J Korean Neurosurg Soc.
2023 May;66(3):316-323. 10.3340/jkns.2022.0264.
Morbidity and Mortality Trends in Preterm Infants of <32 Weeks Gestational Age with Severe Intraventricular Hemorrhage : A 14-Year Single-Center Retrospective Study
- Affiliations
-
- 1Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, Korea University College of Medicine, Seoul, Korea
- 3Department of Radiology, Korea University College of Medicine, Seoul, Korea
- KMID: 2542017
- DOI: http://doi.org/10.3340/jkns.2022.0264
Abstract
Objective
: Owing to advances in critical care treatment, the overall survival rate of preterm infants born at a gestational age (GA) <32 weeks has consistently improved. However, the incidence of severe intraventricular hemorrhage (IVH) has persisted, and there are few reports on in-hospital morbidity and mortality. Therefore, the aim of the present study was to investigate trends surrounding in-hospital morbidity and mortality of preterm infants with severe IVH over a 14-year period.
Methods
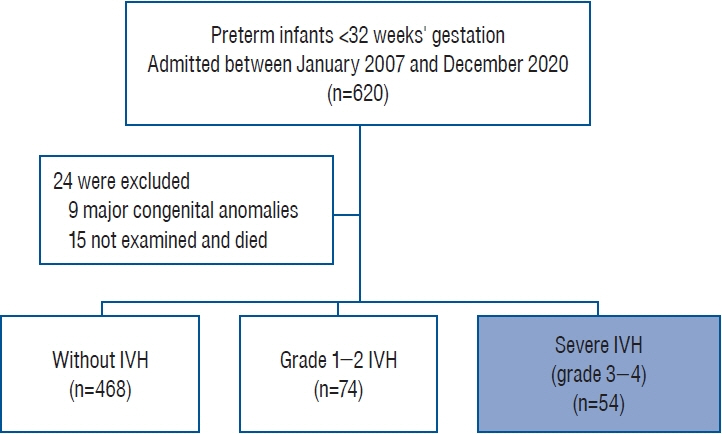
: This single-center retrospective study included 620 infants born at a GA <32 weeks, admitted between January 2007 and December 2020. After applying exclusion criteria, 596 patients were included in this study. Infants were grouped based on the most severe IVH grade documented on brain ultrasonography during their admission, with grades 3 and 4 defined as severe. We compared in-hospital mortality and clinical outcomes of preterm infants with severe IVH for two time periods : 2007–2013 (phase I) and 2014–2020 (phase II). Baseline characteristics of infants who died and survived during hospitalization were analyzed.
Results
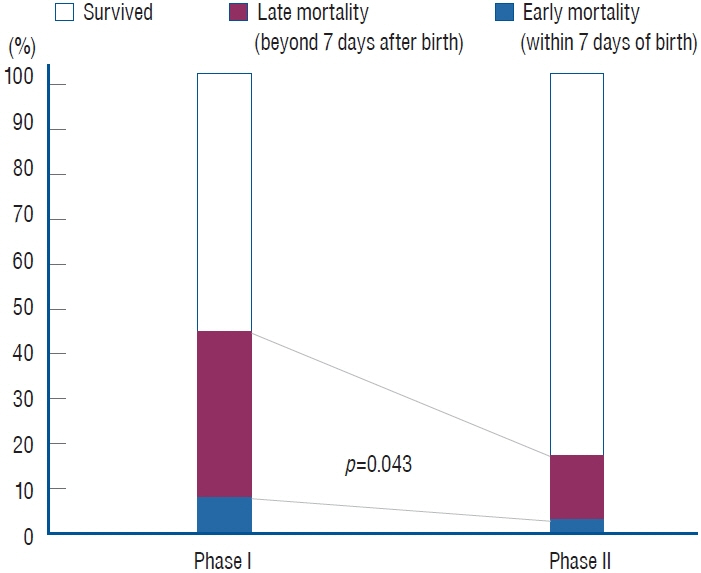
: A total of 54 infants (9.0%) were diagnosed with severe IVH over a 14-year period; overall in-hospital mortality rate was 29.6%. Late in-hospital mortality rate (>7 days after birth) for infants with severe IVH significantly improved over time, decreasing from 39.1% in phase I to 14.3% in phase II (p=0.043). A history of hypotension treated with vasoactive medication within 1 week after birth (adjusted odds ratio, 7.39; p=0.025) was found to be an independent risk factor for mortality. When comparing major morbidities of surviving infants, those in phase II were significantly more likely to have undergone surgery for necrotizing enterocolitis (NEC) (29.2% vs. 0.0%; p=0.027). Additionally, rates of late-onset sepsis (45.8% vs. 14.3%; p=0.049) and central nervous system infection (25.0% vs. 0.0%; p=0.049) were significantly higher in phase II survivors than in phase I survivors.
Conclusion
: In-hospital mortality in preterm infants with severe IVH decreased over the last decade, whereas major neonatal morbidities increased, particularly surgical NEC and sepsis. This study suggests the importance of multidisciplinary specialized medical and surgical neonatal intensive care in preterm infants with severe IVH.
Keyword
Figure
Reference
-
References
1. Ahn SY, Shim SY, Sung IK. Intraventricular hemorrhage and post hemorrhagic hydrocephalus among very-low-birth-weight infants in Korea. J Korean Med Sci 30 Suppl. 1(Suppl 1):S52–S58. 2015.
Article2. Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 67:1–8. 2010.
Article3. Batton B, Li L, Newman NS, Das A, Watterberg KL, Yoder BA, et al. Early blood pressure, antihypotensive therapy and outcomes at 18-22 months' corrected age in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 101:F201–F206. 2016.4. Bolisetty S, Dhawan A, Abdel-Latif M, Bajuk B, Stack J, Lui K, et al. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics. 133:55–62. 2014.
Article5. Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J Neurosurg Pediatr. 17:260–269. 2016.
Article6. Christian EA, Melamed EF, Peck E, Krieger MD, McComb JG. Surgical management of hydrocephalus secondary to intraventricular hemorrhage in the preterm infant. J Neurosurg Pediatr. 17:278–284. 2016.
Article7. Culbreath K, Knell J, Keefe G, Nes E, Han SM, Edwards EM, et al. Impact of concomitant necrotizing enterocolitis on mortality in very low birth weight infants with intraventricular hemorrhage. J Perinatol. 43:91–96. 2023.
Article8. Fanaroff JM, Wilson-Costello DE, Newman NS, Montpetite MM, Fanaroff AA. Treated hypotension is associated with neonatal morbidity and hearing loss in extremely low birth weight infants. Pediatrics. 117:1131–1135. 2006.
Article9. Foglia EE, Roberts RS, Stoller JZ, Davis PG, Haslam R, Schmidt B, et al. Effect of prophylactic indomethacin in extremely low birth weight infants based on the predicted risk of severe intraventricular hemorrhage. Neonatology. 113:183–186. 2018.
Article10. Hall NJ, Hiorns M, Tighe H, Peters M, Khoo AK, Eaton S, et al. Is necrotizing enterocolitis associated with development or progression of intraventricular hemorrhage? Am J Perinatol. 26:139–143. 2009.
Article11. Han RH, McKinnon A, CreveCoeur TS, Baksh BS, Mathur AM, Smyser CD, et al. Predictors of mortality for preterm infants with intraventricular hemorrhage: a population-based study. Childs Nerv Syst. 34:2203–2213. 2018.
Article12. Hwang-Bo S, Seo YM, Oh MY, Im SA, Youn YA. The prognosis of refractory hypotension and severe intraventricular hemorrhage in very low birth weight infants. Medicine (Baltimore). 101:e29598. 2022.
Article13. Jen HC, Graber JJ, Hill JL, Alaish SM, Voigt RW, Strauch ED. Surgical necrotizing enterocolitis and intraventricular hemorrhage in premature infants below 1000 g. J Pediatr Surg. 41:1425–1430. 2006.
Article14. Kazan S, Güra A, Uçar T, Korkmaz E, Ongun H, Akyuz M. Hydrocephalus after intraventricular hemorrhage in preterm and low-birth weight infants: analysis of associated risk factors for ventriculoperitoneal shunting. Surg Neurol 64 Suppl. 2:S77–S81. discussion S81. 2005.
Article15. Lee JH, Youn Y, Chang YS. Short- and long-term outcomes of very low birth weight infants in Korea: Korean Neonatal Network update in 2019. Clin Exp Pediatr. 63:284–290. 2020.
Article16. Lundgren P, Morsing E, Hård AL, Rakow A, Hellström-Westas L, Jacobson L, et al. National cohort of infants born before 24 gestational weeks showed increased survival rates but no improvement in neonatal morbidity. Acta Paediatr. 111:1515–1525. 2022.
Article17. Matei A, Montalva L, Goodbaum A, Lauriti G, Zani A. Neurodevelopmental impairment in necrotising enterocolitis survivors: systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 105:432–439. 2020.
Article18. McCauley KE, Carey EC, Weaver AL, Mara KC, Clark RH, Carey WA, et al. Survival of ventilated extremely premature neonates with severe intraventricular hemorrhage. Pediatrics. 147:e20201584. 2021.
Article19. Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 364:255–264. 2011.
Article20. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 92:529–534. 1978.
Article21. Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, et al. Causes and timing of death in extremely premature infants from 2000 through 2011. N Engl J Med. 372:331–340. 2015.
Article22. Payne AH, Hintz SR, Hibbs AM, Walsh MC, Vohr BR, Bann CM, et al. Neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular-intraventricular hemorrhage. JAMA Pediatr. 167:451–459. 2013.
Article23. Sadarangani SP, Batdorf R, Buchhalter LC, Mrelashvili A, Banerjee R, Henry NK, et al. Clostridium septicum brain abscesses in a premature neonate. Pediatr Infect Dis J. 33:538–540. 2014.
Article24. St Peter D, Gandy C, Hoffman SB. Hypotension and adverse outcomes in prematurity: comparing definitions. Neonatology. 111:228–233. 2017.
Article25. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 126:443–456. 2010.
Article26. van de Bor M, Verloove-Vanhorick SP, Brand R, Keirse MJ, Ruys JH. Incidence and prediction of periventricular-intraventricular hemorrhage in very preterm infants. J Perinat Med. 15:333–339. 1987.
Article27. Wu T, Wang Y, Xiong T, Huang S, Tian T, Tang J, et al. Risk factors for the deterioration of periventricular-intraventricular hemorrhage in preterm infants. Sci Rep. 10:13609. 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends of Mortality, Time, and Causes of Death in Preterm Infants
- Perinatal Outcome in Small for Gestational Age Versus Appropriate for Gestational Age in Preterm Infants
- Effects of Recombinant Human Erythropoietin Administration in Premature Infants with Severe Intraventricular Hemorrhage: A Single-Center Experience
- Risk Factors of Cystic Periventricular Leukomalacia in Preterm Infants with Gestational Ages of Less Than 32 Weeks according to Gestational Age Group
- Fibrinolytic (Thrombolytic) Therapy for Post Intraventricular Hemorrhagic Hydrocephalus in Preterm Infants