J Korean Neurosurg Soc.
2019 Jan;62(1):106-113. 10.3340/jkns.2018.0073.
Clinical Significance of Preoperative Embolization for Non-Hypervascular Metastatic Spine Tumors
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. boscoa@catholic.ac.kr
- 2Department of Orthopedic Surgery, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea.
- 3Department of Orthopedic Surgery, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 4Department of Orthopedic Surgery, Sanggye Paik Hospital, The Inje University College of Medicine, Seoul, Korea.
- KMID: 2434352
- DOI: http://doi.org/10.3340/jkns.2018.0073
Abstract
OBJECTIVE
The efficacy of preoperative embolization for hypervascular metastatic spine disease (MSD) such as renal cell and thyroid cancers has been reported. However, the debate on the efficacy of preoperative embolization for non-hypervascular MSD still remains unsettled. The purpose of this study is to determine whether preoperative embolization for non-hypervascular MSD decreases perioperative blood loss.
METHODS
A total of 79 patients (36 cases of preoperative embolization and 43 cases of non-embolization) who underwent surgery for metastatic spine lesions were included. Representative hypervascular tumors such as renal cell and thyroid cancers were excluded. Intraoperative and perioperative estimated blood losses (EBL), total number of transfusion and calibrated EBL were recorded in the embolization and non-embolization groups. The differences in EBL were also compared along with the type of surgery. In addition, the incidence of Adamkiewicz artery and complications of embolization were assessed.
RESULTS
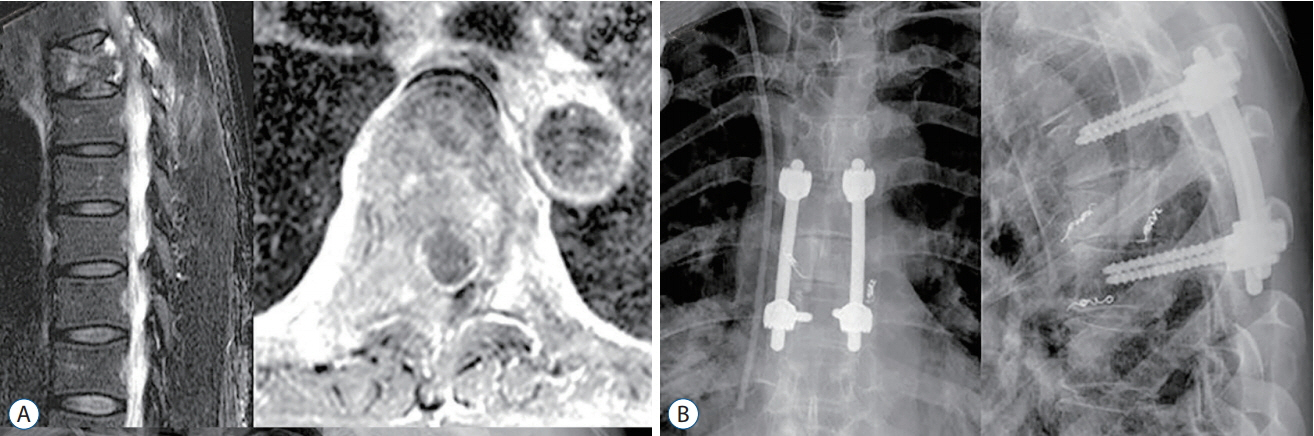
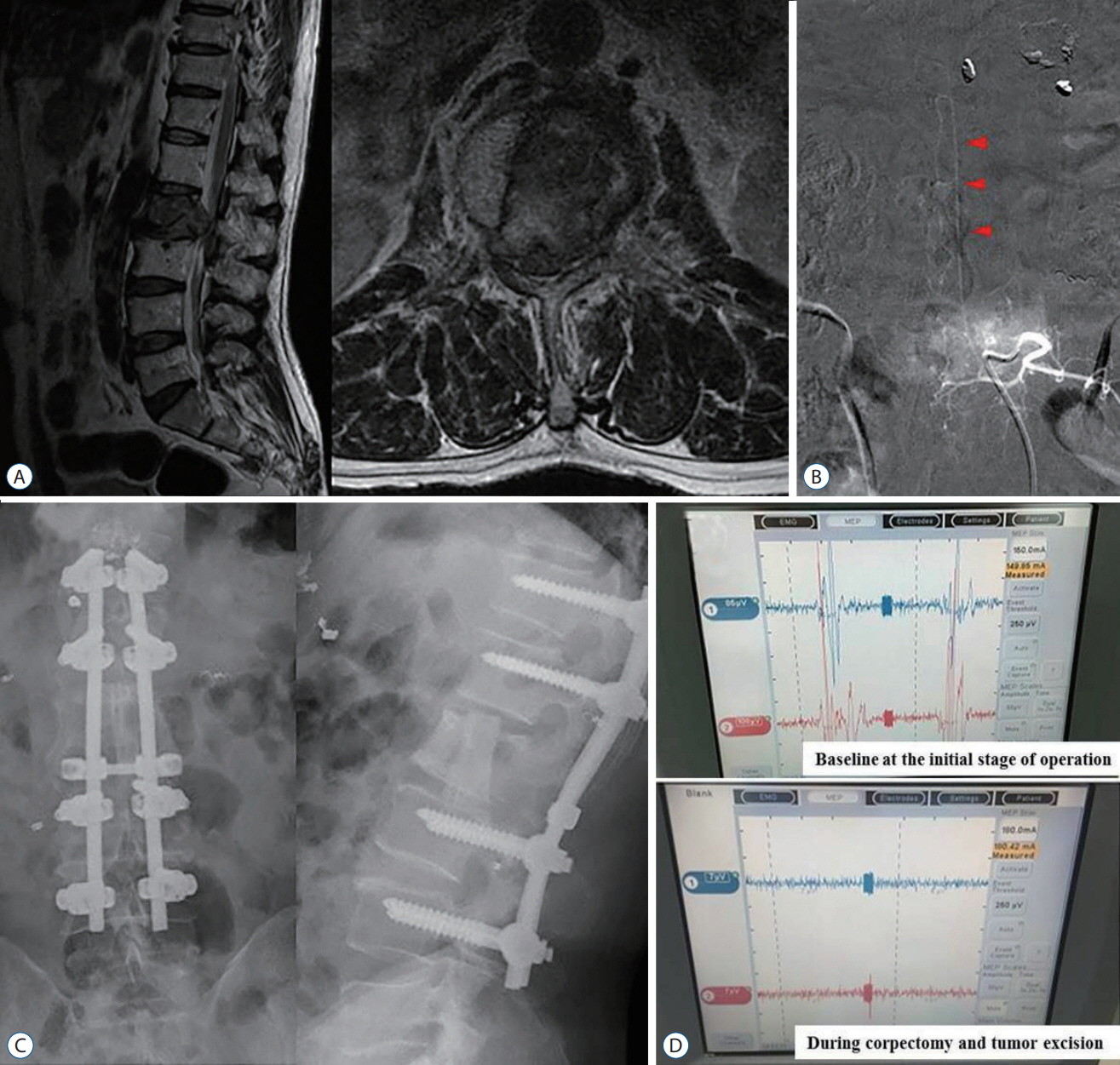
The average age of 50 males and 29 females was 57.6±13.5 years. Lung (30), hepatocellular (14), gastrointestinal (nine) and others (26) were the primary cancers. The demographic data was not significantly different between the embolization and the non-embolization groups. There were no significant differences in intraoperative EBL, perioperative EBL, total transfusion and calibrated EBL between two groups. However, intraoperative EBL and total transfusion in patients with preoperative embolization were significantly lower than in non-embolization in the corpectomy group (1645.5 vs. 892.6 mL, p=0.017 for intraoperative EBL and 6.1 vs. 3.9, p=0.018 for number of transfusion). In addition, the presence of Adamkiewicz artery at the index level was noted in two patients. Disruption of this major feeder artery resulted in significant changes in intraoperative neuromonitoring.
CONCLUSION
Preoperative embolization for non-hypervascular MSD did not reduce perioperative blood loss. However, the embolization significantly reduced intraoperative bleeding and total transfusion in corpectomy group. Moreover, the procedure provided insights into the anatomy of tumor and spinal cord vasculature.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Unstable Pathologic Vertebral Fractures in Multiple Myeloma : Propensity Score Matched Cohort Study between Reconstructive Surgery with Adjuvant Radiotherapy and Radiotherapy Alone
Hyung-Youl Park, Young-Hoon Kim, Joo-Hyun Ahn, Kee-Yong Ha, Sang-Il Kim, Jae-Woong Jung
J Korean Neurosurg Soc. 2022;65(2):287-296. doi: 10.3340/jkns.2021.0199.
Reference
-
References
1. Barton PP, Waneck RE, Karnel FJ, Ritschl P, Kramer J, Lechner GL. Embolization of bone metastases. J Vasc Interv Radiol. 7:81–88. 1996.
Article2. Berkefeld J, Scale D, Kirchner J, Heinrich T, Kollath J. Hypervascular spinal tumors: influence of the embolization technique on perioperative hemorrhage. AJNR Am J Neuroradiol. 20:757–763. 1999.3. Clausen C, Dahl B, Frevert SC, Hansen LV, Nielsen MB, Lönn L. Preoperative embolization in surgical treatment of spinal metastases: singleblind, randomized controlled clinical trial of efficacy in decreasing intraoperative blood loss. J Vasc Interv Radiol. 26:402–412.e1. 2015.
Article4. Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 35:E1221–E1229. 2010.5. Guzman R, Dubach-Schwizer S, Heini P, Lovblad KO, Kalbermatten D, Schroth G, et al. Preoperative transarterial embolization of vertebral metastases. Eur Spine J. 14:263–268. 2005.
Article6. Heran MK. Preoperative embolization of spinal metastatic disease: rationale and technical considerations. Semin Musculoskelet Radiol. 15:135–142. 2011.
Article7. Jacobs WB, Perrin RG. Evaluation and treatment of spinal metastases: an overview. Neurosurg Focus. 11:e10. 2001.
Article8. Kato S, Murakami H, Minami T, Demura S, Yoshioka K, Matsui O, et al. Preoperative embolization significantly decreases intraoperative blood loss during palliative surgery for spinal metastasis. Orthopedics. 35:e1389–e1395. 2012.
Article9. Kobayashi K, Ozkan E, Tam A, Ensor J, Wallace MJ, Gupta S. Preoperative embolization of spinal tumors: variables affecting intraoperative blood loss after embolization. Acta Radiol. 53:935–942. 2012.
Article10. Manke C, Bretschneider T, Lenhart M, Strotzer M, Neumann C, Gmeinwieser J, et al. Spinal metastases from renal cell carcinoma: effect of preoperative particle embolization on intraoperative blood loss. AJNR Am J Neuroradiol. 22:997–1003. 2001.11. Murakami H, Kawahara N, Tomita K, Demura S, Kato S, Yoshioka K : Does interruption of the artery of Adamkiewicz during total en bloc spondylectomy affect neurologic function? Spine (Phila Pa 1976) 35 : E1187-E1192, 2010.12. Nair S, Gobin YP, Leng LZ, Marcus JD, Bilsky M, Laufer I, et al. Preoperative embolization of hypervascular thoracic, lumbar, and sacral spinal column tumors: technique and outcomes from a single center. Interv Neuroradiol. 19:377–385. 2013.
Article13. Orchowski J, Bridwell KH, Lenke LG. Neurological deficit from a purely vascular etiology after unilateral vessel ligation during anterior thoracolumbar fusion of the spine. Spine (Phila Pa 1976). 30:406–410. 2005.
Article14. Pajewski TN, Arlet V, Phillips LH. Current approach on spinal cord monitoring: the point of view of the neurologist, the anesthesiologist and the spine surgeon. Eur Spine J 16 Suppl. 2:S115–S129. 2007.
Article15. Pikis S, Itshayek E, Barzilay Y, Hasharoni A, Kaplan L, Gomori M, et al. Preoperative embolization of hypervascular spinal tumors: current practice and center experience. Neurol Res. 36:502–509. 2014.
Article16. Robial N, Charles YP, Bogorin I, Godet J, Beaujeux R, Boujan F, et al. Is preoperative embolization a prerequisite for spinal metastases surgical management? Orthop Traumatol Surg Res. 98:536–542. 2012.
Article17. Thiex R, Harris MB, Sides C, Bono CM, Frerichs KU. The role of preoperative transarterial embolization in spinal tumors. A large single-center experience. Spine J. 13:141–149. 2013.
Article18. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 30:2186–2191. 2005.
Article19. Truumees E, Dodwad SN, Kazmierczak CD. Preoperative embolization in the treatment of spinal metastasis. J AM Acad Orthop Surg. 18:449–453. 2010.
Article20. White AP, Kwon BK, Lindskog DM, Friedlaender GE, Grauer JN. Metastatic disease of the spine. J AM Acad Orthop Surg. 14:587–598. 2006.
Article21. Wilson MA, Cooke DL, Ghodke B, Mirza SK. Retrospective analysis of preoperative embolization of spinal tumors. AJNR Am J Neuroradiol. 31:656–660. 2010.
Article22. Wirbel RJ, Roth R, Schulte M, Kramann B, Mutschler W. Preoperative embolization in spinal and pelvic metastases. J Orthop Sci. 10:253–257. 2005.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preoperative embolization and en bloc resection of a metastatic pheochromocytoma of the cervical spine
- Preoperative Embolization of Hypervascular Brain Tumor Fed by Branches of the Internal Carotid Artery
- Trends in Utilization of Preoperative Embolization for Spinal Metastases: A Study of the National Inpatient Sample 2005–2017
- Therapeutic Embolization of Renal Tumor
- The Optimal Time between Embolization and Surgery for Hypervascular Spinal Metastatic Tumors : A Systematic Review and Meta-Analysis