J Korean Foot Ankle Soc.
2023 Mar;27(1):30-34. 10.14193/jkfas.2023.27.1.30.
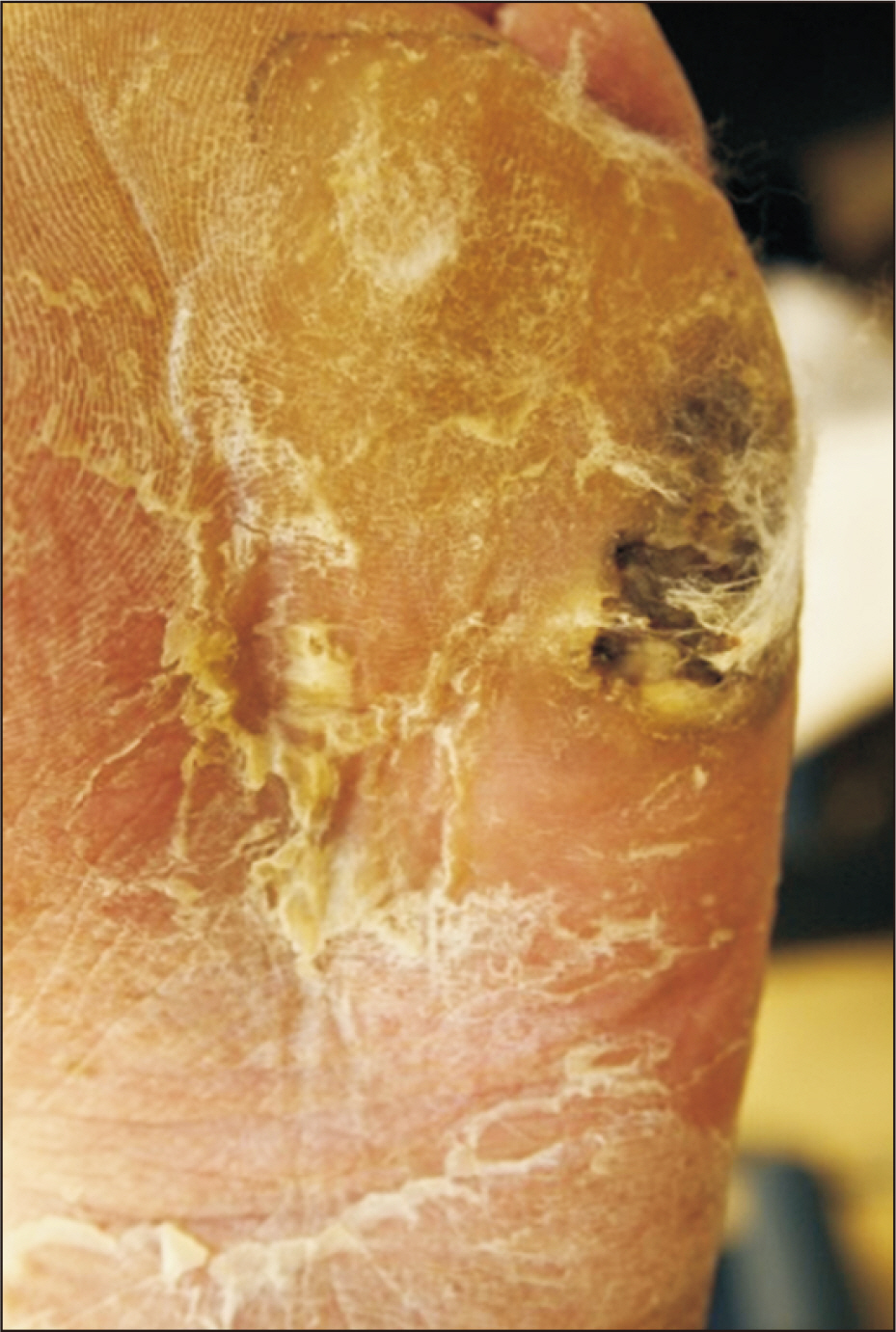
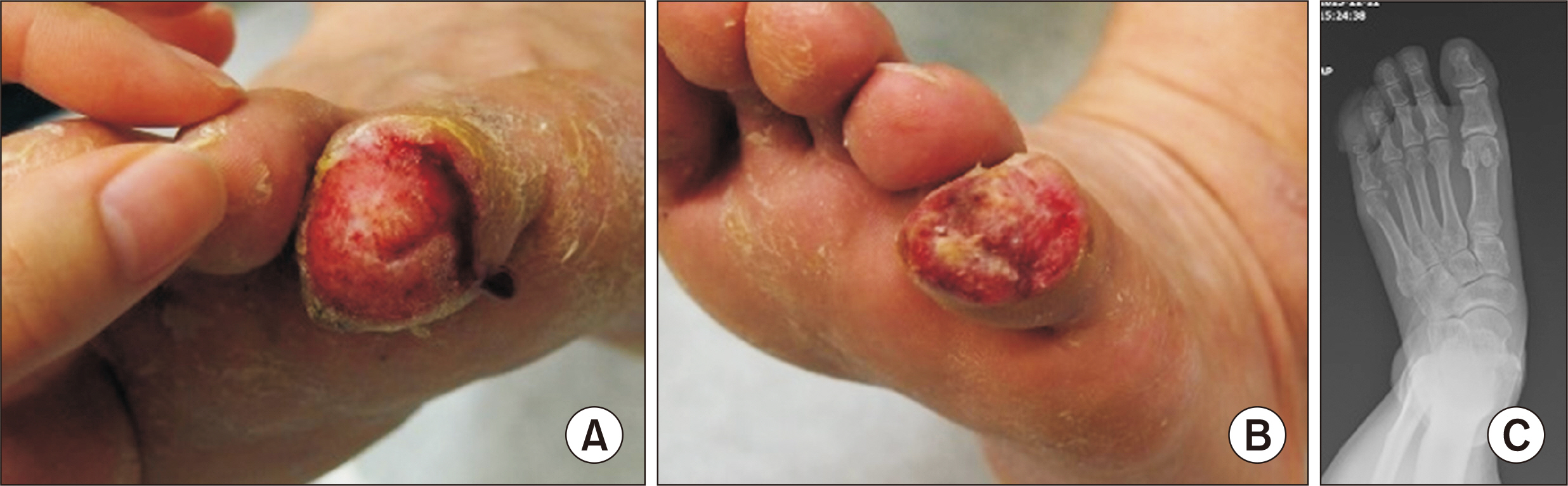
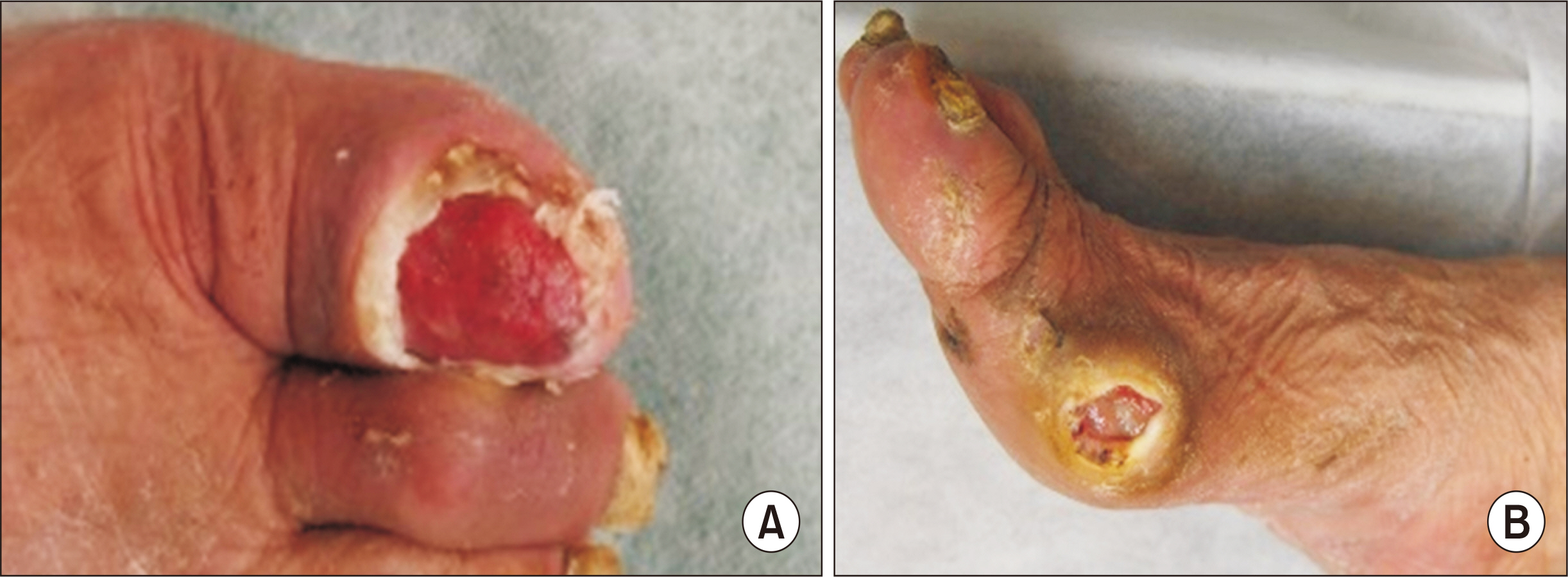
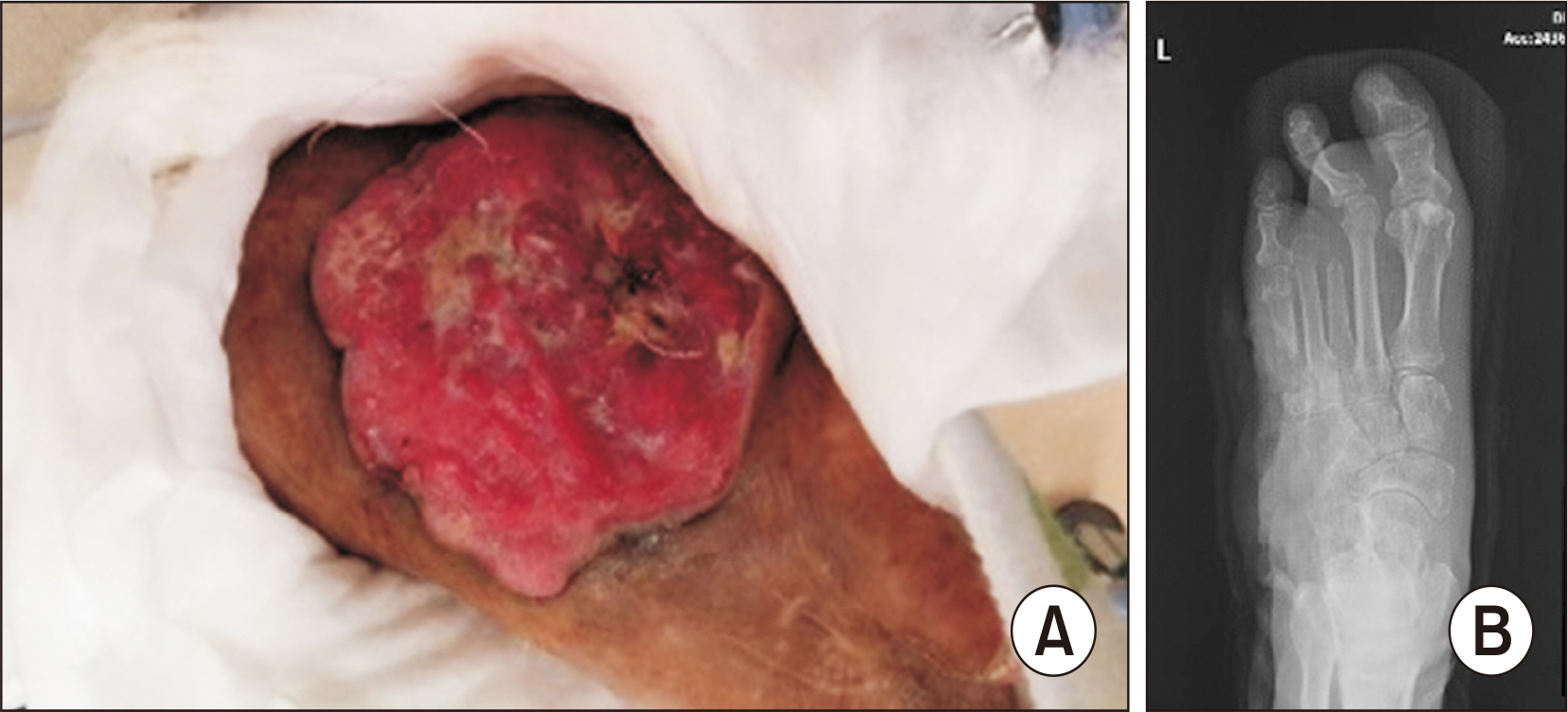
Six Cases of Diabetic Foot Wounds with Concomitant Skin Malignancies
- Affiliations
-
- 1Departments of Orthopedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Departments of General Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Plastic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2540404
- DOI: http://doi.org/10.14193/jkfas.2023.27.1.30
Abstract
- Diabetic foot wounds have a significant effect on the health-related quality of life of patients. As diabetic foot wounds are usually chronic and recurrent, it is possible that they can lead to skin malignancies. Several factors can make it difficult to make an early and accurate diagnosis of skin malignancies of the foot in patients with diabetes mellitus. Even though the prevalence of diabetes mellitus and diabetic foot wounds is increasing, currently there are no guidelines for the biopsy of diabetic foot wounds. We have evolved a criterion for the above based on six cases of diabetic foot wounds with concomitant skin malignancies. We recommend that clinicians should broadly consider implementing this criterion when managing patients with diabetic foot wounds.
Keyword
Figure
Reference
-
1. Moulik PK, Mtonga R, Gill GV. 2003; Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care. 26:491–4. doi: 10.2337/diacare.26.2.491. DOI: 10.2337/diacare.26.2.491. PMID: 12547887.
Article2. Sekhar MS, Thomas RR, Unnikrishnan MK, Vijayanarayana K, Rodrigues GS. 2015; Impact of diabetic foot ulcer on health-related quality of life: a cross-sectional study. Semin Vasc Surg. 28:165–71. doi: 10.1053/j.semvascsurg.2015.12.001. DOI: 10.1053/j.semvascsurg.2015.12.001. PMID: 27113283.
Article3. Armstrong DG, Lavery LA. 1998; Diabetic foot ulcers: prevention, diagnosis and classification. Am Fam Physician. 57:1325–32. 1337–8.4. Mantey I, Foster AV, Spencer S, Edmonds ME. 1999; Why do foot ulcers recur in diabetic patients? Diabet Med. 16:245–9. doi: 10.1046/j.1464-5491.1999.00032.x. DOI: 10.1046/j.1464-5491.1999.00032.x. PMID: 10227571.
Article5. Gerassimidis T, Karkos CD, Karamanos D, Kamparoudis A. 2008; Current endovascular management of the ischaemic diabetic foot. Hippokratia. 12:67–73.6. Muller IS, de Grauw WJ, van Gerwen WH, Bartelink ML, van Den Hoogen HJ, Rutten GE. 2002; Foot ulceration and lower limb amputation in type 2 diabetic patients in dutch primary health care. Diabetes Care. 25:570–4. doi: 10.2337/diacare.25.3.570. DOI: 10.2337/diacare.25.3.570. PMID: 11874949.
Article7. Stratigos A, Garbe C, Lebbe C, Malvehy J, del Marmol V, Pehamberger H, et al. 2015; Diagnosis and treatment of invasive squamous cell carcinoma of the skin: European consensus-based interdisciplinary guideline. Eur J Cancer. 51:1989–2007. doi: 10.1016/j.ejca.2015.06.110. DOI: 10.1016/j.ejca.2015.06.110. PMID: 26219687.
Article8. Fleming ID, Barnawell JR, Burlison PE, Rankin JS. 1975; Skin cancer in black patients. Cancer. 35:600–5. doi: 10.1002/1097-0142(197503)35:3<600::aid-cncr2820350309>3.0.co;2-3. DOI: 10.1002/1097-0142(197503)35:3<600::AID-CNCR2820350309>3.0.CO;2-3. PMID: 1111931.
Article9. Metzger S, Ellwanger U, Stroebel W, Schiebel U, Rassner G, Fierlbeck G. 1998; Extent and consequences of physician delay in the diagnosis of acral melanoma. Melanoma Res. 8:181–6. doi: 10.1097/00008390-199804000-00014. DOI: 10.1097/00008390-199804000-00014. PMID: 9610874.
Article10. Boulton AJ. 2004; The diabetic foot: from art to science. The 18th Camillo Golgi lecture. Diabetologia. 47:1343–53. doi: 10.1007/s00125-004-1463-y. DOI: 10.1007/s00125-004-1463-y. PMID: 15309286.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diabetic Foot Wounds with Concomitant Skin Malignancies
- Diabetic Foot Education and a Diabetic Foot Screening Tool
- Skin Graft Remains a Clinically Good Treatment Strategy for Chronic Diabetic Wounds of the Foot and Ankle
- The Effectiveness of Home Treatment with Nanocrystalline Silver Product (Acticoat(TM)) on the Chronic Ulcerative Lesion of Foot
- Surgical Treatment of Diabetic Foot Disease