Intest Res.
2023 Jan;21(1):100-109. 10.5217/ir.2021.00110.
Improvement of ulcerative colitis control by searching and restricting of inflammatory trigger factors in daily clinical practice
- Affiliations
-
- 1Division of Colon and Rectal Surgery, Chang Gung Memorial Hospital, Linkou, Taoyuan, Taiwan, Republic of China
- 2School of Medicine, Chang Gung University, Taoyuan, Taiwan, Republic of China
- KMID: 2539009
- DOI: http://doi.org/10.5217/ir.2021.00110
Abstract
- Background/Aims
Exacerbating factors of ulcerative colitis (UC) are multiple and complex with individual influence. We aimed to evaluate the efficacy of disease control by searching and restricting inflammation trigger factors of UC relapse individually in daily clinical practice.
Methods
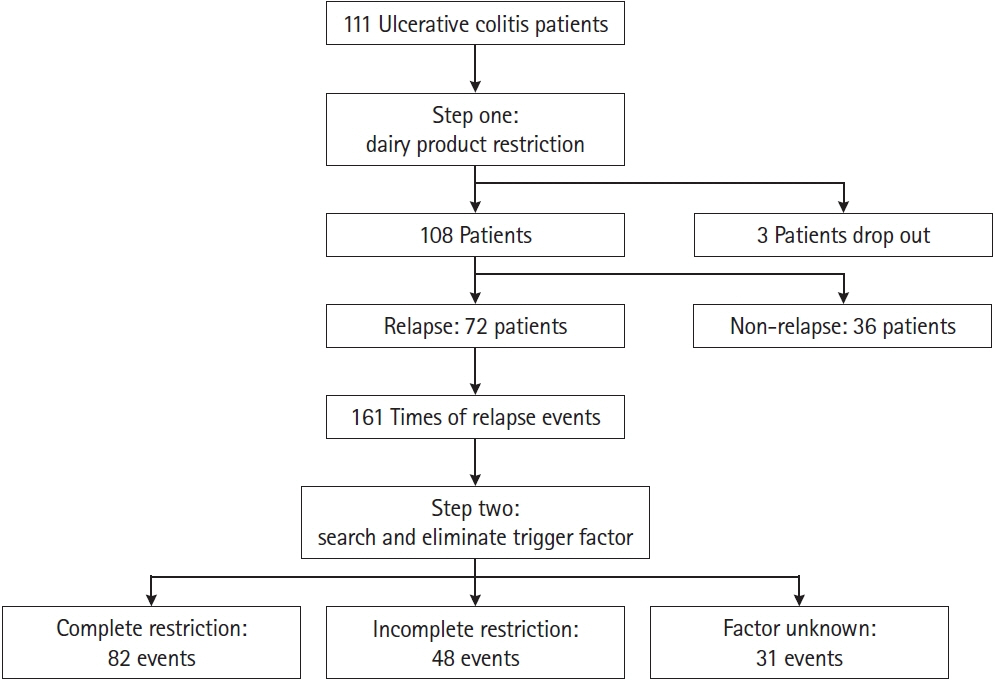
Both patients with UC history or new diagnosis were asked to avoid dairy products at first doctor visit. Individual-reported potential trigger factors were restricted when UC flared up (Mayo endoscopy score ≥1) from remission status. The remission rate, duration to remission and medication were analyzed between the groups of factor restriction complete, incomplete and unknown.
Results
The total remission rate was 91.7% of 108 patients with complete restriction of dairy product. The duration to remission of UC history group was significantly longer than that of new diagnosis group (88.5 days vs. 43.4 days, P=0.006) in patients with initial endoscopic score 2–3, but no difference in patients with score 1. After first remission, the inflammation trigger factors in 161 relapse episodes of 72 patients were multiple and personal. Milk/dairy products, herb medicine/Chinese tonic food and dietary supplement were the common factors, followed by psychological issues, non-dietary factors (smoking cessation, cosmetic products) and discontinuation of medication by patients themselves. Factor unknown accounted for 14.1% of patients. The benefits of factor complete restriction included shorter duration to remission (P<0.001), less steroid and biological agent use (P=0.022) when compared to incomplete restriction or factor unknown group.
Conclusions
Restriction of dairy diet first then searching and restricting trigger factors personally if UC relapse can improve the disease control and downgrade the medication usage of UC patients in daily clinical practice.
Figure
Reference
-
1. Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011; 365:1713–1725.
Article2. Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017; 11:649–670.
Article3. Kuo CJ, Yu KH, See LC, et al. The trend of inflammatory bowel diseases in Taiwan: a population-based study. Dig Dis Sci. 2015; 60:2454–2462.
Article4. Wei SC, Chang TA, Chao TH, et al. Management of ulcerative colitis in Taiwan: consensus guideline of the Taiwan Society of Inflammatory Bowel Disease. Intest Res. 2017; 15:266–284.
Article5. Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet. 2017; 389:1756–1770.
Article6. Geerling BJ, Dagnelie PC, Badart-Smook A, Russel MG, Stockbrügger RW, Brummer RJ. Diet as a risk factor for the development of ulcerative colitis. Am J Gastroenterol. 2000; 95:1008–1013.
Article7. Hou JK, Abraham B, El-Serag H. Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol. 2011; 106:563–573.
Article8. Levine A, Sigall Boneh R, Wine E. Evolving role of diet in the pathogenesis and treatment of inflammatory bowel diseases. Gut. 2018; 67:1726–1738.
Article9. Chiba M, Nakane K, Komatsu M. Westernized diet is the most ubiquitous environmental factor in inflammatory bowel disease. Perm J. 2019; 23:18–107.
Article10. Witkowski M, Witkowski M, Gagliani N, Huber S. Recipe for IBD: can we use food to control inflammatory bowel disease? Semin Immunopathol. 2018; 40:145–156.
Article11. Truelove SC. Ulcerative colitis provoked by milk. Br Med J. 1961; 1:154–160.
Article12. Lee MS, Wahlqvist ML, Peng CJ. Dairy foods and health in Asians: Taiwanese considerations. Asia Pac J Clin Nutr. 2015; 24 Suppl 1:S14–S20.13. Kitahora T, Utsunomiya T, Yokota A. Epidemiological study of ulcerative colitis in Japan: incidence and familial occurrence. The Epidemiology Group of the Research Committee of Inflammatory Bowel Disease in Japan. J Gastroenterol. 1995; 30 Suppl 8:5–8.14. Brasil Lopes M, Rocha R, Castro Lyra A, et al. Restriction of dairy products: a reality in inflammatory bowel disease patients. Nutr Hosp. 2014; 29:575–581.15. Limdi JK. Dietary practices and inflammatory bowel disease. Indian J Gastroenterol. 2018; 37:284–292.
Article16. Hou JK, Lee D, Lewis J. Diet and inflammatory bowel disease: review of patient-targeted recommendations. Clin Gastroenterol Hepatol. 2014; 12:1592–1600.
Article17. Keshteli AH, Madsen KL, Dieleman LA. Diet in the pathogenesis and management of ulcerative colitis: a review of randomized controlled dietary interventions. Nutrients. 2019; 11:1498.
Article18. Rizzello F, Spisni E, Giovanardi E, et al. Implications of the westernized diet in the onset and progression of IBD. Nutrients. 2019; 11:1033.
Article19. Limdi JK, Aggarwal D, McLaughlin JT. Dietary practices and beliefs in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016; 22:164–170.
Article20. Yoon JY. Nutritional approach as therapeutic manipulation in inflammatory bowel disease. Intest Res. 2019; 17:463–475.
Article21. Inns SJ, Emmanuel AV. Survey of UK and New Zealand gastroenterologists’ practice regarding dietary advice and food exclusion in irritable bowel syndrome and inflammatory bowel disease. Frontline Gastroenterol. 2013; 4:44–50.
Article22. Limketkai BN, Iheozor-Ejiofor Z, Gjuladin-Hellon T, et al. Dietary interventions for induction and maintenance of remission in inflammatory bowel disease. Cochrane Database Syst Rev. 2019; 2:CD012839.
Article23. Martin TD, Chan SS, Hart AR. Environmental factors in the relapse and recurrence of inflammatory bowel disease: a review of the literature. Dig Dis Sci. 2015; 60:1396–1405.
Article24. Vedamurthy A, Ananthakrishnan AN. Influence of environmental factors in the development and outcomes of inflammatory bowel disease. Gastroenterol Hepatol (NY). 2019; 15:72–82.25. Tomar SK, Kedia S, Upadhyay AD, et al. Impact of dietary beliefs and practices on patients with inflammatory bowel disease: an observational study from India. JGH Open. 2017; 1:15–21.
Article26. Gkikas K, Gerasimidis K, Milling S, Ijaz UZ, Hansen R, Russell RK. Dietary strategies for maintenance of clinical remission in inflammatory bowel diseases: are we there yet? Nutrients. 2020; 12:2018.
Article27. Llewellyn SR, Britton GJ, Contijoch EJ, et al. Interactions between diet and the intestinal microbiota alter intestinal permeability and colitis severity in mice. Gastroenterology. 2018; 154:1037–1046.
Article28. Wright R, Truelove SC. A controlled therapeutic trial of various diets in ulcerative colitis. Br Med J. 1965; 2:138–141.
Article29. Jowett SL, Seal CJ, Pearce MS, et al. Influence of dietary factors on the clinical course of ulcerative colitis: a prospective cohort study. Gut. 2004; 53:1479–1484.
Article30. Strisciuglio C, Giannetti E, Martinelli M, Sciorio E, Staiano A, Miele E. Does cow’s milk protein elimination diet have a role on induction and maintenance of remission in children with ulcerative colitis? Acta Paediatr. 2013; 102:e273–e278.
Article31. Kurata JH. Dietary and other risk factors of ulcerative colitis: a case-control study in Japan. Epidemiology Group of the Research Committee of Inflammatory Bowel Disease in Japan. J Clin Gastroenterol. 1994; 19:166–171.32. Chassaing B, Koren O, Goodrich JK, et al. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature. 2015; 519:92–96.
Article33. Lecomte M, Couëdelo L, Meugnier E, et al. Dietary emulsifiers from milk and soybean differently impact adiposity and inflammation in association with modulation of colonic goblet cells in high-fat fed mice. Mol Nutr Food Res. 2016; 60:609–620.
Article34. Bhattacharyya S, Shumard T, Xie H, et al. A randomized trial of the effects of the no-carrageenan diet on ulcerative colitis disease activity. Nutr Healthy Aging. 2017; 4:181–192.
Article35. Triantafyllidi A, Xanthos T, Papalois A, Triantafillidis JK. Herbal and plant therapy in patients with inflammatory bowel disease. Ann Gastroenterol. 2015; 28:210–220.36. Torres J, Ellul P, Langhorst J, et al. European Crohn’s and Colitis Organisation topical review on complementary medicine and psychotherapy in inflammatory bowel disease. J Crohns Colitis. 2019; 13:673–685e.
Article37. Gubatan J, Mitsuhashi S, Zenlea T, Rosenberg L, Robson S, Moss AC. Low serum vitamin D during remission increases risk of clinical relapse in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2017; 15:240–246.
Article38. Lang A, Salomon N, Wu JC, et al. Curcumin in combination with mesalamine induces remission in patients with mild-tomoderate ulcerative colitis in a randomized controlled trial. Clin Gastroenterol Hepatol. 2015; 13:1444–1449.
Article39. Dhillon P, Singh K. Therapeutic applications of probiotics in ulcerative colitis: an updated review. Pharma Nutrition. 2020; 13:100194.
Article40. Iheozor-Ejiofor Z, Kaur L, Gordon M, Baines PA, Sinopoulou V, Akobeng AK. Probiotics for maintenance of remission in ulcerative colitis. Cochrane Database Syst Rev. 2020; 3:CD007443.
Article41. Magee EA, Edmond LM, Tasker SM, Kong SC, Curno R, Cummings JH. Associations between diet and disease activity in ulcerative colitis patients using a novel method of data analysis. Nutr J. 2005; 4:7.
Article42. Gibney MJ. Ultra-processed foods: definitions and policy issues. Curr Dev Nutr. 2018; 3–nzy077.
Article43. Monteiro CA, Cannon G, Levy RB, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019; 22:936–941.
Article44. Mikocka-Walus A, Knowles SR, Keefer L, Graff L. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2016; 22:752–762.45. Neuendorf R, Harding A, Stello N, Hanes D, Wahbeh H. Depression and anxiety in patients with Inflammatory Bowel Disease: a systematic review. J Psychosom Res. 2016; 87:70–80.
Article46. Vogelaar L, van’t Spijker A, Timman R, et al. Fatigue management in patients with IBD: a randomised controlled trial. Gut. 2014; 63:911–918.
Article47. Ali T, Madhoun MF, Orr WC, Rubin DT. Assessment of the relationship between quality of sleep and disease activity in inflammatory bowel disease patients. Inflamm Bowel Dis. 2013; 19:2440–2443.
Article48. Bernstein MT, Targownik LE, Sexton KA, Graff LA, Miller N, Walker JR. Assessing the relationship between sources of stress and symptom changes among persons with IBD over time: a prospective study. Can J Gastroenterol Hepatol. 2016; 2016:1681507.
Article49. Bernstein CN, Singh S, Graff LA, Walker JR, Miller N, Cheang M. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010; 105:1994–2002.
Article50. Annaházi A, Molnár T. Optimal endpoint of therapy in IBD: an update on factors determining a successful drug withdrawal. Gastroenterol Res Pract. 2015; 2015:832395.
Article51. Beaugerie L, Massot N, Carbonnel F, Cattan S, Gendre JP, Cosnes J. Impact of cessation of smoking on the course of ulcerative colitis. Am J Gastroenterol. 2001; 96:2113–2116.
Article52. Jiang L, Xia B, Li J, et al. Risk factors for ulcerative colitis in a Chinese population: an age-matched and sex-matched casecontrol study. J Clin Gastroenterol. 2007; 41:280–284.53. Cornish JA, Tan E, Simillis C, Clark SK, Teare J, Tekkis PP. The risk of oral contraceptives in the etiology of inflammatory bowel disease: a meta-analysis. Am J Gastroenterol. 2008; 103:2394–2400.
Article54. Khalili H, Higuchi LM, Ananthakrishnan AN, et al. Hormone therapy increases risk of ulcerative colitis but not Crohn’s disease. Gastroenterology. 2012; 143:1199–1206.
Article