J Korean Med Sci.
2023 May;38(18):e137. 10.3346/jkms.2023.38.e137.
Analysis of the Effects of COVID-19 on Hip Fractures in Korea Without Lockdown: Interrupted Time Series Analysis Using a Nationwide Cohort
- Affiliations
-
- 1Department of Healthcare Management, Graduate School of Public Health, Yonsei University, Seoul, Korea
- 2Department of Orthopedic Surgery, Daejeon Eulji Medical Center, Eulji University School of Medicine, Daejeon, Korea
- KMID: 2542029
- DOI: http://doi.org/10.3346/jkms.2023.38.e137
Abstract
- Background
The purpose of this study was to investigate the change in the incidence rate, length of hospital stay (LOS), in-hospital mortality rate, and surgical method of hip fractures during the coronavirus disease 2019 (COVID-19) pandemic in South Korea where lockdown restrictions were not implemented.
Methods
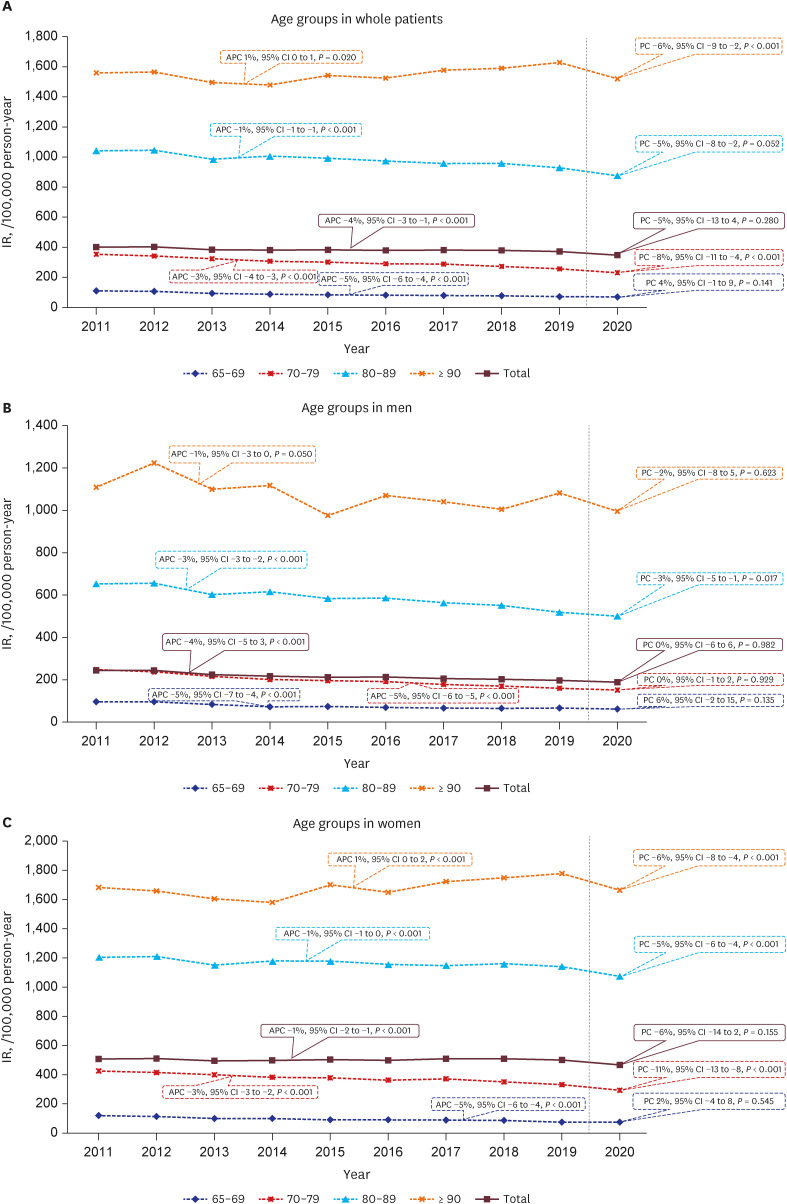
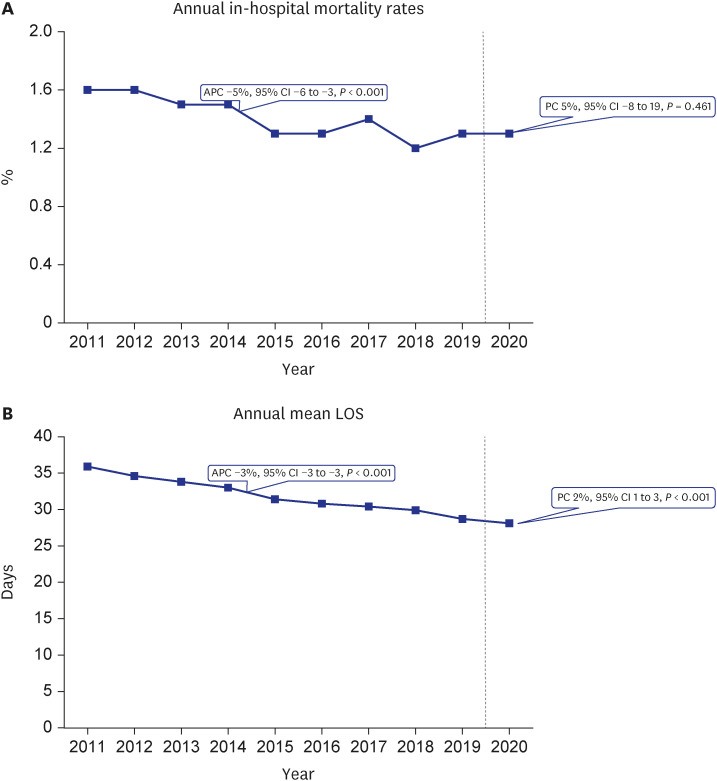
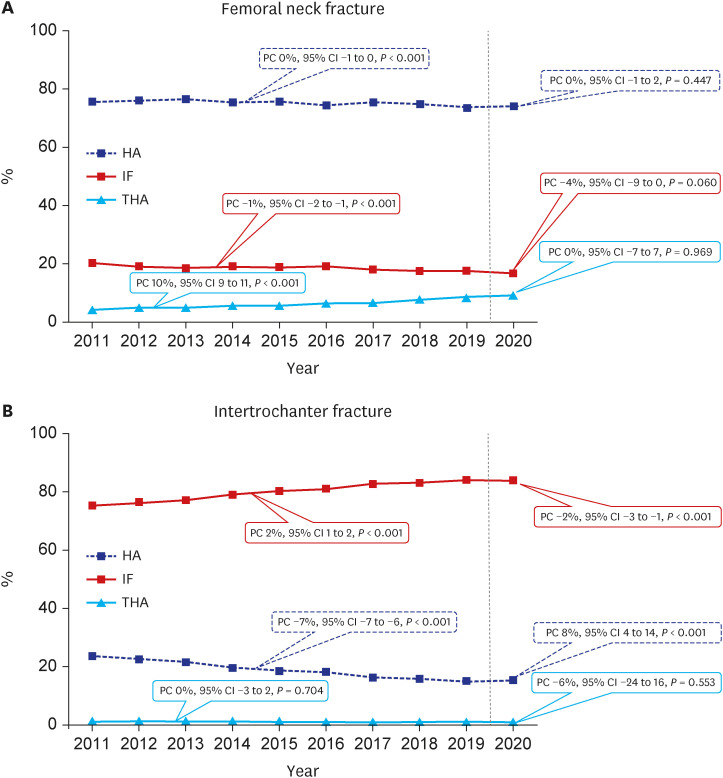
We calculated the expected values of the incidence of hip fractures, in-hospital mortality and LOS of hip fracture patients in 2020 (COVID period) based hip fracture database of the Korean National Health Insurance Review and Assessment (HIRA) during a 9-year period from 2011 to 2019 (pre-COVID period). A generalized estimating equation model with Poisson distribution and logarithmic link function was used to estimate adjusted annual percent change (PC) of incidence rate and 95% confidence intervals (CIs). Then, we compared the annual incidence, in-hospital mortality rate and LOS in 2020 with the expected values.
Results
The overall incidence rate of hip fracture in 2020 was not significantly different from the expected value (PC, −5%; 95% CI, −13 to 4; P = 0.280). In women, the incidence rate of hip fracture in age groups over 70 years was smaller than the predicted value (P < 0.001). The in-hospital mortality rate was not significantly different from the expected value (PC, 5%; 95% CI, −8 to 19; P = 0.461). The mean LOS was larger than the expected value by 2% (PC, 2%; 95% CI, 1 to 3; P < 0.001). In intertrochanteric fracture, the proportion of internal fixation was smaller than the predicted value by 2% (PC, −2%; 95% CI, −3 to −1; P < 0.001), and that of hemiarthroplasty was larger than the predicted value by 8% (PC, 8%; 95% CI, 4 to 14; P < 0.001).
Conclusions
In 2020, the incidence rate of hip fracture did not significantly decrease, and inhospital mortality rate did not significantly increase compared to the expected rates, which were projected based on the HIRA hip fracture data from 2011 to 2019. Only LOS increased slightly.
Keyword
Figure
Reference
-
1. Wilk R, Adamczyk P, Pluskiewicz W, Skrzypek M, Hajzyk M, Koczy B. One year of the COVID-19 pandemic in Poland-the incidence of osteoporotic forearm, arm, and hip fractures. Arch Osteoporos. 2022; 17(1):38. PMID: 35239040.
Article2. Jung J. A long way to the recovery: COVID-19 will not disappear. J Korean Med Sci. 2021; 36(32):e231. PMID: 34402229.
Article3. Slullitel PA, Lucero CM, Soruco ML, Barla JD, Benchimol JA, Boietti BR, et al. Prolonged social lockdown during COVID-19 pandemic and hip fracture epidemiology. Int Orthop. 2020; 44(10):1887–1895. PMID: 32772318.
Article4. Shin MS, Sim B, Jang WM, Lee JY. Estimation of excess all-cause mortality during COVID-19 pandemic in Korea. J Korean Med Sci. 2021; 36(39):e280. PMID: 34636505.
Article5. Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011; 26(8):1087–1092. PMID: 21860561.
Article6. Nazemi AK, Al-Humadi SM, Tantone R, Hays TR, Bowen SN, Komatsu DE, et al. Hip fractures before and during the COVID-19 pandemic: comparative demographics and outcomes. Geriatr Orthop Surg Rehabil. 2021; 12:21514593211003077. PMID: 33796344.
Article7. Amzallag N, Factor S, Shichman I, Ben-Tov T, Khoury A. Hip fractures during the COVID-19 pandemic: demographics, treatment pathway, and outcomes. Isr Med Assoc J. 2021; 23(8):484–489. PMID: 34392622.8. Brent L, Ferris H, Sorensen J, Valentelyte G, Kelly F, Hurson C, et al. Impact of COVID-19 on hip fracture care in Ireland: findings from the Irish Hip Fracture Database. Eur Geriatr Med. 2022; 13(2):425–431. PMID: 35064562.
Article9. da Silva AC, da Silva Santos G, Maluf EM, Borba VZ. Incidence of hip fractures during the COVID-19 pandemic in the Brazilian public health care system. Arch Osteoporos. 2022; 17(1):42. PMID: 35253090.
Article10. Hadfield JN, Gray AC. The evolving COVID-19 effect on hip fracture patients. Injury. 2020; 51(7):1411–1412. PMID: 32553412.
Article11. Kim KK, Lee SW, Choi JK, Won YY. Epidemiology and postoperative complications of hip fracture during COVID-19 pandemic. Osteoporos Sarcopenia. 2022; 8(1):17–23. PMID: 35350648.
Article12. Johansen A, Inman DS. A view of COVID-19 from the perspective of the National Hip Fracture Database. Bone Joint J. 2021; 103-B(6):1007–1008. PMID: 34058880.
Article13. Shemesh S, Bebin A, Niego N, Frenkel Rutenberg T. The impact of the COVID-19 2020 pandemic on hospital length of stay following fragility hip fracture surgery. Isr Med Assoc J. 2021; 23(8):469–474. PMID: 34392619.14. Prosso I, Oren N, Livshits G, Lakstein D. Incidence and mortality rate of hip fractures in different age groups during the first wave of the COVID-19 pandemic. Isr Med Assoc J. 2021; 23(8):475–478. PMID: 34392620.15. Ojeda-Thies C, Cuarental-García J, Ramos-Pascua LR. Decreased volume of hip fractures observed during COVID-19 lockdown. Eur Geriatr Med. 2021; 12(4):759–766. PMID: 33481186.
Article16. Health Insurance Review and Assessment. Accessed March 1, 2023. https://opendata.hira.or.kr/home.do .17. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID: 16224307.
Article18. Schweda A, Weismüller B, Bäuerle A, Dörrie N, Musche V, Fink M, et al. Phenotyping mental health: age, community size, and depression differently modulate COVID-19-related fear and generalized anxiety. Compr Psychiatry. 2021; 104:152218. PMID: 33232827.
Article19. Ju G, Lee J, Ahn MH, Lee J, Kim EJ, Suh S, et al. Effects of depression and resilience of public workers on work-related stress and anxiety in response to the COVID-19 pandemic. J Korean Med Sci. 2021; 36(36):e262. PMID: 34519189.
Article20. Park C, Hwang JM, Jo S, Bae SJ, Sakong J. COVID-19 outbreak and its association with healthcare workers’ emotional stress: a cross-sectional study. J Korean Med Sci. 2020; 35(41):e372. PMID: 33107230.
Article21. Malik-Tabassum K, Robertson A, Tadros BJ, Chan G, Crooks M, Buckle C, et al. The effect of the COVID-19 lockdown on the epidemiology of hip fractures in the elderly: a multicentre cohort study. Ann R Coll Surg Engl. 2021; 103(5):337–344. PMID: 33715420.
Article22. Pluskiewicz W, Wilk R, Adamczyk P, Hajzyk M, Swoboda M, Sladek A, et al. The incidence of arm, forearm, and hip osteoporotic fractures during early stage of COVID-19 pandemic. Osteoporos Int. 2021; 32(8):1595–1599. PMID: 33515269.
Article23. Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011; 469(7):1913–1918. PMID: 21161737.
Article24. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res. 2020; 136:110186. PMID: 32682159.
Article25. Visser M, Schaap LA, Wijnhoven HA. Self-reported impact of the COVID-19 pandemic on nutrition and physical activity behaviour in dutch older adults living independently. Nutrients. 2020; 12(12):3708. PMID: 33266217.
Article26. Wang KC, Xiao R, Cheung ZB, Barbera JP, Forsh DA. Early mortality after hip fracture surgery in COVID-19 patients: a systematic review and meta-analysis. J Orthop. 2020; 22:584–591. PMID: 33223732.
Article27. Raheman FJ, Rojoa DM, Nayan Parekh J, Berber R, Ashford R. Meta-analysis and metaregression of risk factors associated with mortality in hip fracture patients during the COVID-19 pandemic. Sci Rep. 2021; 11(1):10157. PMID: 33980936.
Article28. Minarro JC, Zamorano-Moyano C, Urbano-Luque MT, Arenas-de Larriva AP, Izquierdo-Fernández A, Quevedo-Reinoso R. Is COVID-19 affecting the incidence of hip fractures? Injury. 2020; 51(10):2329. PMID: 32713621.
Article29. Waterman JL, Jayaraju U, Nadimi JK, Morgan D. Impact of COVID-19 on key performance indicators of the national hip fracture database and the management of hip fracture patients. Cureus. 2021; 13(12):e20575. PMID: 35103154.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improving Causal Inference in Observational Studies: Interrupted Time Series Design
- Mortality Rate and Outcomes of Omicron Variant Positive Patients with Osteoporotic Fractures: A Retrospective Study
- Did the COVID-19 pandemic impact the surgical treatment of febrile acute appendicitis at a single center in Korea, a country not under lockdown? Observational cohort study
- Impact of Government Healthcare Policy Changes on Consumption and Human Movements During COVID-19: An Interrupted Time Series Analysis in Korea
- Impact of COVID-19 lockdown on blood glucose levels in pediatric patients with type 1 diabetes mellitus