Clin Endosc.
2022 Jan;55(1):15-21. 10.5946/ce.2021.141.
Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
- Affiliations
-
- 1Division of Endoscopy, Shizuoka Cancer Center, Shizuoka, Japan
- 2Department of Gastroenterology and Endoscopy, Sapporo Kinentou hospital, Hokkaido, Japan
- KMID: 2525043
- DOI: http://doi.org/10.5946/ce.2021.141
Abstract
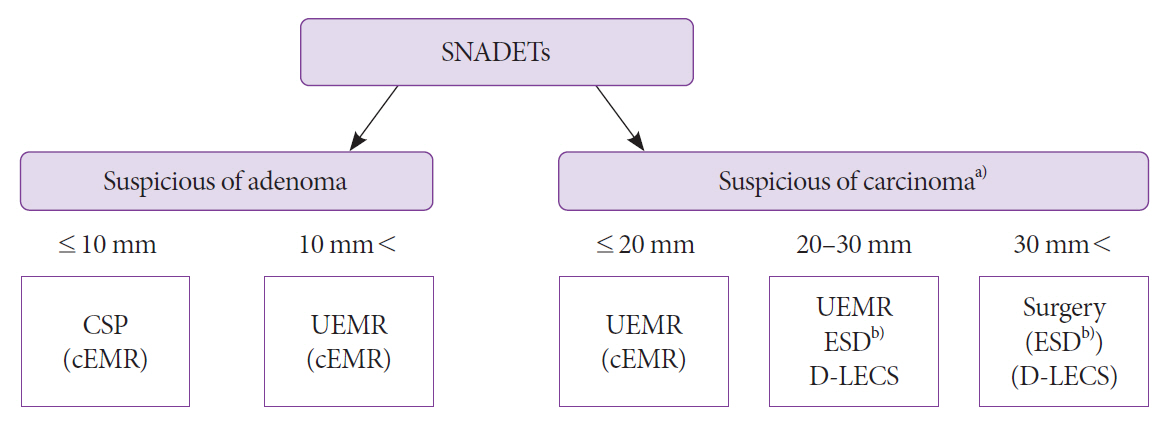
- Endoscopic submucosal dissection (ESD) is the standard treatment method for esophageal, gastric, and colorectal cancers. However, it has not been standardized for duodenal lesions because of its high complication rates. Recently, minimally invasive and simple methods such as cold snare polypectomy and underwater endoscopic mucosal resection have been utilized more for superficial nonampullary duodenal epithelial tumors (SNADETs). Although the rate of complications associated with duodenal ESD has been gradually decreasing because of technical advancements, performing ESD for all SNADETs is unnecessary. As such, the appropriate treatment plan for SNADETs should be chosen according to the lesion type, patient condition, and endoscopist’s skill.
Keyword
Figure
Reference
-
1. Sellner F. Investigations on the significance of the adenoma-carcinoma sequence in the small bowel. Cancer. 1990; 66:702–715.2. Okada K, Fujisaki J, Kasuga A, et al. Sporadic nonampullary duodenal adenoma in the natural history of duodenal cancer: a study of follow-up surveillance. Am J Gastroenterol. 2011; 106:357–364.3. Kinoshita S, Nishizawa T, Ochiai Y, et al. Accuracy of biopsy for the preoperative diagnosis of superficial nonampullary duodenal adenocarcinoma. Gastrointest Endosc. 2017; 86:329–332.4. Kiguchi Y, Kato M, Nakayama A, et al. Feasibility study comparing underwater endoscopic mucosal resection and conventional endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumor < 20 mm. Dig Endosc. 2020; 32:753–760.5. Kakushima N, Yoshida M, Yabuuchi Y, et al. Present status of endoscopic submucosal dissection for non-ampullary duodenal epithelial tumors. Clin Endosc. 2020; 53:652–658.6. Nonaka S, Oda I, Tada K, et al. Clinical outcome of endoscopic resection for nonampullary duodenal tumors. Endoscopy. 2015; 47:129–135.7. Tomizawa Y, Ginsberg GG. Clinical outcome of EMR of sporadic, nonampullary, duodenal adenomas: a 10-year retrospective. Gastrointest Endosc. 2018; 87:1270–1278.8. de Benito Sanz M, Hernández L, Garcia Martinez MI, et al. Efficacy and safety of cold versus hot snare polypectomy for small (5-9mm) colorectal polyps: a multicenter randomized controlled trial. Endoscopy. 2022; 54:35–44.9. Takizawa K, Kakushima N, Tanaka M. Duodenal cold snare polypectomy (D-CSP). Stomach Intest. 2016; 51:1613–1616.10. Maruoka D, Matsumura T, Kasamatsu S, et al. Cold polypectomy for duodenal adenomas: a prospective clinical trial. Endoscopy. 2017; 49:776–783.11. Hamada K, Takeuchi Y, Ishikawa H, et al. Feasibility of cold snare polypectomy for multiple duodenal adenomas in patients with familial adenomatous polyposis: a pilot study. Dig Dis Sci. 2016; 61:2755–2759.12. Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S. “Underwater” EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc. 2012; 75:1086–1091.13. Binmoeller KF, Shah JN, Bhat YM, Kane SD. “Underwater” EMR of sporadic laterally spreading nonampullary duodenal adenomas (with video). Gastrointest Endosc. 2013; 78:496–502.14. Iwagami H, Takeuchi Y, Yamasaki Y, et al. Feasibility of underwater endoscopic mucosal resection and management of residues for superficial non-ampullary duodenal epithelial neoplasms. Dig Endosc. 2020; 32:565–573.15. Yamasaki Y, Uedo N, Takeuchi Y, et al. Underwater endoscopic mucosal resection for superficial nonampullary duodenal adenomas. Endoscopy. 2018; 50:154–158.16. Ono H, Kaise M, Nonaka S, Uedo N, Hirasawa T, Oyama T. Clinical issues of duodenal endoscopic treatment. Stomach Intest. 2016; 51:1585–1592.17. Hoteya S, Furuhata T, Takahito T, et al. Endoscopic submucosal dissection and endoscopic mucosal resection for non-ampullary superficial duodenal tumor. Digestion. 2017; 95:36–42.18. Yahagi N, Kato M, Ochiai Y, et al. Outcomes of endoscopic resection for superficial duodenal epithelial neoplasia. Gastrointest Endosc. 2018; 88:676–682.19. Kato M, Takatori Y, Sasaki M, et al. Water pressure method for duodenal endoscopic submucosal dissection (with video). Gastrointest Endosc. 2021; 93:942–949.20. Kato M, Ochiai Y, Fukuhara S, et al. Clinical impact of closure of the mucosal defect after duodenal endoscopic submucosal dissection. Gastrointest Endosc. 2019; 89:87–93.21. Dohi O, Yoshida N, Naito Y, et al. Efficacy and safety of endoscopic submucosal dissection using a scissors-type knife with prophylactic overthe-scope clip closure for superficial non-ampullary duodenal epithelial tumors. Dig Endosc. 2020; 32:904–913.22. Tashima T, Ohata K, Sakai E, et al. Efficacy of an over-the-scope clip for preventing adverse events after duodenal endoscopic submucosal dissection: a prospective interventional study. Endoscopy. 2018; 50:487–496.23. Yahagi N, Nishizawa T, Akimoto T, Ochiai Y, Goto O. New endoscopic suturing method: string clip suturing method. Gastrointest Endosc. 2016; 84:1064–1065.24. Yamasaki Y, Takeuchi Y, Uedo N, et al. Line-assisted complete closure of duodenal mucosal defects after underwater endoscopic mucosal resection. Endoscopy. 2017; 49:E37–E38.25. Tashima T, Tanisaka Y, Mashimo Y, Mizuide M, Ryozawa S. Endoscopic closure assisted by a novel traction device after duodenal endoscopic submucosal dissection. VideoGIE. 2020; 5:425–427.26. Takimoto K, Imai Y, Matsuyama K. Endoscopic tissue shielding method with polyglycolic acid sheets and fibrin glue to prevent delayed perforation after duodenal endoscopic submucosal dissection. Dig Endosc. 2014; 26(Suppl 2):46–49.27. Hiki N, Yamamoto Y, Fukunaga T, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008; 22:1729–1735.28. Irino T, Nunobe S, Hiki N, et al. Laparoscopic-endoscopic cooperative surgery for duodenal tumors: a unique procedure that helps ensure the safety of endoscopic submucosal dissection. Endoscopy. 2015; 47:349–351.29. Nunobe S, Ri M, Yamazaki K, et al. Safety and feasibility of laparoscopic and endoscopic cooperative surgery for duodenal neoplasm: a retrospective multicenter study. Endoscopy. 2021; 53:1065–1068.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Treatment for Superficial Nonampullary Duodenal Tumors
- SOX9 Is Highly Expressed in Nonampullary Duodenal Adenoma and Adenocarcinoma in Humans
- Clinicopathological features and management strategy for superficial nonampullary duodenal tumors: a multi-center retrospective study
- Non-Ampullary Duodenal Tumors
- Endoscopic Resection for Superficial Non-Ampullary Duodenal Epithelial Tumors