Perinatology.
2019 Dec;30(4):221-228. 10.14734/PN.2019.30.4.221.
Trends of Mortality, Time, and Causes of Death in Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. iamgawon@hanmail.net
- KMID: 2468543
- DOI: http://doi.org/10.14734/PN.2019.30.4.221
Abstract
OBJECTIVE
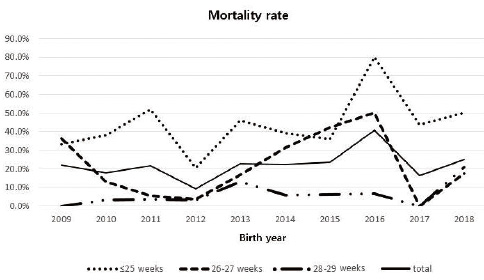
Although survival rate of preterm infants in Korea has increased in the past several decades, it seems to be stable recently. The objective of this study is to evaluate the mortality rate of preterm infants in a single center in Korea between 2009 and 2018.
METHODS
Preterm infants with gestational age (GA) < 30 weeks who were admitted to Busan Paik Hospital (January 2009 to December 2018) were enrolled.
RESULTS
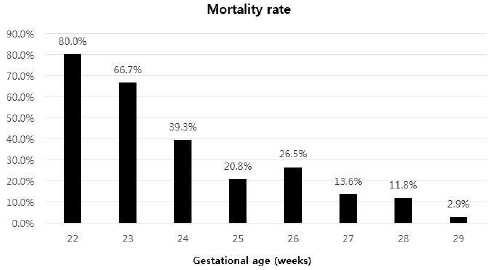
The overall mortality rate was 20.8%. Mortality rate decreased from 21.9% in 2009 to 9.2% in 2012. It then increased and reached a plateau at 20%. Mortality rate was 80.0% in those with GA of 22 weeks. It then decreased with increasing GA. It was 2.9% in those with GA of 29 weeks. The risk of death decreased by 0.573 times when GA increased by 1 week. Death immediately after birth was high in infants with GA of 22 weeks. It was rare in infants with GA ≥25 weeks. Death within 24 hours after birth was high in infants with GA ≤24 weeks who were delivered precipitately without appropriate perinatal support. Sepsis was the leading cause of all deaths. High grade intraventricular hemorrhage was the second common cause of death, especially in infants with GA ≤24 weeks.
CONCLUSION
Mortality rate of preterm infants in this study did not decrease. Modifiable factors including delivery with appropriate supports of neonatal resuscitation team and sufficient maternal obstetric care, especially maternal infection control might reduce mortality, especially immediate postnatal death.
Keyword
MeSH Terms
Figure
Reference
-
1. Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015; 314:1039–1051.
Article2. Kusuda S, Fujimura M, Uchiyama A, Totsu S, Matsunami K. Neonatal Research Network, Japan. Trends in morbidity and mortality among very-low-birth-weight infants from 2003 to 2008 in Japan. Pediatr Res. 2012; 72:531–538.
Article3. Stensvold HJ, Klingenberg C, Stoen R, Moster D, Braekke K, Guthe HJ, et al. Neonatal morbidity and 1-year survival of extremely preterm infants. Pediatrics. 2017; 139:e20161821.
Article4. Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017; 171:e164396.
Article5. Kim JK, Chang YS, Sung S, Park WS. Mortality rate-dependent variations in the survival without major morbidities rate of extremely preterm infants. Sci Rep. 2019; 9:7371.
Article6. Muglia LJ, Katz M. The enigma of spontaneous preterm birth. N Engl J Med. 2010; 362:529–535.
Article7. Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011; 26:467–473.
Article8. Chang YS, Park HY, Park WS. The Korean Neonatal Network: an overview. J Korean Med Sci. 2015; 30(Suppl 1):S3–S11.
Article9. Chung SH, Bae CW. Improvement in the survival rates of very low birth weight infants after the establishment of the Korean Neonatal Network: comparison between the 2000s and 2010s. J Korean Med Sci. 2017; 32:1228–1234.
Article10. Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, et al. Neonatal outcomes of very low birth weight and very preterm neonates: an international comparison. J Pediatr. 2016; 177:144–152.e6.11. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007; 196:147–152.e6.
Article12. Battin MR, Knight DB, Kuschel CA, Howie RN. Improvement in mortality of very low birthweight infants and the changing pattern of neonatal mortality: the 50-year experience of one perinatal centre. J Paediatr Child Health. 2012; 48:596–599.
Article13. World Health Organization. International statistical classification of diseases and related health problems. 10th revision, 2nd ed. Geneva: World Health Organization;2004.14. Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. N Engl J Med. 2015; 372:1801–1811.
Article15. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010; 126:443–456.
Article16. Brumbaugh JE, Hansen NI, Bell EF, Sridhar A, Carlo WA, Hintz SR, et al. Outcomes of extremely preterm infants with birth weight less than 400 g. JAMA Pediatr. 2019; 173:434–445.
Article17. Weiner J, Sharma J, Lantos J, Kilbride H. How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2011; 165:630–634.18. James J, Munson D, DeMauro SB, Langer JC, Dworetz AR, Natarajan G, et al. Outcomes of preterm infants following discussions about withdrawal or withholding of life support. J Pediatr. 2017; 190:118–123.e4.19. Puopolo KM, Mukhopadhyay S, Hansen NI, Cotten CM, Stoll BJ, Sanchez PJ, et al. Identification of extremely premature infants at low risk for early-onset sepsis. Pediatrics. 2017; 140:e20170925.
Article20. Wynn JL, Hansen NI, Das A, Cotten CM, Goldberg RN, Sánchez PJ, et al. Early sepsis does not increase the risk of late sepsis in very low birth weight neonates. J Pediatr. 2013; 162:942–948.e1-3.
Article21. Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017; 390:1770–1780.
Article22. Knowles SJ, O'Sullivan NP, Meenan AM, Hanniffy R, Robson M. Maternal sepsis incidence, aetiology and outcome for mother and fetus: a prospective study. BJOG. 2015; 122:663–671.
Article23. Berlak N, Shany E, Ben-Shimol S, Chertok IA, Goldinger G, Greenberg D, et al. Late onset sepsis: comparison between coagulase-negative staphylococci and other bacteria in the neonatal intensive care unit. Infect Dis (Lond). 2018; 50:764–770.
Article24. Dong Y, Speer CP. Late-onset neonatal sepsis: recent developments. Arch Dis Child Fetal Neonatal Ed. 2015; 100:F257–F263.
Article25. Jeon GW, Sin JB. Successful caspofungin treatment of persistent candidemia in extreme prematurity at 23 and 24 weeks' gestation. J Formos Med Assoc. 2014; 113:191–194.
Article26. de Vries LS, Groenendaal F, Liem KD, Heep A, Brouwer AJ, van't Verlaat E, et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2019; 104:F70–F75.
Article27. Ahn SY, Chang YS, Sung SI, Park WS. Mesenchymal stem cells for severe intraventricular hemorrhage in preterm infants: phase I dose-escalation clinical trial. Stem Cells Transl Med. 2018; 7:847–856.
Article28. Jeon GW. Surfactant preparations for preterm infants with respiratory distress syndrome: past, present, and future. Korean J Pediatr. 2019; 62:155–161.
Article29. Kawai M. Late-onset circulatory collapse of prematurity. Pediatr Int. 2017; 59:391–396.
Article30. Yasuoka K, Inoue H, Egami N, Ochiai M, Tanaka K, Sawano T, et al. Late-onset circulatory collapse and risk of cerebral palsy in extremely preterm infants. J Pediatr. 2019; 212:117–123.
Article31. Helenius K, Sjörs G, Shah PS, Modi N, Reichman B, Morisaki N, et al. Survival in very preterm infants: an international comparison of 10 national neonatal networks. Pediatrics. 2017; 140:e20171264.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deaths in the Neonatal Intensive Care Unit between 2002 and 2014
- Changes in Neonatal Epidemiology during the Last 3 Decades in Korea
- Effects of Antenatal Exposure to Magnesium Sulfate on Neuroprotection in Preterm Infants
- Survival and Cause of Death among Extremely Preterm Infants Near the Limit of Viability
- Comparison of Clinical Manifestation and Prognosis of Preterm and Full-Term Infants with Down Syndrome