J Neurocrit Care.
2022 Dec;15(2):104-112. 10.18700/jnc.220054.
Failed recanalization mediates the association of women with poor outcomes after thrombectomy: a single-center experience
- Affiliations
-
- 1Department of Neurology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 2Department of Biostatistics, Clinical Trial Center, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- KMID: 2538767
- DOI: http://doi.org/10.18700/jnc.220054
Abstract
- Background
Whether thrombectomy benefits differ according to sex remains debatable. We aimed to investigate whether there was a difference in stroke outcomes between men and women treated with thrombectomy.
Methods
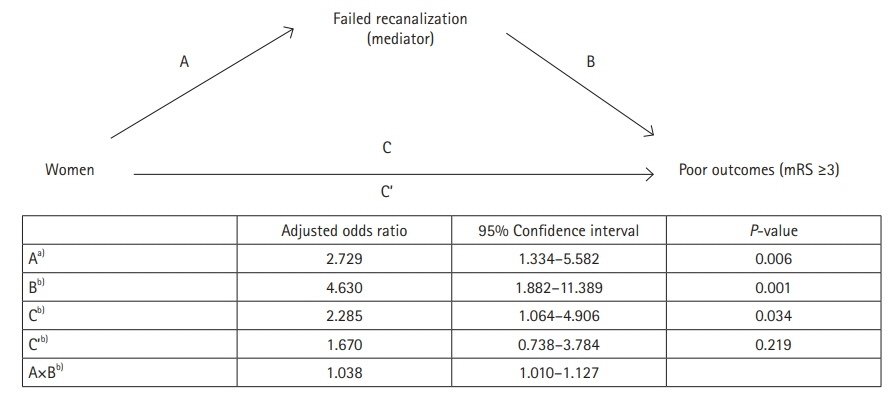
We studied 173 patients with anterior circulation strokes. Failed recanalization was defined as thrombolysis in cerebral infarction grade 0-2a. Scores >2 on the modified Rankin Scale at 3 months were regarded as poor outcomes. To prove that failed recanalization mediated the association between sex differences and functional outcome, the four steps of the reasoning process adapted from Baron and Kenny’s causal-steps approach were tested. The adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were calculated.
Results
This study included 76 women and 97 men. Women were older and presented with atrial fibrillation more frequently than men. Female sex was independently associated with failed recanalization (aOR, 2.729; 95% CI, 1.334–5.582), which was an independent predictor of poor outcomes (aOR, 4.630; 95% CI, 1.882–11.389). Women were associated with poor outcomes in the analysis adjusted for confounders, except for failed recanalization (aOR, 2.285; 95% CI, 1.064–4.906). However, the association became insignificant in the additional analysis adjusted for failed recanalization (aOR, 1.670; 95% CI, 0.738–3.784). The indirect effect between female sex and poor outcomes via failed recanalization was statistically significant (aOR, 1.038; 95% CI, 1.010–1.127).
Conclusion
Our study showed that failed recanalization mediated the association between women and poor outcomes after thrombectomy. Nonetheless, this might be explained by chance given our limited study population.
Keyword
Figure
Reference
-
1. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–95.
Article2. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.3. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–30.
Article4. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.5. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–18.
Article6. Chalos V, de Ridder IR, Lingsma HF, Brown S, van Oostenbrugge RJ, Goyal M, et al. Does sex modify the effect of endovascular treatment for ischemic stroke? Stroke. 2019; 50:2413–9.
Article7. Sheth SA, Lee S, Warach SJ, Gralla J, Jahan R, Goyal M, et al. Sex differences in outcome after endovascular stroke therapy for acute ischemic stroke. Stroke. 2019; 50:2420–7.
Article8. de Ridder IR, Fransen PS, Beumer D, Berkhemer OA, van den Berg LA, Wermer MJ, et al. Is intra-arterial treatment for acute ischemic stroke less effective in women than in men? Interv Neurol. 2016; 5:174–8.
Article9. Dula AN, Mlynash M, Zuck ND, Albers GW, Warach SJ; DEFUSE 3 Investigators. Neuroimaging in ischemic stroke is different between men and women in the DEFUSE 3 cohort. Stroke. 2020; 51:481–8.
Article10. Carvalho A, Cunha A, Gregório T, Paredes L, Costa H, Veloso M, et al. Is the efficacy of endovascular treatment for acute ischemic stroke sex-related. Interv Neurol. 2018; 7:42–7.
Article11. Deb-Chatterji M, Schlemm E, Flottmann F, Meyer L, Alegiani A, Brekenfeld C, et al. Sex differences in outcome after thrombectomy for acute ischemic stroke are explained by confounding factors. Clin Neuroradiol. 2021; 31:1101–9.
Article12. Madsen TE, DeCroce-Movson E, Hemendinger M, McTaggart RA, Yaghi S, Cutting S, et al. Sex differences in 90-day outcomes after mechanical thrombectomy for acute ischemic stroke. J Neurointerv Surg. 2019; 11:221–5.
Article13. Ko SB, Park HK, Kim BM, Heo JH, Rha JH, Kwon SU, et al. 2019 Update of the Korean clinical practice guidelines of stroke for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2019; 21:231–40.
Article14. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–418.
Article15. Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009; 30:525–31.
Article16. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article17. Kawiorski MM, Martínez-Sánchez P, García-Pastor A, Calleja P, Fuentes B, Sanz-Cuesta BE, et al. Alberta Stroke Program Early CT Score applied to CT angiography source images is a strong predictor of futile recanalization in acute ischemic stroke. Neuroradiology. 2016; 58:487–93.
Article18. Dankbaar JW, Kerckhoffs KG, Horsch AD, van der Schaaf IC, Kappelle LJ, Velthuis BK, et al. Internal carotid artery stenosis and collateral recruitment in stroke patients. Clin Neuroradiol. 2018; 28:339–44.
Article19. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–37.20. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–29.
Article21. Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke. 1999; 30:2280–4.
Article22. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51:1173–82.
Article23. Sen S, Androulakis XM, Duda V, Alonso A, Chen LY, Soliman EZ, et al. Migraine with visual aura is a risk factor for incident atrial fibrillation: a cohort study. Neurology. 2018; 91:e2202–10.24. Mallinckrodt B, Abraham WT, Wei M, Russell DW. Advances in testing the statistical significance of mediation effects. J Couns Psychol. 2006; 53:372–8.25. Demeestere J, Christensen S, Mlynash M, Federau C, Albers GW, Lemmens R, et al. Effect of sex on clinical outcome and imaging after endovascular treatment of large-vessel ischemic stroke. J Stroke Cerebrovasc Dis. 2021; 30:105468.
Article26. Uchida K, Yoshimura S, Sakai N, Yamagami H, Morimoto T. Sex differences in management and outcomes of acute ischemic stroke with large vessel occlusion. Stroke. 2019; 50:1915–8.
Article27. Goda T, Oyama N, Kitano T, Iwamoto T, Yamashita S, Takai H, et al. Factors associated with unsuccessful recanalization in mechanical thrombectomy for acute ischemic stroke. Cerebrovasc Dis Extra. 2019; 9:107–13.
Article28. Hashimoto T, Hayakawa M, Funatsu N, Yamagami H, Satow T, Takahashi JC, et al. Histopathologic analysis of retrieved thrombi associated with successful reperfusion after acute stroke thrombectomy. Stroke. 2016; 47:3035–7.
Article29. Davison MA, Ouyang B, Keppetipola KM, Chen M. Arterial diameter and the gender disparity in stroke thrombectomy outcomes. J Neurointerv Surg. 2018; 10:949–52.30. Müller HR, Brunhölzl C, Radü EW, Buser M. Sex and side differences of cerebral arterial caliber. Neuroradiology. 1991; 33:212–6.
Article31. Hong SJ, Ko YG, Shin DH, Kim JS, Kim BK, Choi D, et al. Impact of vessel diameter measured by preprocedural computed tomography angiography on immediate and late outcomes of endovascular therapy for iliac artery diseases. Circ J. 2017; 81:675–81.32. Kain K, Catto AJ, Carter AM, Young J, Bamford J, Bavington J, et al. Decreased fibrinolytic potential in South Asian women with ischaemic cerebrovascular disease. Br J Haematol. 2001; 114:155–61.
Article33. Kim JS, Lee KB, Roh H, Ahn MY, Hwang HW. Gender differences in the functional recovery after acute stroke. J Clin Neurol. 2010; 6:183–8.
Article34. de Ridder I, Dirks M, Niessen L, Dippel D; PRACTISE Investigators. Unequal access to treatment with intravenous alteplase for women with acute ischemic stroke. Stroke. 2013; 44:2610–2.
Article35. Bushnell C, Howard VJ, Lisabeth L, Caso V, Gall S, Kleindorfer D, et al. Sex differences in the evaluation and treatment of acute ischaemic stroke. Lancet Neurol. 2018; 17:641–50.
Article36. Reeves M, Bhatt A, Jajou P, Brown M, Lisabeth L. Sex differences in the use of intravenous rt-PA thrombolysis treatment for acute ischemic stroke: a meta-analysis. Stroke. 2009; 40:1743–9.37. Yeo LL, Bhogal P, Gopinathan A, Cunli Y, Tan B, Andersson T. Why does mechanical thrombectomy in large vessel occlusion sometimes fail?: a review of the literature. Clin Neuroradiol. 2019; 29:401–14.
Article38. Qureshi AI, Singh B, Huang W, Du Z, Lobanova I, Liaqat J, et al. Mechanical thrombectomy in acute ischemic stroke patients performed within and outside clinical trials in the United States. Neurosurgery. 2020; 86:E2–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of failed mechanical thrombectomy with a focus on technical reasons: Ten years of experience in a single institution
- Clinical and radiological outcomes of mechanical thrombectomy in simultaneous anterior cerebral artery and middle cerebral artery occlusion
- Adjuvant Tirofiban Injection Through Deployed Solitaire Stent As a Rescue Technique After failed Mechanical Thrombectomy in Acute Stroke
- Aspiration-Retriever Technique for Stroke with Large Bore Intermediate Catheter : A Single Center Experience
- Outcomes of Mechanical Thrombectomy in Patients with Large Diffusion-Weighted Imaging Lesions