Ann Surg Treat Res.
2022 May;102(5):263-270. 10.4174/astr.2022.102.5.257.
Clinicopathological features and management strategy for superficial nonampullary duodenal tumors: a multi-center retrospective study
- Affiliations
-
- 1Department of Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2529680
- DOI: http://doi.org/10.4174/astr.2022.102.5.257
Abstract
- Purpose
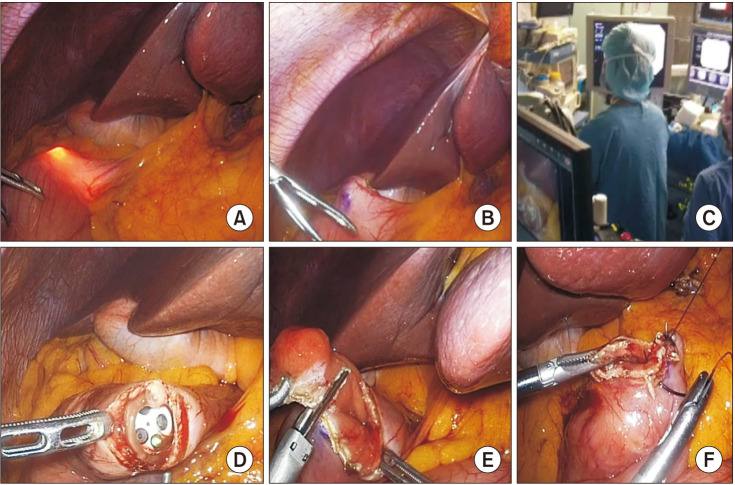
We investigated the clinicopathological features and management for superficial nonampullary duodenal tumors (SNADTs). The safety and feasibility of laparoscopic management, especially laparoscopic endoscopic cooperative surgery (LECS), were evaluated.
Methods
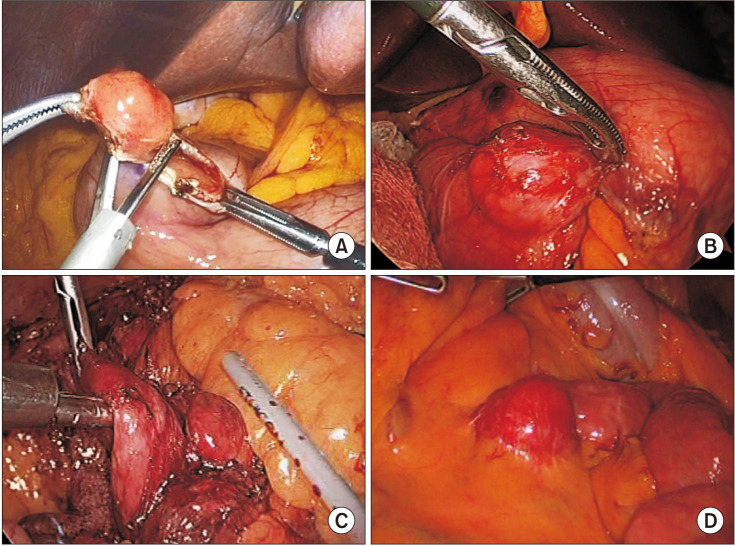
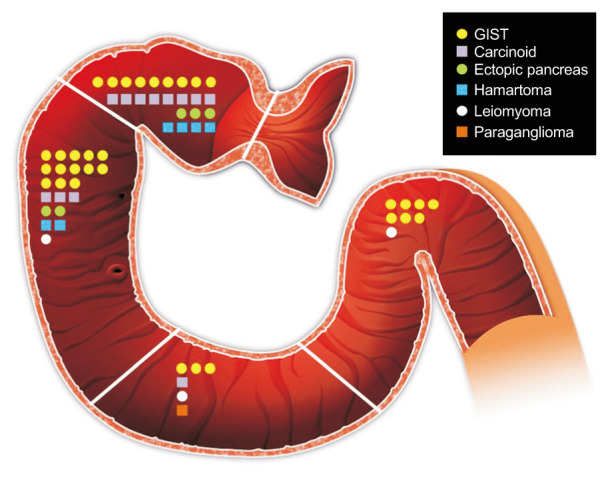
A total of 59 patients with SNADTs who underwent operations from January 2009 to December 2018 at all 8 institutions of the Catholic Medical Center were identified in our comprehensive multi-institutional database. Clinicopathological and surgical data on the 4 anatomical regions of the duodenum were collected and compared.Characteristics of laparoscopic procedure (laparoscopy-only) and LECS procedures were also compared.
Results
There were significantly more asymptomatic patients with tumors in the first and second vs. third and fourth duodenal regions. Gastrointestinal stromal tumors (GISTs), carcinoids, and ectopic pancreatic tumors were identified in 32, 12, and 5 cases, respectively. Forty-two patients (71.2%) underwent laparoscopy. Of patients undergoing laparoscopy, the LECS group exhibited significantly more endophytic features and smaller tumor sizes (P < 0.001 and P < 0.001, respectively). Although no significant difference in the wedge resection or postoperative complication rate was seen between the 2 groups (P = 0.096 and P = 0.227, respectively), the wedge resection rate was higher, and the complication rate lower, in the LECS group than the conventional laparoscopic surgery group.
Conclusion
Most of the SNADTs located in proximal duodenum were detected incidentally. GISTs were the most common diagnoses of SNADTs in all locations. In treating these tumors, laparoscopic resection is safe and feasible. Especially, LECS may be ideal for treating small endophytic tumors, minimizing over-resection and postoperative complications.
Keyword
Figure
Reference
-
1. Shukla SK, Elias EG. Primary neoplasms of the duodenum. Surg Gynecol Obstet. 1976; 142:858–860. PMID: 936029.2. Goda K, Kikuchi D, Yamamoto Y, Takimoto K, Kakushima N, Morita Y, et al. Endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors in Japan: multicenter case series. Dig Endosc. 2014; 26 Suppl 2:23–29.3. Matsumoto S, Miyatani H, Yoshida Y, Nokubi M. Duodenal carcinoid tumors: 5 cases treated by endoscopic submucosal dissection. Gastrointest Endosc. 2011; 74:1152–1156. PMID: 21944312.4. Matsumoto S, Miyatani H, Yoshida Y. Endoscopic submucosal dissection for duodenal tumors: a single-center experience. Endoscopy. 2013; 45:136–137. PMID: 22930172.5. Hoteya S, Furuhata T, Takahito T, Fukuma Y, Suzuki Y, Kikuchi D, et al. Endoscopic submucosal dissection and endoscopic mucosal resection for non-ampullary superficial duodenal tumor. Digestion. 2017; 95:36–42. PMID: 28052275.6. Hoteya S, Yahagi N, Iizuka T, Kikuchi D, Mitani T, Matsui A, et al. Endoscopic submucosal dissection for nonampullary large superficial adenocarcinoma/adenoma of the duodenum: feasibility and long-term outcomes. Endosc Int Open. 2013; 1:2–7. PMID: 26135505.7. Inoue T, Uedo N, Yamashina T, Yamamoto S, Hanaoka N, Takeuchi Y, et al. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc. 2014; 26:220–227. PMID: 23621427.8. Honda T, Yamamoto H, Osawa H, Yoshizawa M, Nakano H, Sunada K, et al. Endoscopic submucosal dissection for superficial duodenal neoplasms. Dig Endosc. 2009; 21:270–274. PMID: 19961529.9. Ichikawa D, Komatsu S, Dohi O, Naito Y, Kosuga T, Kamada K, et al. Laparoscopic and endoscopic co-operative surgery for non-ampullary duodenal tumors. World J Gastroenterol. 2016; 22:10424–10431. PMID: 28058023.10. Kanaji S, Morita Y, Yamazaki Y, Otowa Y, Takao T, Tanaka S, et al. Feasibility of laparoscopic endoscopic cooperative surgery for non-ampullary superficial duodenal neoplasms: single-arm confirmatory trial. Dig Endosc. 2021; 33:373–380. PMID: 32333811.11. Ojima T, Nakamori M, Nakamura M, Hayata K, Katsuda M, Takifuji K, et al. Laparoscopic and endoscopic cooperative surgery versus endoscopic submucosal dissection for the treatment of low-risk tumors of the duodenum. J Gastrointest Surg. 2018; 22:935–940. PMID: 29352442.12. Sakon M, Takata M, Seki H, Hayashi K, Munakata Y, Tateiwa N. A novel combined laparoscopic-endoscopic cooperative approach for duodenal lesions. J Laparoendosc Adv Surg Tech A. 2010; 20:555–558. PMID: 20578925.13. Yanagimoto Y, Omori T, Jeong-Ho M, Shinno N, Yamamoto K, Takeuchi Y, et al. Feasibility and safety of a novel laparoscopic and endoscopic cooperative surgery technique for superficial duodenal tumor resection: how I do it. J Gastrointest Surg. 2019; 23:2068–2074. PMID: 30859426.14. Drake RL, Vogl W, Mitchell AW, Gray H. Gray’s anatomy for students. Philadelphia: Elsevier/Churchill Livingstone;2005.15. Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol. 2008; 39:1411–1419. PMID: 18774375.16. Matsueda K, Kanzaki H, Matsueda K, Nasu J, Yoshioka M, Nakagawa M, et al. The clinicopathological differences of sporadic non-ampullary duodenal epithelial neoplasm depending on tumor location. J Gastroenterol Hepatol. 2019; 34:1540–1544. PMID: 30812050.17. Lee JH, Han HS, Kim YW, Min SK, Lee HK. Laparoscopic wedge resection with handsewn closure for gastroduodenal tumors. J Laparoendosc Adv Surg Tech A. 2003; 13:349–353. PMID: 14733696.18. Adell-Carceller R, Salvador-Sanchís JL, Navarro-Navarro J, Segarra-Soria M, García-Calvo R, Gibert-Gerez J, et al. Laparoscopically treated duodenal hamartoma of Brunner's glands. Surg Laparosc Endosc. 1997; 7:298–300. PMID: 9282760.19. Stauffer JA, Raimondo M, Woodward TA, Goldberg RF, Bowers SP, Asbun HJ. Laparoscopic partial sleeve duodenectomy (PSD) for nonampul lary duodenal neoplasms: avoiding a whipple by separating the duodenum from the pancreatic head. Pancreas. 2013; 42:461–466. PMID: 23462322.20. Yamamoto Y, Yoshizawa N, Tomida H, Fujisaki J, Igarashi M. Therapeutic outcomes of endoscopic resection for superficial non-ampullary duodenal tumor. Dig Endosc. 2014; 26 Suppl 2:50–56. PMID: 24750149.21. Kwon OK, Yu W. Endoscopic and laparoscopic full-thickness resection of endophytic gastric submucosal tumors very close to the esophagogastric junction. J Gastric Cancer. 2015; 15:278–285. PMID: 26819807.22. Min JS, Seo KW, Jeong SH. Choice of LECS procedure for benign and malignant gastric tumors. J Gastric Cancer. 2021; 21:111–121. PMID: 34234973.23. Jeong SH, Bae K, Ha CY, Lee YJ, Lee OJ, Jung WT, et al. Effectiveness of endoscopic clipping and computed tomography gastroscopy for the preoperative localization of gastric cancer. J Korean Surg Soc. 2013; 84:80–87. PMID: 23396626.24. Jeong SH, Seo KW, Min JS. Intraoperative tumor localization of early gastric cancers. J Gastric Cancer. 2021; 21:4–15. PMID: 33854809.25. Wei M, Liang Y, Wang L, Li Z, Chen Y, Yan Z, et al. Clinical application of indocyanine green fluorescence technology in laparoscopic radical gastrectomy. Front Oncol. 2022; 12:847341. PMID: 35311067.26. Lee SJ, Kim GH, Park DY, Choi SA, Lee SH, Choi YY, et al. Acute ectopic pancreatitis occurring after endoscopic biopsy in a gastric ectopic pancreas. Clin Endosc. 2014; 47:455–459. PMID: 25325008.27. Kaneko T, Ohara M, Okamura K, Fujiwara-Kuroda A, Miyasaka D, Yamabuki T, et al. Adenocarcinoma arising from an ectopic pancreas in the duodenum: a case report. Surg Case Rep. 2019; 5:126. PMID: 31388774.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
- Endoscopic Treatment for Superficial Nonampullary Duodenal Tumors
- SOX9 Is Highly Expressed in Nonampullary Duodenal Adenoma and Adenocarcinoma in Humans
- Non-Ampullary Duodenal Tumors
- Efficacy and Long-Term Outcome of Endoscopic Treatment of Sporadic Nonampullary Duodenal Adenoma