J Korean Neurosurg Soc.
2023 Jul;66(4):438-445. 10.3340/jkns.2022.0204.
The Optimal Time between Embolization and Surgery for Hypervascular Spinal Metastatic Tumors : A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Neurosurgery, Dongtan Sacred Heart Hospital, Hwaseong, Korea
- 3Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Medical Device Development, Seoul National University College of Medicine, Seoul, Korea
- 5Department of Brain and Cognitive Sciences, College of Natural Science, Seoul National University, Seoul, Korea
- KMID: 2543535
- DOI: http://doi.org/10.3340/jkns.2022.0204
Abstract
Objective
: Preoperative transarterial embolization (TAE) of tumor feeders in hypervascular spine metastasis is known to reduce intraoperative estimated blood loss (EBL) during surgery. The effect of TAE varies for several reasons, and one controllable factor is the timing between embolization and surgery. However, the adequate timing remains unclear. This study aimed to evaluate the timing and other factors that reduce EBL in spinal metastasis surgery through a meta-analysis.
Methods
: A comprehensive database search was performed to identify direct comparative studies of EBL stratified by the timing of surgery after TAE for spinal metastasis. EBL was analyzed according to the timing of surgery and other factors. Subgroup analyses were also performed. The difference in EBL was calculated as the mean difference (MD) and 95% confidence interval (CI).
Results
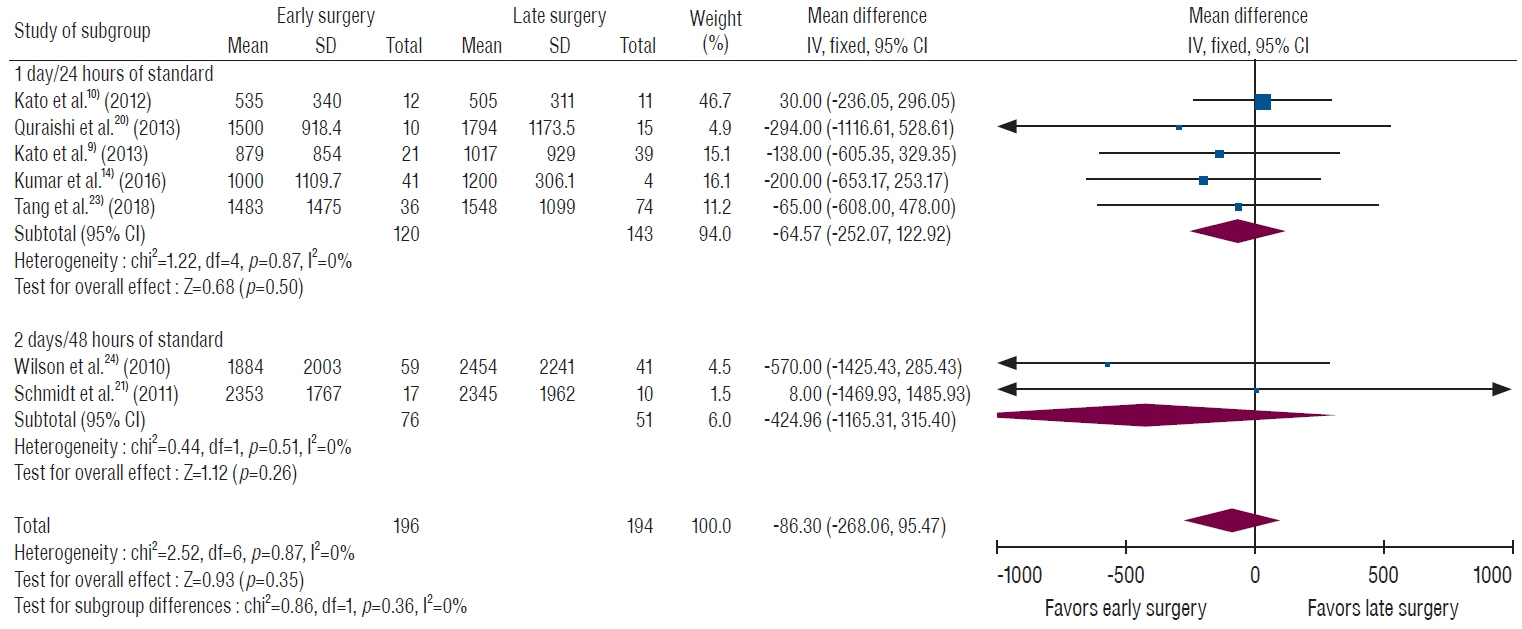
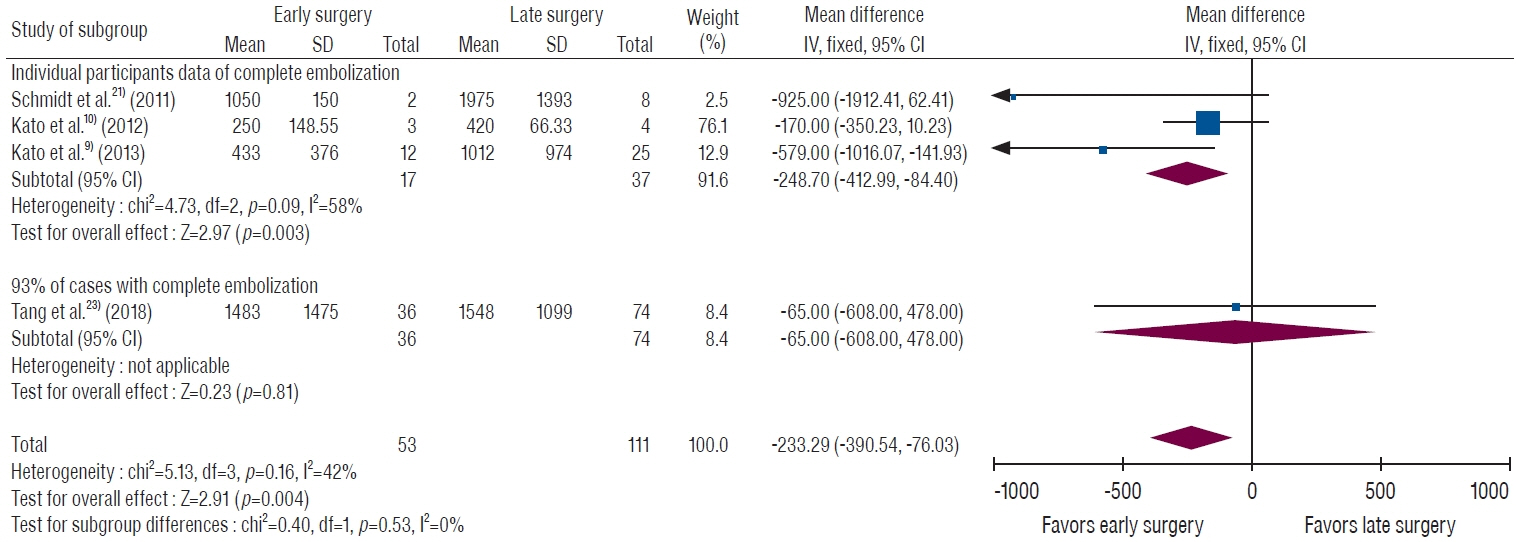
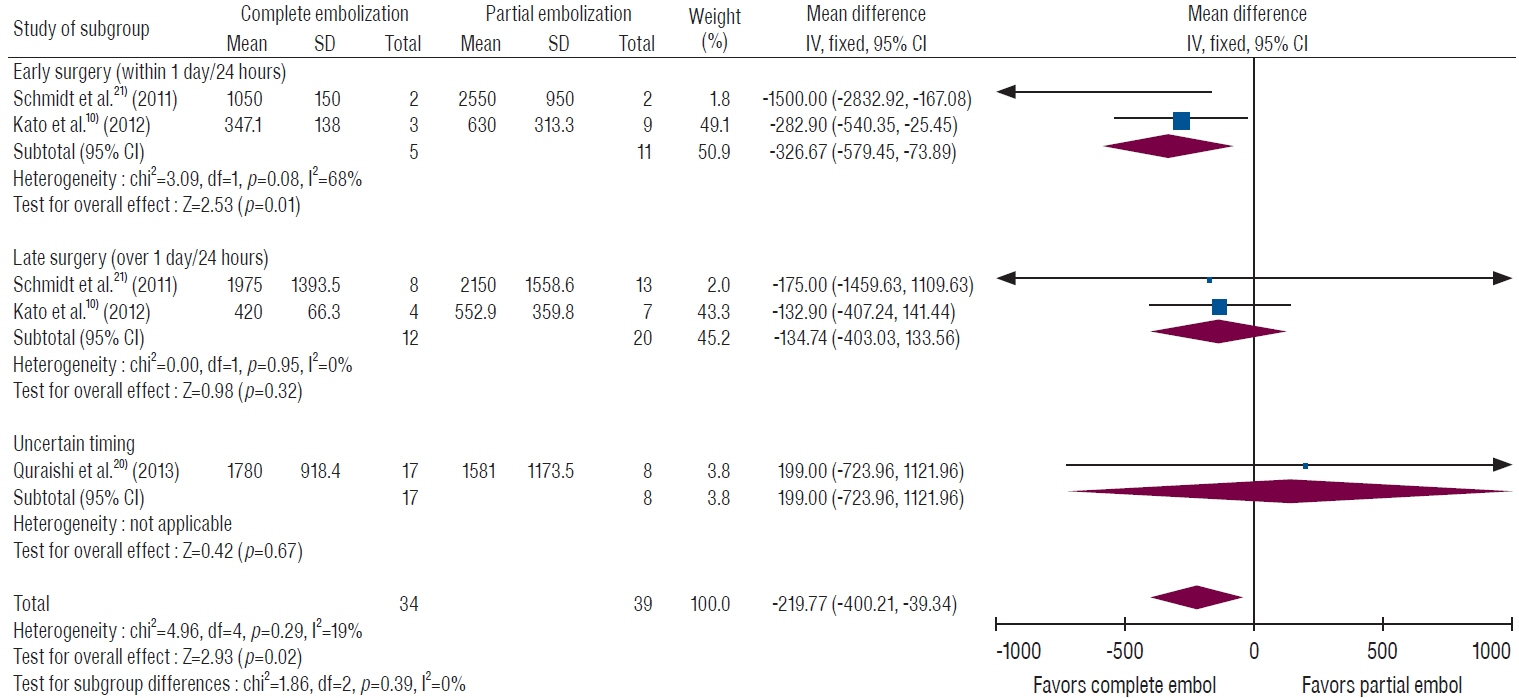
: Among seven studies, 196 and 194 patients underwent early and late surgery after TAE, respectively. The early surgery was defined as within 1–2 days after TAE, while the late surgery group received surgery at least 1 day after TAE. Overall, the MD in EBL was not different according to the timing of surgery (MD, 86.3 mL; 95% CI, -95.5 to 268.1 mL; p=0.35). A subgroup analysis of the complete embolization group demonstrated that patients who underwent early surgery within 24 hours after TAE had significantly less bleeding (MD, 233.3 mL; 95% CI, 76.0 to 390.5 mL; p=0.004). In cases of partial embolization, EBL was not significantly different regardless of the time interval.
Conclusion
: Complete embolization followed by early spinal surgery within 24 hours may reduce intraoperative bleeding for the patients with hypervascular spinal metastasis.
Figure
Reference
-
References
1. Clausen C, Dahl B, Frevert SC, Hansen LV, Nielsen MB, Lönn L. Preoperative embolization in surgical treatment of spinal metastases: singleblind, randomized controlled clinical trial of efficacy in decreasing intraoperative blood loss. J Vasc Interv Radiol. 26:402–412.e1. 2015.2. De la Garza Ramos R, Echt M, Benton JA, Gelfand Y, Longo M, Yanamadala V, et al. Accuracy of freehand versus navigated thoracolumbar pedicle screw placement in patients with metastatic tumors of the spine. J Korean Neurosurg Soc. 63:777–783. 2020.3. Feldman F, Casarella WJ, Dick HM, Hollander BA. Selective intra-arterial embolization of bone tumors. A useful adjunct in the management of selected lesions. Am J Roentgenol Radium Ther Nucl Med. 123:130–139. 1975.4. Gottfried ON, Schloesser PE, Schmidt MH, Stevens EA. Embolization of metastatic spinal tumors. Neurosurg Clin N Am. 15:391–399. 2004.
Article5. Griessenauer CJ, Salem M, Hendrix P, Foreman PM, Ogilvy CS, Thomas AJ. Preoperative embolization of spinal tumors: a systematic review and meta-analysis. World Neurosurg. 87:362–371. 2016.
Article6. He Z, Wong ST, Yam KY. Newly-Diagnosed, histologically-confirmed central nervous system tumours in a regional hospital in hong kong : an epidemiological study of a 21-year period. J Korean Neurosurg Soc. 63:119–135. 2020.
Article7. Heran MK. Preoperative embolization of spinal metastatic disease: rationale and technical considerations. Semin Musculoskelet Radiol. 15:135–142. 2011.
Article8. Hong JT, Kim IS, Lee HJ, Park JH, Hur JW, Lee JB, et al. Evaluation and surgical planning for craniovertebral junction deformity. Neurospine. 17:554–567. 2020.
Article9. Kato S, Hozumi T, Takaki Y, Yamakawa K, Goto T, Kondo T. Optimal schedule of preoperative embolization for spinal metastasis surgery. Spine (Phila Pa 1976). 38:1964–1969. 2013.
Article10. Kato S, Murakami H, Minami T, Demura S, Yoshioka K, Matsui O, et al. Preoperative embolization significantly decreases intraoperative blood loss during palliative surgery for spinal metastasis. Orthopedics. 35:e1389–e1395. 2012.
Article11. Kim CH. Surgical timing in lumbar disc herniation surgery. Neurospine. 17:213–214. 2020.
Article12. Kim KR, Le Huec JC, Jang HJ, Noh SH, Park JY, Ha Y, et al. Which is more predictive value for mechanical complications: fixed thoracolumbar alignment (T1 pelvic angle) versus dynamic global balance parameter (odontoid-hip axis angle). Neurospine. 18:597–607. 2021.
Article13. Kobayashi K, Ozkan E, Tam A, Ensor J, Wallace MJ, Gupta S. Preoperative embolization of spinal tumors: variables affecting intraoperative blood loss after embolization. Acta Radiol. 53:935–942. 2012.
Article14. Kumar N, Tan B, Zaw AS, Khine HE, Maharajan K, Lau LL, et al. The role of preoperative vascular embolization in surgery for metastatic spinal tumours. Eur Spine J. 25:3962–3970. 2016.
Article15. Kumar N, Zaw AS, Khine HE, Maharajan K, Wai KL, Tan B, et al. Blood loss and transfusion requirements in metastatic spinal tumor surgery: evaluation of influencing factors. Ann Surg Oncol. 23:2079–2086. 2016.
Article16. Ma J, Tullius T, Van Ha TG. Update on preoperative embolization of bone metastases. Semin Intervent Radiol. 36:241–248. 2019.
Article17. Nagoshi N, Nori S, Tsuji O, Suzuki S, Okada E, Yagi M, et al. Surgical and functional outcomes of expansive open-door laminoplasty for patients with mild kyphotic cervical alignment. Neurospine. 18:749–757. 2021.
Article18. Park SJ, Lim SH, Kim YJ, Moon KS, Kim IY, Jung S, et al. The tumor control according to radiation dose of gamma knife radiosurgery for small and medium-sized brain metastases from non-small cell lung cancer. J Korean Neurosurg Soc. 64:983–994. 2021.
Article19. Perez-Roman RJ, McCarthy D, Luther EM, Lugo-Pico JG, Leon-Correa R, Gaztanaga W, et al. Effects of body mass index on perioperative outcomes in patients undergoing anterior cervical discectomy and fusion surgery. Neurospine. 18:79–86. 2021.
Article20. Quraishi NA, Purushothamdas S, Manoharan SR, Arealis G, Lenthall R, Grevitt MP. Outcome of embolised vascular metastatic renal cell tumours causing spinal cord compression. Eur Spine J. 22(Suppl 1):S27–S32. 2013.
Article21. Schmidt R, Rupp-Heim G, Dammann F, Ulrich C, Nothwang J. Surgical therapy of vertebral metastases. Are there predictive parameters for intraoperative excessive blood loss despite preoperative embolization? Tumori. 97:66–73. 2011.22. Sun S, Lang EV. Bone metastases from renal cell carcinoma: preoperative embolization. J Vasc Interv Radiol. 9:263–269. 1998.
Article23. Tang B, Ji T, Guo W, Tang X, Jin L, Dong S, et al. Which is the better timing between embolization and surgery for hypervascular spinal tumors, the same day or the next day?: A retrospective comparative study. Medicine (Baltimore). 97:e10912. 2018.24. Wilson MA, Cooke DL, Ghodke B, Mirza SK. Retrospective analysis of preoperative embolization of spinal tumors. AJNR Am J Neuroradiol. 31:656–660. 2010.25. Wirbel RJ, Roth R, Schulte M, Kramann B, Mutschler W. Preoperative embolization in spinal and pelvic metastases. J Orthop Sci. 10:253–257. 2005.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Introduction of the Systematic Review and Meta-Analysis
- Clinical Significance of Preoperative Embolization for Non-Hypervascular Metastatic Spine Tumors
- A Commentary on “Does Vertebral Cement Augmentation Reduce Postoperative Proximal Junction Complications in Spinal Deformity Corrective Surgery: A Systematic Review and Meta-analysis”
- Trends in Utilization of Preoperative Embolization for Spinal Metastases: A Study of the National Inpatient Sample 2005–2017
- Systematic Review and Meta-analysis in Digestive Cancer Research