Clin Endosc.
2023 Jan;56(1):75-82. 10.5946/ce.2022.059.
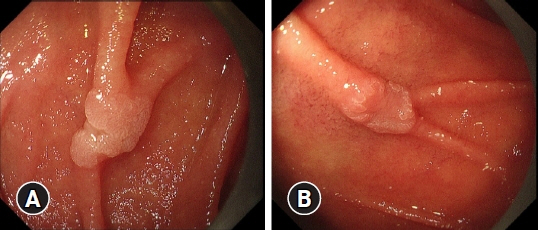
Non-atrophic gastric mucosa is an independently associated factor for superficial non-ampullary duodenal epithelial tumors: a multicenter, matched, case-control study
- Affiliations
-
- 1Department of Gastroenterology, Ishikawa Prefectural Central Hospital, Ishikawa, Japan
- 2Department of Gastrointestinal Oncology, Osaka International Cancer Institute, Osaka, Japan
- 3Department of Gastroenterology and Hepatology, Graduate School of Medical Sciences, Kumamoto University, Kumamoto, Japan
- 4Department of Medicine and Bioregulatory Science, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
- 5Department of Gastroenterology, Fukuoka University Chikushi Hospital, Fukuoka, Japan
- 6Department of Endoscopy, Fukuoka University Chikushi Hospital, Fukuoka, Japan
- 7Department of Gastroenterology, Fukui Prefectural Hospital, Fukui, Japan
- 8Department of Gastroenterology, Kochi Red Cross Hospital, Kochi, Japan
- 9Department of Preventive Medicine and Public Health, Faculty of Medicine, Fukuoka University, Fukuoka, Japan
- KMID: 2538754
- DOI: http://doi.org/10.5946/ce.2022.059
Abstract
- Background/Aims
The etiology of superficial non-ampullary duodenal epithelial tumors (SNADETs) remains unclear. Recent studies have reported conflicting associations between duodenal tumor development and Helicobacter pylori infection or endoscopic gastric mucosal atrophy. As such, the present study aimed to clarify the relationship between SNADETs and H. pylori infection and/or endoscopic gastric mucosal atrophy.
Methods
This retrospective case-control study reviewed data from 177 consecutive patients with SNADETs who underwent endoscopic or surgical resection at seven institutions in Japan over a three-year period. The prevalence of endoscopic gastric mucosal atrophy and the status of H. pylori infection were compared in 531 sex- and age-matched controls selected from screening endoscopies at two of the seven participating institutions.
Results
For H. pylori infection, 85 of 177 (48.0%) patients exhibited SNADETs and 112 of 531 (21.1%) control patients were non-infected (p<0.001). Non-atrophic mucosa (C0 to C1) was observed in 96 of 177 (54.2%) patients with SNADETs and 112 of 531 (21.1%) control patients (p<0.001). Conditional logistic regression analysis revealed that non-atrophic gastric mucosa was an independent risk factor for SNADETs (odds ratio, 5.10; 95% confidence interval, 2.44–8.40; p<0.001).
Conclusions
Non-atrophic gastric mucosa, regardless of H. pylori infection status, was a factor independently associated with SNADETs.
Keyword
Figure
Reference
-
1. Hoffman BP, GrayzeL DM. Benign tumors of the duodenum. Am J Surg. 1945; 70:394–400.2. Darling RC, Welch CE. Tumors of the small intestine. N Engl J Med. 1959; 260:397–408.3. Shukla SK, Elias EG. Primary neoplasms of the duodenum. Surg Gynecol Obstet. 1976; 142:858–860.4. Alwmark A, Andersson A, Lasson A. Primary carcinoma of the duodenum. Ann Surg. 1980; 191:13–18.5. Lim CH, Cho YS. Nonampullary duodenal adenoma: current understanding of its diagnosis, pathogenesis, and clinical management. World J Gastroenterol. 2016; 22:853–861.6. Chow JS, Chen CC, Ahsan H, et al. A population-based study of the incidence of malignant small bowel tumours: SEER, 1973-1990. Int J Epidemiol. 1996; 25:722–728.7. Goda K, Kikuchi D, Yamamoto Y, et al. Endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors in Japan: multicenter case series. Dig Endosc. 2014; 26 Suppl 2:23–29.8. Howe JR, Karnell LH, Menck HR, et al. The American College of Surgeons Commission on Cancer and the American Cancer Society. Adenocarcinoma of the small bowel: review of the National Cancer Data Base, 1985-1995. Cancer. 1999; 86:2693–2706.9. Zar N, Holmberg L, Wilander E, et al. Survival in small intestinal adenocarcinoma. Eur J Cancer. 1996; 32A:2114–2119.10. Dabaja BS, Suki D, Pro B, et al. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004; 101:518–526.11. Kawai T, Takeuchi M, Fukuzawa M. Gastric atrophy prevent from incidence of duodenal tumor? J Clin Biochem Nutr. 2017; 60:219.12. Kakushima N, Ono H, Yoshida M, et al. Characteristics and risk factors for sporadic non-ampullary duodenal adenocarcinoma. Scand J Gastroenterol. 2017; 52:1253–1257.13. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014; 12:1495–1499.14. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.15. Dixon MF. Gastrointestinal epithelial neoplasia: Vienna revisited. Gut. 2002; 51:130–131.16. Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969; 1:87–97.17. Sakaki N, Momma K, Egawa N, et al. The influence of Helicobacter pylori infection on the progression of gastric mucosal atrophy and occurrence of gastric cancer. Eur J Gastroenterol Hepatol. 1995; 7 Suppl 1:S59–S62.18. Kamada T, Haruma K, Inoue K, et al. Helicobacter pylori infection and endoscopic gastritis: Kyoto classification of gastritis. Nihon Shokakibyo Gakkai Zasshi. 2015; 112:982–993.19. Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013; 48:452–458.20. Murray MA, Zimmerman MJ, Ee HC. Sporadic duodenal adenoma is associated with colorectal neoplasia. Gut. 2004; 53:261–265.21. Wu ZJ, Lin Y, Xiao J, et al. Clinical significance of colonoscopy in patients with upper gastrointestinal polyps and neoplasms: a meta-analysis. PLoS One. 2014; 9:e91810.22. Negri E, Bosetti C, La Vecchia C, et al. Risk factors for adenocarcinoma of the small intestine. Int J Cancer. 1999; 82:171–174.23. Ushiku T, Arnason T, Fukayama M, et al. Extra-ampullary duodenal adenocarcinoma. Am J Surg Pathol. 2014; 38:1484–1493.24. Toba T, Inoshita N, Kaise M, et al. Clinicopathological features of superficial non-ampurally duodenal epithelial tumor; gastric phenotype of histology correlates to higher malignant potency. J Gastroenterol. 2018; 53:64–70.25. Minatsuki C, Yamamichi N, Inada KI, et al. Expression of gastric markers is associated with malignant potential of nonampullary duodenal adenocarcinoma. Dig Dis Sci. 2018; 63:2617–2625.26. Harris AW, Gummett PA, Walker MM, et al. Relation between gastric acid output, Helicobacter pylori, and gastric metaplasia in the duodenal bulb. Gut. 1996; 39:513–520.27. Kushima R, Manabe R, Hattori T, et al. Histogenesis of gastric foveolar metaplasia following duodenal ulcer: a definite reparative lineage of Brunner's gland. Histopathology. 1999; 35:38–43.28. Islami F, Kamangar F. Helicobacter pylori and esophageal cancer risk: a meta-analysis. Cancer Prev Res (Phila). 2008; 1:329–338.29. Navarro Silvera SA, Mayne ST, Risch H, et al. Food group intake and risk of subtypes of esophageal and gastric cancer. Int J Cancer. 2008; 123:852–860.30. Chen KH, Mukaisho K, Sugihara H, et al. High animal-fat intake changes the bile-acid composition of bile juice and enhances the development of Barrett's esophagus and esophageal adenocarcinoma in a rat duodenal-contents reflux model. Cancer Sci. 2007; 98:1683–1688.31. Mukaisho K, Nakayama T, Hagiwara T, et al. Two distinct etiologies of gastric cardia adenocarcinoma: interactions among pH, Helicobacter pylori, and bile acids. Front Microbiol. 2015; 6:412.32. Niwa A, Kuwano S, Tomita H, et al. The different pathogeneses of sporadic adenoma and adenocarcinoma in non-ampullary lesions of the proximal and distal duodenum. Oncotarget. 2017; 8:41078–41090.33. Yoshida M, Shimoda T, Abe M, et al. Clinicopathological characteristics of non-ampullary duodenal tumors and their phenotypic classification. Pathol Int. 2019; 69:398–406.34. Maruoka D, Arai M, Ishigami H, et al. Sporadic nonampullary duodenal adenoma/carcinoma is associated with not only colon adenoma/carcinoma but also gastric cancer: association of location of duodenal lesions with comorbid diseases. Scand J Gastroenterol. 2015; 50:333–340.35. Kamada T, Haruma K, Ito M, et al. Time trends in Helicobacter pylori infection and atrophic gastritis over 40 years in Japan. Helicobacter. 2015; 20:192–198.36. Kakushima N, Kanemoto H, Tanaka M, et al. Treatment for superficial non-ampullary duodenal epithelial tumors. World J Gastroenterol. 2014; 20:12501–12508.37. Neugut AI, Jacobson JS, Suh S, et al. The epidemiology of cancer of the small bowel. Cancer Epidemiol Biomarkers Prev. 1998; 7:243–251.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-Ampullary Duodenal Tumors
- Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
- Usefulness of the S-O clip for duodenal endoscopic submucosal dissection: a propensity score-matched study
- Efficacy of Underwater Endoscopic Mucosal Resection for Superficial Non-Ampullary Duodenal Epithelial Tumor
- Underwater Endoscopic Mucosal Resections of Non-ampullary Small Duodenal Tumors