J Cerebrovasc Endovasc Neurosurg.
2024 Sep;26(3):331-337. 10.7461/jcen.2024.E2023.04.005.
Preoperative embolization and en bloc resection of a metastatic pheochromocytoma of the cervical spine
- Affiliations
-
- 1Department of Neurosurgery, University of Rochester Medical Center, Rochester, NY
- KMID: 2559445
- DOI: http://doi.org/10.7461/jcen.2024.E2023.04.005
Abstract
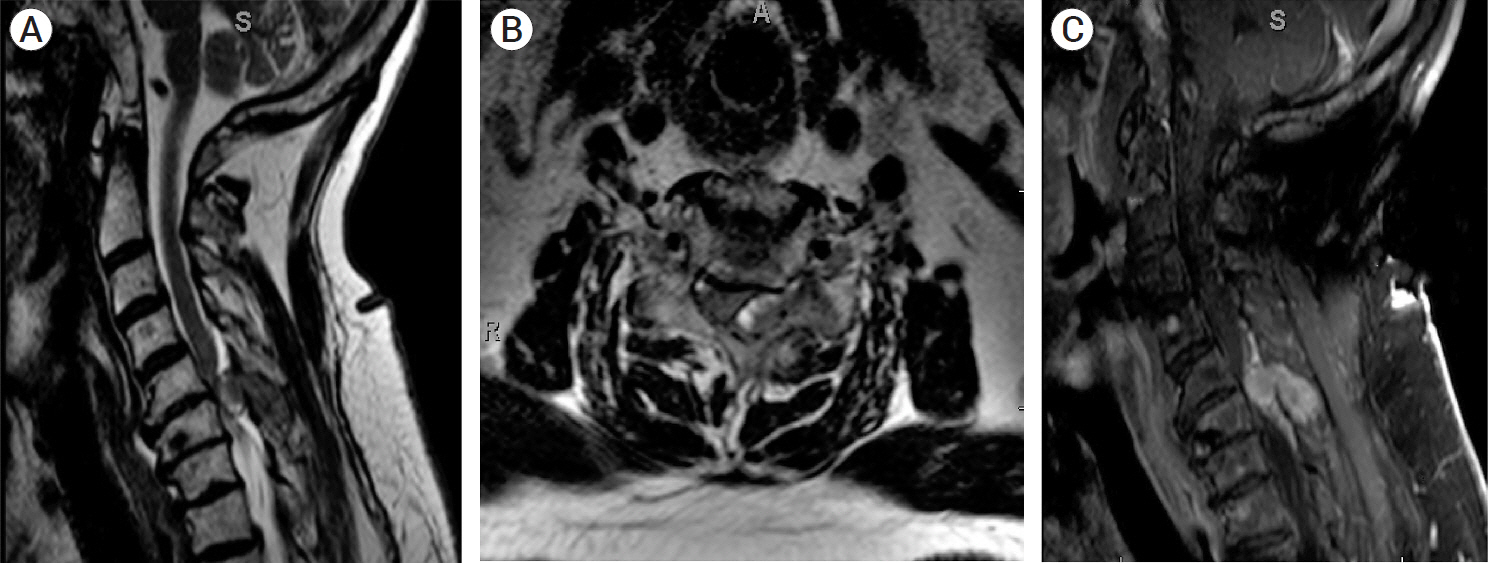
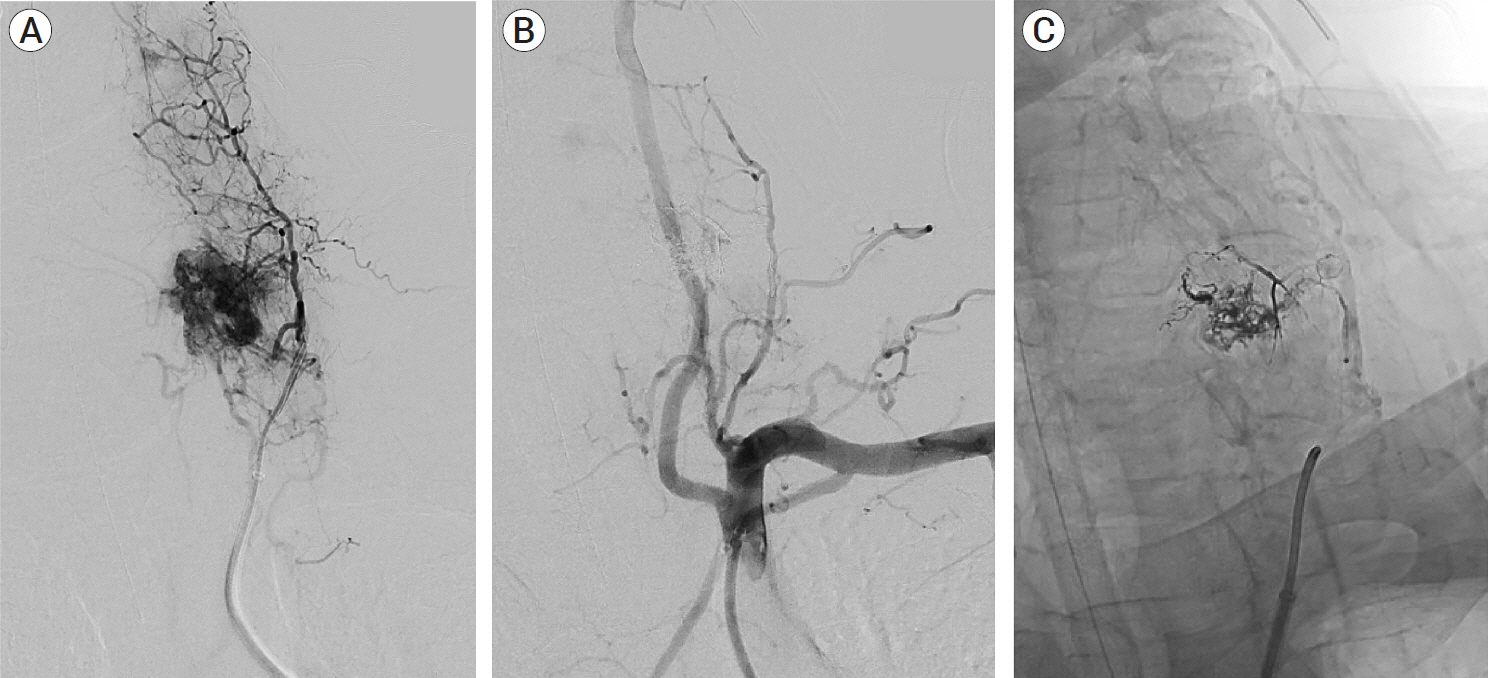
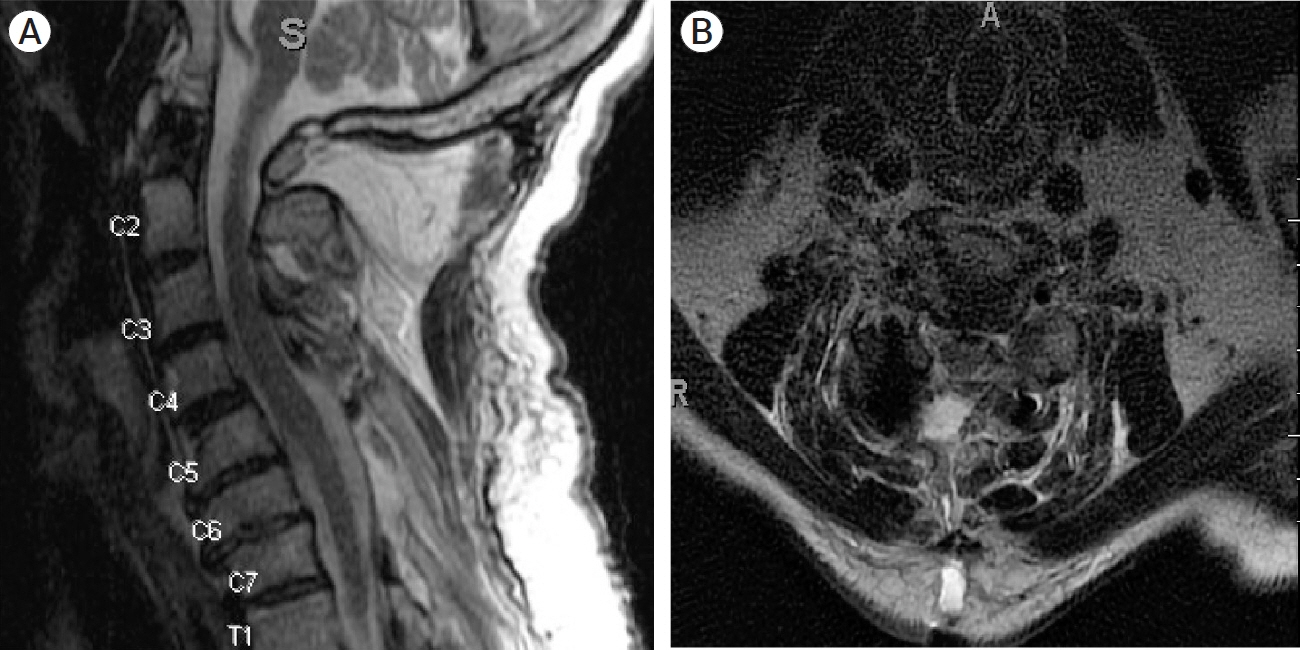
- This is a unique case of metastatic pheochromocytoma of the cervical spine treated with preoperative embolization and subsequent en bloc resection. A 65-year-old man with metastatic pheochromocytoma presented with two weeks of worsening neck pain, left arm and leg weakness and paresthesia, and urinary incontinence. Magnetic resonance imaging showed a metastatic osseous lesion at C6 with severe stenosis and spinal cord compression. The patient underwent successful preoperative angiographic embolization with a liquid embolic agent followed by C5-C7 laminectomy, en bloc tumor resection, and C3-T2 posterior spinal fusion. Six weeks postoperatively, the patient reported improving strength and resolving neck pain and paresthesias. While there is no standard paradigm for the treatment of metastatic pheochromocytomas of the cervical spine, preoperative embolization may minimize intraoperative blood loss and hemodynamic instability during subsequent surgical resection.
Keyword
Figure
Reference
-
1. Ahlman H. Malignant pheochromocytoma: State of the field with future projections. Annals of the New York Academy of Sciences. 2006; Aug. 1073(1):449–64.2. Cross GO, Pace JW. Malignant pheochromocytoma with paroxysmal hypertension and metastasis to the cervical spine. JAMA. 1950; 142(14):1068–70.3. Kaloostian PE, Zadnik PL, Awad AJ, McCarthy E, Wolinsky JP, Sciubba DM. En bloc resection of a pheochromocytoma metastatic to the spine for local tumor control and for treatment of chronic catecholamine release and related hypertension. J Neurosurg Spine. 2013; Jun. 18(6):611–6.
Article4. Kaloostian PE, Zadnik PL, Kim JE, Groves ML, Wolinsky JP, Gokaslan ZL, et al. High incidence of morbidity following resection of metastatic pheochromocytoma in the spine: Report of 5 cases. J Neurosurg Spine. 2014; Jun. 20(6):726–33.5. Kasliwal MK, Sharma MS, Vaishya S, Sharma BS. Metachronous pheochromocytoma metastasis to the upper dorsal spine-6-year survival. Spine Journal. 2008; Sep. 8(5):845–8.
Article6. Kheir E, Pal D, Mohanlal P, Shivane A, Chakrabarty A, Timothy J. Cervical spine metastasis from adrenal pheochromocytoma. Acta Neurochir (Wien). 2006; Nov. 148(11):1219–20.
Article7. Liu S, Song A, Zhou X, Kong X, Li WA, Wang Y, et al. Malignant pheochromocytoma with multiple vertebral metastases causing acute incomplete paralysis during pregnancy: Literature review with one case report. Medicine (Baltimore). 2017; Nov. 96(44):e8535.8. Liu S, Zhou X, Song A, Li WA, Rastogi R, Wang Y, et al. Successful treatment of malignant pheochromocytoma with sacrum metastases: A case report. Medicine (Baltimore). 2018; Aug. 97(35):e12184.9. Olson JJ, Loftus CM, Hitchon PW. Briefly noted: Metastatic pheochromocytoma of the cervical spine. Spine. 1989; Mar. 14(3):349–51.10. Rizzoni D, Porteri E, Castellano M, Bettoni G, Muiesan ML, Muiesan P, et al. Vascular hypertrophy and remodeling in secondary hypertension. Hypertension. 1996; Nov. 28(5):785–90.
Article11. Takahashi K, Ashizawa N, Minami T, Suzuki S, Sakamoto I, Hayashi K, et al. Malignant pheochromocytoma with multiple hepatic metastases treated by chemotherapy and transcatheter arterial embolization. Internal Medicine. 1999; Apr. 38(4):349–54.
Article12. Visani J, Mongardi L, Cultrera F, de Bonis P, Lofrese G, Ricciardi L, et al. Surgical treatment of metastatic pheochromocytomas of the spine: A systematic review. J Integr Neurosci. 2021; Jun. 20(2):499–507.13. Yamaguchi S, Hida K, Nakamura N, Seki T, Iwasaki Y. Multiple vertebral metastases from malignant cardiac pheochromocytoma: Case report. Neurol Med Chir (Tokyo). 2003; Jul. 43(7):352–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Combined en Bloc Spondylectomy and Chest Wall Resection for Malignant Tumors Invading Spinal Column and Chest Wall
- Right trisectionectomy with en bloc portal vein resection for perihilar cholangiocarcinoma after preoperative left portal vein stenting and sequential right portal and hepatic vein embolization
- Total en bloc Spondylectomy for Solitary Metastatic Spinal Tumor
- Operative Technique for En Bloc Resection of Upper Cervical Chordomas: Extended Transoral Transmandibular Approach and Multilevel Reconstruction
- Large Aneurysmal Bone Cyst of the Posterior Archofa Lumbar Vertebraina Child Treated with En Bloc Excision: A Case Report