Ann Surg Treat Res.
2023 Feb;104(2):101-108. 10.4174/astr.2023.104.2.101.
Clinical outcomes of gastric cancer surgery after liver transplantation
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 2Division of Gastrointestinal Surgery, Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 3Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Surgery, Al-Noor Specialist Hospital, Makkah, Saudi Arabia
- 5Department of Surgery, Gachon University Gil Medical Center, Incheon, Korea
- 6Division of Hepatobiliary Surgery, Department of Surgery, Seoul National University Hospital, Seoul, Korea
- KMID: 2539224
- DOI: http://doi.org/10.4174/astr.2023.104.2.101
Abstract
- Purpose
De novo malignancy is common after liver transplantation (LT); however, there are limited reports on the clinical outcomes of gastric cancer surgery after LT. Our study aimed to investigate the feasibility and safety of gastric cancer surgery after LT.
Methods
Seventeen patients underwent gastric cancer surgery after LT at a single institution between January 2013 and June 2021. We retrospectively collected data on surgical complications, survival, and recurrence status of these cases.
Results
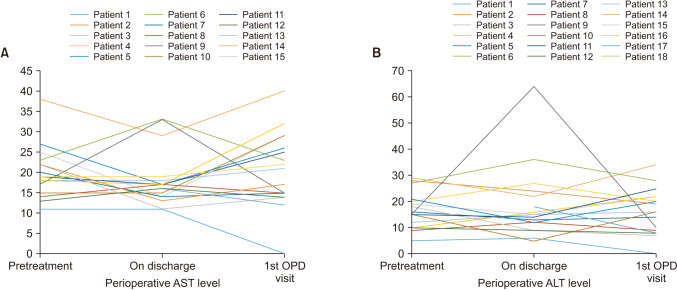
Fifteen patients (88.2%) underwent curative gastrectomy, with 10 open distal (66.7%) and 5 laparoscopic distal (33.3%) gastrectomies. Surgical and severe complication rates were 3 of 15 (20.0%) and 1 of 15 (6.7%), respectively. There were no significant differences between laparoscopic (33.3%) and open surgery (66.7%) in terms of operation time and complication rate. No surgery-related mortalities occurred. Immunosuppressants could be maintained without difficulty, and no suspicious acute rejection was identified during the perioperative period. There was 1 recurrence after curative surgery (recurrence rate, 6.7%), and the 5-year cancer-specific survival rate after curative surgery was 93.3%.
Conclusion
Laparoscopic gastrectomy can be safely done even after LT in terms of postoperative complications and graft safety.
Figure
Cited by 2 articles
-
De novo gastric cancer after liver transplantation: A review of the Asian experience
Cheon-Soo Park, Yong-Kyu Chung
Ann Liver Transplant. 2023;3(1):1-5. doi: 10.52604/alt.23.0006.Surveillance and management of de novo malignancy after liver transplantation
Woo-Hyoung Kang
Ann Liver Transplant. 2024;4(1):10-15. doi: 10.52604/alt.24.0006.
Reference
-
1. Baccarani U, Adani GL, Serraino D, Lorenzin D, Gambato M, Buda A, et al. De novo tumors are a major cause of late mortality after orthotopic liver transplantation. Transplant Proc. 2009; 41:1303–1305. PMID: 19460546.2. Fung JJ, Jain A, Kwak EJ, Kusne S, Dvorchik I, Eghtesad B. De novo malignancies after liver transplantation: a major cause of late death. Liver Transpl. 2001; 7(11 Suppl 1):S109–S118. PMID: 11689783.3. Kim S, Rovgaliyev B, Lee JM, Lee KW, Hong SK, Cho JH, et al. Clinical significance of de novo malignancy after liver transplant: a single-center study. Transplant Proc. 2021; 53:200–206. PMID: 32409224.4. Park HW, Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, et al. De novo malignancies after liver transplantation: incidence comparison with the Korean Cancer Registry. Transplant Proc. 2012; 44:802–805. PMID: 22483500.5. Gong CS, Yoo MW, Kim BS, Hwang S, Kim KH, Yook JH, et al. De novo gastric cancer after liver transplantation. Ann Transplant. 2016; 21:386–391. PMID: 27334929.6. Kim HH, Han SU, Kim MC, Kim W, Lee HJ, Ryu SW, et al. Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage i gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol. 2019; 5:506–513. PMID: 30730546.7. Lee MS, Kim EY, Lee JH, Jee YS, Park DJ, Kim HH, et al. Laparoscopy-assisted distal gastrectomy for gastric cancer after liver transplantation. J Korean Surg Soc. 2011; 80 Suppl 1(Suppl 1):S1–S5. PMID: 22066074.8. Park EY, Park DJ, Park HW, Nam CW, Nah YW, Kim GY. Totally laparoscopic distal gastrectomy in post liver transplant patient. J Minim Invasive Surg. 2019; 22:39–42. PMID: 35601701.9. Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, et al. Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol. 2020; 38:3304–3313. PMID: 32816629.10. Lee KG, Lee HJ, Yang JY, Oh SY, Bard S, Suh YS, et al. Risk factors associated with complication following gastrectomy for gastric cancer: retrospective analysis of prospectively collected data based on the Clavien-Dindo system. J Gastrointest Surg. 2014; 18:1269–1277. PMID: 24820136.11. Information Committee of the Korean Gastric Cancer Association. Korean gastric cancer association-led nationwide survey on surgically treated gastric cancers in 2019. J Gastric Cancer. 2021; 21:221–235. PMID: 34691807.12. Curet MJ. Special problems in laparoscopic surgery: previous abdominal surgery, obesity, and pregnancy. Surg Clin North Am. 2000; 80:1093–1110. PMID: 10987026.13. Lee KW, Seo YD, Oh SC, Suh SW, Jeong J, Kim H, et al. What is the best immune-suppressant combination in terms of antitumor effect in hepatocellular carcinoma? Hepatol Res. 2016; 46:593–600. PMID: 26348114.14. Charlton M, Levitsky J, Aqel B, O’Grady J, Hemibach J, Rinella M, et al. International liver transplantation society consensus statement on immunosuppression in liver transplant recipients. Transplantation. 2018; 102:727–743. PMID: 29485508.15. Finkenstedt A, Graziadei IW, Oberaigner W, Hilbe W, Nachbaur K, Mark W, et al. Extensive surveillance promotes early diagnosis and improved survival of de novo malignancies in liver transplant recipients. Am J Transplant. 2009; 9:2355–2361. PMID: 19663894.16. Herrero JI, Alegre F, Quiroga J, Pardo F, Iñarrairaegui M, Sangro B, et al. Usefulness of a program of neoplasia surveillance in liver transplantation: a preliminary report. Clin Transplant. 2009; 23:532–536. PMID: 19681977.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- De novo gastric cancer after liver transplantation: A review of the Asian experience
- Pediatric liver transplantation in Korea: long-term outcomes and allocations
- Totally Laparoscopic Distal Gastrectomy in Post Liver Transplant Patient
- Pediatric Liver Transplantation
- Surgical Outcomes of Patients Undergoing Gastrectomy for Gastric Cancer: Does the Age Matter?