J Neurocrit Care.
2022 Dec;15(2):96-103. 10.18700/jnc.220061.
Prevalence and prediction of augmented renal clearance in the neurocritical care population
- Affiliations
-
- 1UK HealthCare Pharmacy Services and Department of Pharmacy Practice and Science, University of Kentucky College of Pharmacy, Lexington, KY, USA
- 2Department of Pharmacy Services, University of California, Davis and University of California San Francisco School of Pharmacy, Sacramento, CA, USA
- KMID: 2538766
- DOI: http://doi.org/10.18700/jnc.220061
Abstract
- Background
Augmented renal clearance (ARC; creatinine clearance [CrCl] >130 mL/min/1.73 m2) is prevalent in patients with neurological injuries and may influence their exposure to important pharmacological therapies. Little is known about the relationship between estimated and measured CrCl in this population.
Methods
This single-center, prospective, observational cohort study aimed to describe the association between ARC and estimated CrCl and neurological outcomes in a broad neurocritical care population. Prospective patient screening criteria included adults aged 18–85 years, with critical illness due to neurologic causes (such as ischemic stroke or subarachnoid hemorrhage) and lack of renal dysfunction on admission. Patients who had at least one urine CrCl measurement performed within the first 7 days of hospitalization were included. Two cohorts were evaluated: those with ARC and those without ARC.
Results
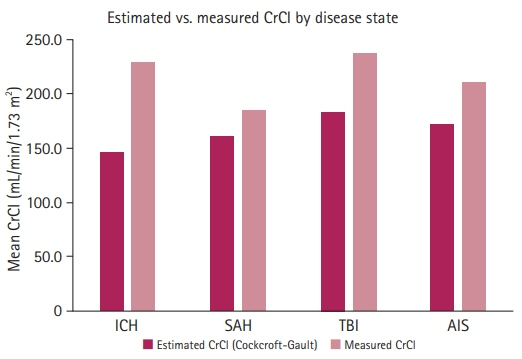
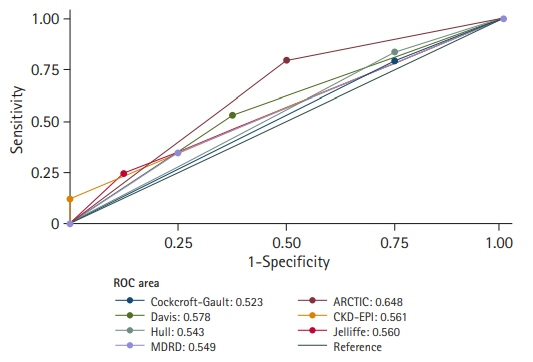
Fifty-seven patients were included, of whom 49 (86%) exhibited ARC. Subjects with ARC were more likely to be male and had a significantly higher median measured CrCl (201.7 mL/min/1.73 m2) than those without ARC (109.8 mL/min/1.73 m2). The Augmented Renal Clearance in Trauma Intensive Care (ARCTIC) score displayed the strongest association (vs. CrCl equations) with ARC development (area under the receiver operating characteristic curve, 0.648).
Conclusion
The prevalence of ARC in the present study of a broad neurocritical care population appeared to be high (86%). The ARCTIC score had higher sensitivity and specificity for diagnosing ARC than the common serum creatinine-based estimation.
Keyword
Figure
Reference
-
1. Cook AM, Arora S, Davis J, Pittman T. Augmented renal clearance of vancomycin and levetiracetam in a traumatic brain injury patient. Neurocrit Care. 2013; 19:210–4.
Article2. May CC, Arora S, Parli SE, Fraser JF, Bastin MT, Cook AM. Augmented renal clearance in patients with subarachnoid hemorrhage. Neurocrit Care. 2015; 23:374–9.
Article3. Udy A, Boots R, Senthuran S, Stuart J, Deans R, Lassig-Smith M, et al. Augmented creatinine clearance in traumatic brain injury. Anesth Analg. 2010; 111:1505–10.
Article4. Udy AA, Jarrett P, Lassig-Smith M, Stuart J, Starr T, Dunlop R, et al. Augmented renal clearance in traumatic brain injury: a single-center observational study of atrial natriuretic peptide, cardiac output, and creatinine clearance. J Neurotrauma. 2017; 34:137–44.
Article5. Morbitzer KA, Jordan JD, Dehne KA, Durr EA, Olm-Shipman CM, Rhoney DH. Enhanced renal clearance in patients with hemorrhagic stroke. Crit Care Med. 2019; 47:800–8.
Article6. Udy AA, Baptista JP, Lim NL, Joynt GM, Jarrett P, Wockner L, et al. Augmented renal clearance in the ICU: results of a multicenter observational study of renal function in critically ill patients with normal plasma creatinine concentrations. Crit Care Med. 2014; 42:520–7.7. Udy AA, Roberts JA, De Waele JJ, Paterson DL, Lipman J. What’s behind the failure of emerging antibiotics in the critically ill?: understanding the impact of altered pharmacokinetics and augmented renal clearance. Int J Antimicrob Agents. 2012; 39:455–7.
Article8. Udy AA, Varghese JM, Altukroni M, Briscoe S, McWhinney BC, Ungerer JP, et al. Subtherapeutic initial β-lactam concentrations in select critically ill patients: association between augmented renal clearance and low trough drug concentrations. Chest. 2012; 142:30–9.
Article9. Grootaert V, Willems L, Debaveye Y, Meyfroidt G, Spriet I. Augmented renal clearance in the critically ill: how to assess kidney function. Ann Pharmacother. 2012; 46:952–9.
Article10. Baptista JP, Neves M, Rodrigues L, Teixeira L, Pinho J, Pimentel J. Accuracy of the estimation of glomerular filtration rate within a population of critically ill patients. J Nephrol. 2014; 27:403–10.
Article11. Barletta JF, Mangram AJ, Byrne M, Sucher JF, Hollingworth AK, Ali-Osman FR, et al. Identifying augmented renal clearance in trauma patients: Validation of the Augmented Renal Clearance in Trauma Intensive Care scoring system. J Trauma Acute Care Surg. 2017; 82:665–71.12. Davis GA, Chandler MH. Comparison of creatinine clearance estimation methods in patients with trauma. Am J Health Syst Pharm. 1996; 53:1028–32.13. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31–41.
Article14. Jelliffe RW. Letter: Creatinine clearance: bedside estimate. Ann Intern Med. 1973; 79:604–5.15. Hull JH, Hak LJ, Koch GG, Wargin WA, Chi SL, Mattocks AM. Influence of range of renal function and liver disease on predictability of creatinine clearance. Clin Pharmacol Ther. 1981; 29:516–21.
Article16. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145:247–54.
Article17. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–12.18. Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017; 80:6–15.
Article19. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012; 43:1711–37.
Article20. Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:2032–60.21. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.22. Clarke JT. Colorimetric determination and distribution of urinary creatinine and creatine. Clin Chem. 1961; 7:371–83.
Article23. Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968; 28:14–20.
Article24. Jennett B, Teasdale G. Aspects of coma after severe head injury. Lancet. 1977; 1:878–81.
Article25. Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001; 32:891–7.26. Goldstein LB, Bertels C, Davis JN. Interrater reliability of the NIH stroke scale. Arch Neurol. 1989; 46:660–2.27. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–74.
Article28. Udy AA, Roberts JA, Lipman J. Implications of augmented renal clearance in critically ill patients. Nat Rev Nephrol. 2011; 7:539–43.
Article29. Baptista JP, Sousa E, Martins PJ, Pimentel JM. Augmented renal clearance in septic patients and implications for vancomycin optimisation. Int J Antimicrob Agents. 2012; 39:420–3.30. Udy AA, Roberts JA, Shorr AF, Boots RJ, Lipman J. Augmented renal clearance in septic and traumatized patients with normal plasma creatinine concentrations: identifying at-risk patients. Crit Care. 2013; 17:R35.
Article31. Udy AA, Jarrett P, Stuart J, Lassig-Smith M, Starr T, Dunlop R, et al. Determining the mechanisms underlying augmented renal drug clearance in the critically ill: use of exogenous marker compounds. Crit Care. 2014; 18:657.
Article32. Garrelts JC, Peterie JD. Altered vancomycin dose vs. serum concentration relationship in burn patients. Clin Pharmacol Ther. 1988; 44:9–13.
Article33. Lott RS, Uden DL, Wargin WA, Strate RG, Zaske DE. Correlation of predicted versus measured creatinine clearance values in burn patients. Am J Hosp Pharm. 1978; 35:717–20.
Article34. Carrie C, Bentejac M, Cottenceau V, Masson F, Petit L, Cochard JF, et al. Association between augmented renal clearance and clinical failure of antibiotic treatment in brain-injured patients with ventilator-acquired pneumonia: a preliminary study. Anaesth Crit Care Pain Med. 2018; 37:35–41.
Article35. Carrié C, Petit L, d'Houdain N, Sauvage N, Cottenceau V, Lafitte M, et al. Association between augmented renal clearance, antibiotic exposure and clinical outcome in critically ill septic patients receiving high doses of β-lactams administered by continuous infusion: a prospective observational study. Int J Antimicrob Agents. 2018; 51:443–9.36. Claus BO, Hoste EA, Colpaert K, Robays H, Decruyenaere J, De Waele JJ. Augmented renal clearance is a common finding with worse clinical outcome in critically ill patients receiving antimicrobial therapy. J Crit Care. 2013; 28:695–700.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Augmented renal clearance
- Neurotrauma Code: Proposal for the Implementation of Strategies in Areas of Difficult Care for a Time-dependent Condition.
- Free Water Clearance: A Clinical marker of Patients with Obstructive Uropathy
- Hiccups in neurocritical care
- Therapeutic Momentum: Scenarios in Patients with Neurotrauma