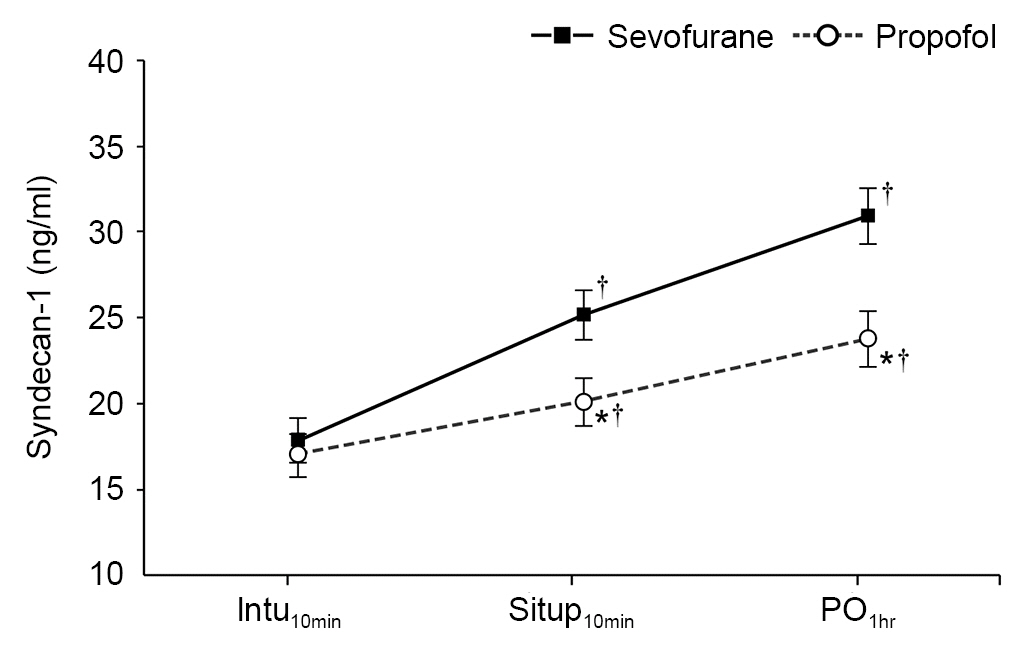
Fifty patients (98.0%) completed the study. Patients in the propofol group had significantly lower levels of syndecan-1 than patients in the sevoflurane group at 1 h after operation (23.8 ± 1.6 vs. 30.9 ± 1.7 ng/ml, respectively; Bonferroni corrected P = 0.012). There were no significant differences between groups in postoperative complications. The postoperative hospital stay was 8.4 ± 2.5 days in the sevoflurane group and 7.4 ± 1.0 days in the propofol group (P = 0.077).
Conclusions
Propofol-remifentanil anesthesia resulted in lesser increases in syndecan-1 levels compared to increases with sevoflurane-remifentanil anesthesia in patients who underwent DIEP flap reconstruction. Our results suggest that propofol-remifentanil anesthesia shows protective effects against EG damage during DIEP flap breast reconstruction in contrast to sevoflurane-remifentanil anesthesia.
Keyword
Figure
Reference
-
1. Reitsma S, Slaaf DW, Vink H, van Zandvoort MA, oude Egbrink MG. The endothelial glycocalyx: composition, functions, and visualization. Pflugers Arch. 2007; 454:345–59.
Article2. Alphonsus CS, Rodseth RN. The endothelial glycocalyx: a review of the vascular barrier. Anaesthesia. 2014; 69:777–84.
Article3. Kolářová H, Ambrůzová B, Svihálková Šindlerová L, Klinke A, Kubala L. Modulation of endothelial glycocalyx structure under inflammatory conditions. Mediators Inflamm. 2014; 2014:694312.
Article4. Gonzalez Rodriguez E, Ostrowski SR, Cardenas JC, Baer LA, Tomasek JS, Henriksen HH, et al. Syndecan-1: a quantitative marker for the endotheliopathy of trauma. J Am Coll Surg. 2017; 225:419–27.
Article5. Anand D, Ray S, Srivastava LM, Bhargava S. Evolution of serum hyaluronan and syndecan levels in prognosis of sepsis patients. Clin Biochem. 2016; 49:768–76.
Article6. Suzuki A, Tomita H, Okada H. Form follows function: the endothelial glycocalyx. Transl Res. 2022; 247:158–67.
Article7. Gill PS, Hunt JP, Guerra AB, Dellacroce FJ, Sullivan SK, Boraski J, et al. A 10-year retrospective review of 758 DIEP flaps for breast reconstruction. Plast Reconstr Surg. 2004; 113:1153–60.
Article8. Ireton JE, Lakhiani C, Saint-Cyr M. Vascular anatomy of the deep inferior epigastric artery perforator flap: a systematic review. Plast Reconstr Surg. 2014; 134:810e–821e.9. Selber JC, Nelson J, Fosnot J, Goldstein J, Bergey M, Sonnad SS, et al. A prospective study comparing the functional impact of SIEA, DIEP, and muscle-sparing free TRAM flaps on the abdominal wall: part I. unilateral reconstruction. Plast Reconstr Surg. 2010; 126:1142–53.
Article10. Nimalan N, Branford OA, Stocks G. Anaesthesia for free flap breast reconstruction. BJA Educ. 2016; 16:162–6.
Article11. Annecke T, Chappell D, Chen C, Jacob M, Welsch U, Sommerhoff CP, et al. Sevoflurane preserves the endothelial glycocalyx against ischaemia-reperfusion injury. Br J Anaesth. 2010; 104:414–21.
Article12. Chappell D, Heindl B, Jacob M, Annecke T, Chen C, Rehm M, et al. Sevoflurane reduces leukocyte and platelet adhesion after ischemia-reperfusion by protecting the endothelial glycocalyx. Anesthesiology. 2011; 115:483–91.
Article13. Kim HJ, Kim E, Baek SH, Kim HY, Kim JY, Park J, et al. Sevoflurane did not show better protective effect on endothelial glycocalyx layer compared to propofol during lung resection surgery with one lung ventilation. J Thorac Dis. 2018; 10:1468–75.
Article14. Maldonado F, Morales D, Gutiérrez R, Barahona M, Cerda O, Cáceres M. Effect of sevoflurane and propofol on tourniquet-induced endothelial damage: a pilot randomized controlled trial for knee-ligament surgery. BMC Anesthesiol. 2020; 20:121.
Article15. Oh CS, Choi JM, Park EH, Piao L, Park HJ, Rhee KY, et al. Impact of anesthetic agents on endothelial glycocalyx injury during total knee arthroplasty: desflurane- vs. propofol-based anesthesia-a prospective randomized controlled trial. Biomed Res Int. 2021; 2021:8880267.
Article16. Kim NY, Kim KJ, Lee KY, Shin HJ, Cho J, Nam DJ, et al. Effect of volatile and total intravenous anesthesia on syndecan-1 shedding after minimally invasive gastrectomy: a randomized trial. Sci Rep. 2021; 11:1511.
Article17. Prichep LS, Gugino LD, John ER, Chabot RJ, Howard B, Merkin H, et al. The Patient State Index as an indicator of the level of hypnosis under general anaesthesia. Br J Anaesth. 2004; 92:393–9.
Article18. Lee KH, Kim YH, Sung YJ, Oh MK. The Patient State Index is well balanced for propofol sedation. Hippokratia. 2015; 19:235–8.19. Steppan J, Hofer S, Funke B, Brenner T, Henrich M, Martin E, et al. Sepsis and major abdominal surgery lead to flaking of the endothelial glycocalix. J Surg Res. 2011; 165:136–41.
Article20. Rehm M, Bruegger D, Christ F, Conzen P, Thiel M, Jacob M, et al. Shedding of the endothelial glycocalyx in patients undergoing major vascular surgery with global and regional ischemia. Circulation. 2007; 116:1896–906.
Article21. Lie KH, Barker AS, Ashton MW. A classification system for partial and complete DIEP flap necrosis based on a review of 17,096 DIEP flaps in 693 articles including analysis of 152 total flap failures. Plast Reconstr Surg. 2013; 132:1401–8.
Article22. Depypere B, Herregods S, Denolf J, Kerkhove LP, Mainil L, Vyncke T, et al. 20 Years of DIEAP flap breast reconstruction: a big data analysis. Sci Rep 2019; 9: 12899. Erratum in: Sci Rep. 2020; 10:1398.23. Pattani KM, Byrne P, Boahene K, Richmon J. What makes a good flap go bad? A critical analysis of the literature of intraoperative factors related to free flap failure. Laryngoscope. 2010; 120:717–23.
Article24. Ibrahim AM, Kim PS, Rabie AN, Lee BT, Lin SJ. Vasopressors and reconstructive flap perfusion: a review of the literature comparing the effects of various pharmacologic agents. Ann Plast Surg. 2014; 73:245–8.25. Zhang JN, Ma Y, Wei XY, Liu KY, Wang H, Han H, et al. Remifentanil protects against lipopolysaccharide-induced inflammation through PARP-1/NF-κB signaling pathway. Mediators Inflamm. 2019; 2019:3013716.26. Al-Hashimi M, Scott SW, Thompson JP, Lambert DG. Opioids and immune modulation: more questions than answers. Br J Anaesth. 2013; 111:80–8.
Article27. Sacerdote P, Gaspani L, Rossoni G, Panerai AE, Bianchi M. Effect of the opioid remifentanil on cellular immune response in the rat. Int Immunopharmacol. 2001; 1:713–9.
Article28. Zongze Z, Jia Z, Chang C, Kai C, Yanlin W. Protective effects of remifentanil on septic mice. Mol Biol Rep. 2010; 37:2803–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Remifentanil-Propofol and Remifentanil-Sevoflurane Anesthesia for Pediatric Tonsillectomy
- A Comparative Study of the RecoveryCharacteristics for the Use of Propofol-Remifentanil Anesthesia or Sevoflurane-Remifentanil Anesthesia under Bispectral Index Guidance
- Comparison of Total Intravenous Anesthesia and Sevoflurane-Alfentanil Anesthesia for Laparoscopic Cholecystectomy
- Effects of remifentanil on emergence characteristics from anesthesia in cervical spine surgery: a comparison of remifentanil- and sevoflurane-based anesthesia
- Effects of propofol-remifentanil versus sevoflurane-remifentanil on acute postoperative pain after total shoulder arthroplasty: a randomized trial