Ann Surg Treat Res.
2023 Feb;104(2):71-79. 10.4174/astr.2023.104.2.71.
Domestic medical travel from non-Seoul regions to Seoul for initial breast cancer treatment: a nationwide cohort study
- Affiliations
-
- 1Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2539221
- DOI: http://doi.org/10.4174/astr.2023.104.2.71
Abstract
- Purpose
This study was conducted to investigate the trend of domestic medical travel from non-Seoul areas to Seoul for initial breast cancer treatment, and identify factors associated with medical travel in breast cancer patients.
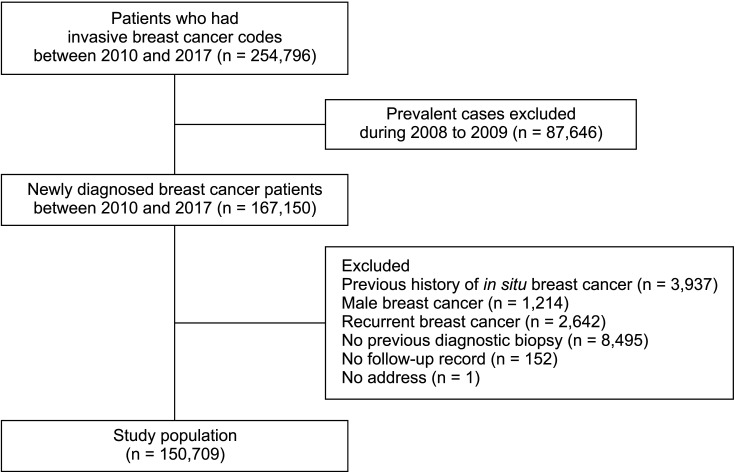
Methods
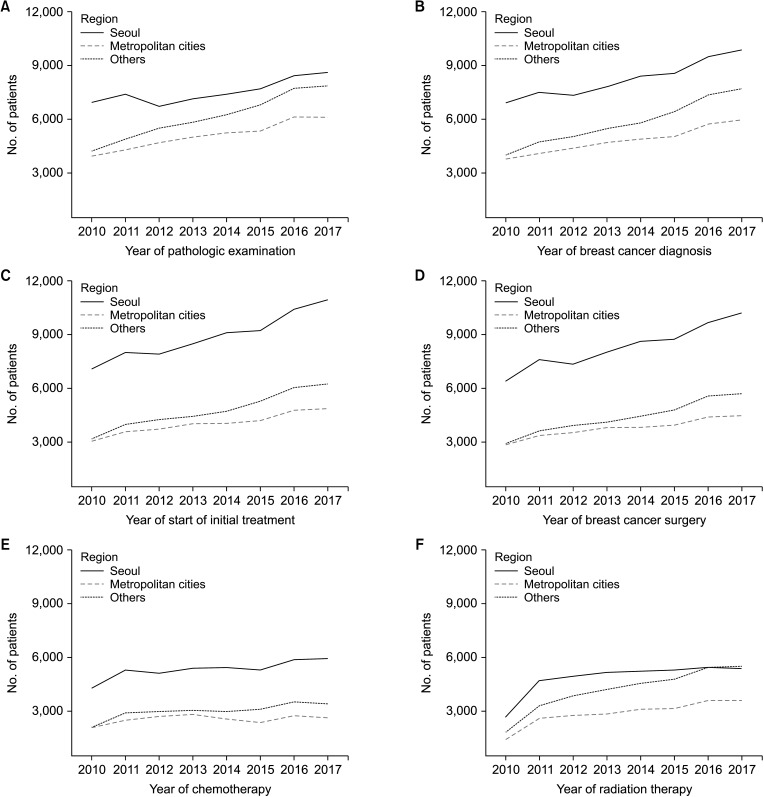
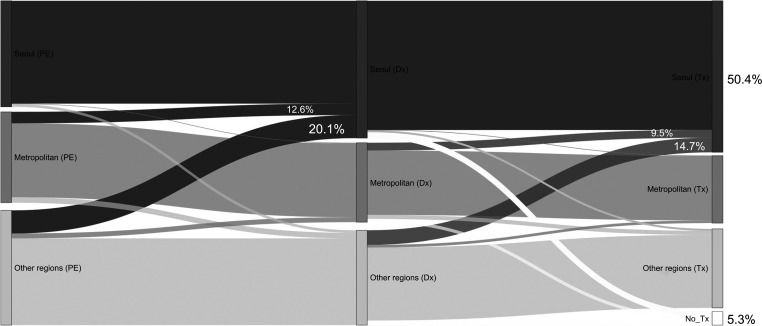
A nationwide retrospective cohort study was performed using the Health Insurance Review and Assessment data of South Korea. Patients were classified according to the regions in which they underwent breast biopsy (Seoul vs.metropolitan cities vs. other regions). Frequencies of biopsy, diagnosis, treatment, and domestic medical travel were analyzed according to regions, and factors associated with medical travel were investigated.
Results
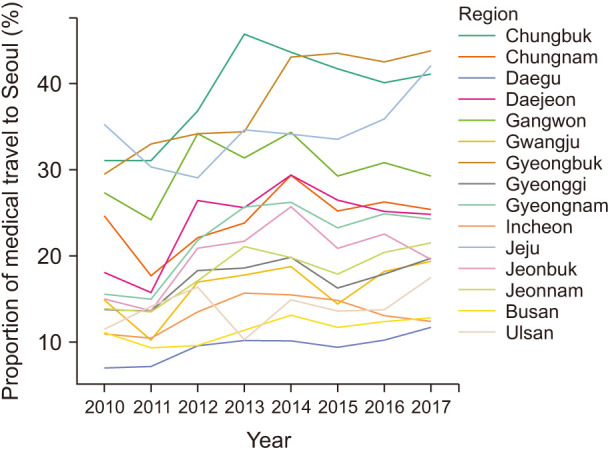
A total of 150,709 breast cancer survivors who were diagnosed between January 2010 and December 2017 were included. The total rate of medical travel from non-Seoul regions to Seoul had increased from 14.2% (1,161 of 8,150) in 2010 to 19.8% (2,762 of 13,964) in 2017. Approximately a quarter of patients from other regions traveled to Seoul, and over 40% of patients from Chungbuk, Gyeongbuk, and Jeju regions traveled to Seoul for initial treatment in 2017. The difference in the annual frequencies of upfront surgery between Seoul and non-Seoul regions increased over time. Younger age and regions other than metropolitan cities were significantly related to medical travel. Patients covered by medical aid or past medical histories were significantly less likely to travel to Seoul for initial breast cancer treatment.
Conclusion
Medical travel to Seoul for upfront breast cancer surgery is increasing. Policies for appropriate healthcare delivery need to be established in the near future.
Keyword
Figure
Cited by 1 articles
-
Implementation of BRCA Test among Young Breast Cancer Patients in South Korea: A Nationwide Cohort Study
Yung-Huyn Hwang, Tae-Kyung Yoo, Sae Byul Lee, Jisun Kim, Beom Seok Ko, Hee Jeong Kim, Jong Won Lee, Byung Ho Son, Il Yong Chung
Cancer Res Treat. 2024;56(3):802-808. doi: 10.4143/crt.2023.1186.
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID: 30207593.2. Hinson AM, Hohmann SF, Stack BC. Domestic travel and regional migration for parathyroid surgery among patients receiving care at academic medical centers in the United States, 2012-2014. JAMA Otolaryngol Head Neck Surg. 2016; 142:641–647. PMID: 27124618.3. Kang SY, Kim YS, Kim Z, Kim HY, Kim HJ, Park S, et al. Breast cancer statistics in Korea in 2017: data from a breast cancer registry. J Breast Cancer. 2020; 23:115–128. PMID: 32395372.4. Chung IY, Lee J, Park S, Lee JW, Youn HJ, Hong JH, et al. Nationwide analysis of treatment patterns for Korean breast cancer survivors using National Health Insurance Service data. J Korean Med Sci. 2018; 33:e276. PMID: 30369858.5. Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet. 1999; 353:1119–1126. PMID: 10209974.6. Yun YH, Kim YA, Min YH, Park S, Won YJ, Kim DY, et al. The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol. 2012; 23:2731–2737. PMID: 22553194.7. Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, et al. Time to surgery and breast cancer survival in the United States. JAMA Oncol. 2016; 2:330–339. PMID: 26659430.8. Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009; 27:4671–4678. PMID: 19720926.9. Shalowitz DI, Nivasch E, Burger RA, Schapira MM. Are patients willing to travel for better ovarian cancer care? Gynecol Oncol. 2018; 148:42–48. PMID: 29079037.10. Xu Z, Aquina CT, Justiniano CF, Becerra AZ, Boscoe FP, Schymura MJ, et al. Centralizing rectal cancer surgery: what is the impact of travel on patients? Dis Colon Rectum. 2020; 63:319–325. PMID: 32045397.11. Park S, Park IK, Kim ER, Hwang Y, Lee HJ, Kang CH, et al. Current trends of lung cancer surgery and demographic and social factors related to changes in the trends of lung cancer surgery: an analysis of the national database from 2010 to 2014. Cancer Res Treat. 2017; 49:330–337. PMID: 27456943.12. Hong NS, Lee KS, Kam S, Choi GS, Kwon OK, Ryu DH, et al. A survival analysis of gastric or colorectal cancer patients treated with surgery: comparison of capital and a non-capital city. J Prev Med Public Health. 2017; 50:283–293. PMID: 29020762.13. Kim JH, Kim SY, Yun SJ, Chung JI, Choi H, Yu HS, et al. Medical travel among non-Seoul residents to seek prostate cancer treatment in medical facilities of Seoul. Cancer Res Treat. 2019; 51:53–64. PMID: 29458236.14. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–728. PMID: 28378543.15. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43:1130–1139. PMID: 16224307.16. Song H, Fang F, Valdimarsdóttir U, Lu D, Andersson TM, Hultman C, et al. Waiting time for cancer treatment and mental health among patients with newly diagnosed esophageal or gastric cancer: a nationwide cohort study. BMC Cancer. 2017; 17:2. PMID: 28049452.17. Lohrisch C, Paltiel C, Gelmon K, Speers C, Taylor S, Barnett J, et al. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006; 24:4888–4894. PMID: 17015884.18. Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH. Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol. 2016; 2:322–329. PMID: 26659132.19. Ho PJ, Cook AR, Binte Mohamed Ri NK, Liu J, Li J, Hartman M. Impact of delayed treatment in women diagnosed with breast cancer: a population-based study. Cancer Med. 2020; 9:2435–2444. PMID: 32053293.20. Lamont EB, Hayreh D, Pickett KE, Dignam JJ, List MA, Stenson KM, et al. Is patient travel distance associated with survival on phase II clinical trials in oncology? J Natl Cancer Inst. 2003; 95:1370–1375. PMID: 13130112.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Waiting Time for Breast Cancer Treatment in Korea: A Nationwide Cohort Study
- Implementation of BRCA Test among Young Breast Cancer Patients in South Korea: A Nationwide Cohort Study
- Age-Period-Cohort Analysis of Female Breast Cancer Mortality in Korea
- Marked Reduction in the Risk of Dementia in Patients with Breast Cancer: A Nationwide Population-Based Cohort Study
- Nationwide Korean Breast Cancer Data of 2004 Using Breast Cancer Registration Program