Clin Endosc.
2023 Jan;56(1):14-22. 10.5946/ce.2022.247.
Role of artificial intelligence in diagnosing Barrett’s esophagus-related neoplasia
- Affiliations
-
- 1Department of Gastroenterology, University Hospital of Augsburg, Augsburg, Germany
- KMID: 2538747
- DOI: http://doi.org/10.5946/ce.2022.247
Abstract
- Barrett’s esophagus is associated with an increased risk of adenocarcinoma. Thorough screening during endoscopic surveillance is crucial to improve patient prognosis. Detecting and characterizing dysplastic or neoplastic Barrett’s esophagus during routine endoscopy are challenging, even for expert endoscopists. Artificial intelligence-based clinical decision support systems have been developed to provide additional assistance to physicians performing diagnostic and therapeutic gastrointestinal endoscopy. In this article, we review the current role of artificial intelligence in the management of Barrett’s esophagus and elaborate on potential artificial intelligence in the future.
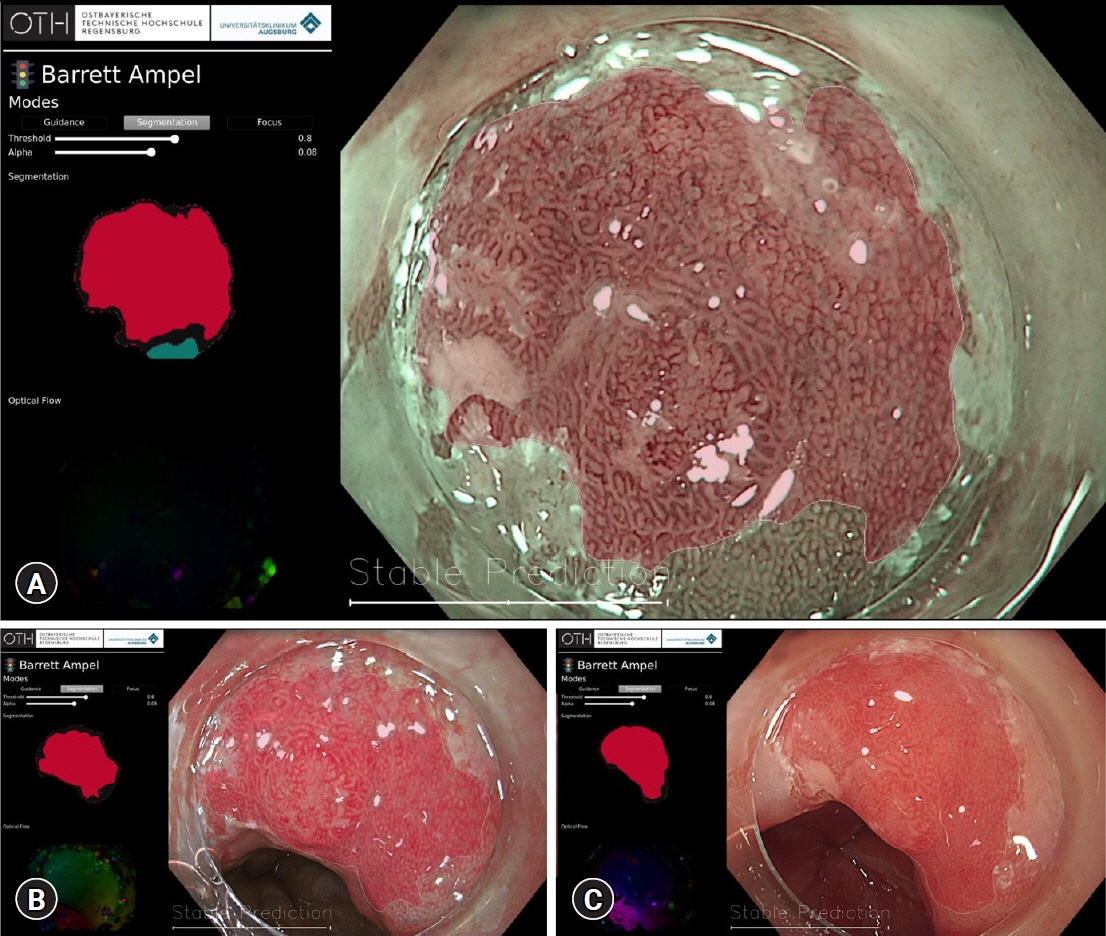
Figure
Cited by 1 articles
-
As how artificial intelligence is revolutionizing endoscopy
Jean-Francois Rey
Clin Endosc. 2024;57(3):302-308. doi: 10.5946/ce.2023.230.
Reference
-
1. Spechler SJ, Souza RF. Barrett’s esophagus. N Engl J Med. 2014; 371:836–845.2. Qumseya BJ, Bukannan A, Gendy S, et al. Systematic review and meta-analysis of prevalence and risk factors for Barrett’s esophagus. Gastrointest Endosc. 2019; 90:707–717.3. Smyth EC, Lagergren J, Fitzgerald RC, et al. Oesophageal cancer. Nat Rev Dis Primers. 2017; 3:17048.4. Coleman HG, Xie SH, Lagergren J. The epidemiology of esophageal adenocarcinoma. Gastroenterology. 2018; 154:390–405.5. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249.6. Kambhampati S, Tieu AH, Luber B, et al. Risk factors for progression of Barrett’s esophagus to high grade dysplasia and esophageal adenocarcinoma. Sci Rep. 2020; 10:4899.7. Chandrasekar VT, Hamade N, Desai M, et al. Significantly lower annual rates of neoplastic progression in short- compared to long-segment non-dysplastic Barrett’s esophagus: a systematic review and meta-analysis. Endoscopy. 2019; 51:665–672.8. Visrodia K, Singh S, Krishnamoorthi R, et al. Magnitude of missed esophageal adenocarcinoma after Barrett’s esophagus diagnosis: a systematic review and meta-analysis. Gastroenterology. 2016; 150:599–607.9. Singer ME, Odze RD. High rate of missed Barrett's esophagus when screening with forceps biopsies. Esophagus. 2023; 20:143–149.10. Sharma P, Bergman JJ, Goda K, et al. Development and validation of a classification system to identify high-grade dysplasia and esophageal adenocarcinoma in Barrett’s esophagus using narrow-band imaging. Gastroenterology. 2016; 150:591–598.11. ASGE Technology Committee, Thosani N, Abu Dayyeh BK, et al. ASGE Technology Committee systematic review and meta-analysis assessing the ASGE Preservation and Incorporation of Valuable Endoscopic Innovations thresholds for adopting real-time imaging-assisted endoscopic targeted biopsy during endoscopic surveillance of Barrett’s esophagus. Gastrointest Endosc. 2016; 83:684–698.12. Qumseya BJ, Wang H, Badie N, et al. Advanced imaging technologies increase detection of dysplasia and neoplasia in patients with Barrett's esophagus: a meta-analysis and systematic review. Clin Gastroenterol Hepatol. 2013; 11:1562–1570.13. Tholoor S, Bhattacharyya R, Tsagkournis O, et al. Acetic acid chromoendoscopy in Barrett’s esophagus surveillance is superior to the standardized random biopsy protocol: results from a large cohort study (with video). Gastrointest Endosc. 2014; 80:417–424.14. Chedgy FJ, Subramaniam S, Kandiah K, et al. Acetic acid chromoendoscopy: improving neoplasia detection in Barrett’s esophagus. World J Gastroenterol. 2016; 22:5753–5760.15. Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019; 25:44–56.16. van der Sommen F, de Groof J, Struyvenberg M, et al. Machine learning in GI endoscopy: practical guidance in how to interpret a novel field. Gut. 2020; 69:2035–2045.17. Hsiao CH, Lin PC, Chung LA, et al. A deep learning-based precision and automatic kidney segmentation system using efficient feature pyramid networks in computed tomography images. Comput Methods Programs Biomed. 2022; 221:106854.18. Zou KH, Warfield SK, Bharatha A, et al. Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol. 2004; 11:178–189.19. van der Sommen F, Zinger S, Curvers WL, et al. Computer-aided detection of early neoplastic lesions in Barrett’s esophagus. Endoscopy. 2016; 48:617–624.20. de Groof AJ, Struyvenberg MR, van der Putten J, et al. Deep-learning system detects neoplasia in patients with Barrett’s esophagus with higher accuracy than endoscopists in a multistep training and validation study with benchmarking. Gastroenterology. 2020; 158:915–929.21. de Groof AJ, Struyvenberg MR, Fockens KN, et al. Deep learning algorithm detection of Barrett’s neoplasia with high accuracy during live endoscopic procedures: a pilot study (with video). Gastrointest Endosc. 2020; 91:1242–1250.22. Hashimoto R, Requa J, Dao T, et al. Artificial intelligence using convolutional neural networks for real-time detection of early esophageal neoplasia in Barrett’s esophagus (with video). Gastrointest Endosc. 2020; 91:1264–1271.23. Iwagami H, Ishihara R, Aoyama K, et al. Artificial intelligence for the detection of esophageal and esophagogastric junctional adenocarcinoma. J Gastroenterol Hepatol. 2021; 36:131–136.24. Ghatwary N, Zolgharni M, Ye X. Early esophageal adenocarcinoma detection using deep learning methods. Int J Comput Assist Radiol Surg. 2019; 14:611–621.25. Struyvenberg MR, de Groof AJ, van der Putten J, et al. A computer-assisted algorithm for narrow-band imaging-based tissue characterization in Barrett’s esophagus. Gastrointest Endosc. 2021; 93:89–98.26. Hussein M, González-Bueno Puyal J, Lines D, et al. A new artificial intelligence system successfully detects and localises early neoplasia in Barrett’s esophagus by using convolutional neural networks. United European Gastroenterol J. 2022; 10:528–537.27. Ebigbo A, Mendel R, Probst A, et al. Computer-aided diagnosis using deep learning in the evaluation of early oesophageal adenocarcinoma. Gut. 2019; 68:1143–1145.28. Ebigbo A, Mendel R, Probst A, et al. Real-time use of artificial intelligence in the evaluation of cancer in Barrett’s oesophagus. Gut. 2020; 69:615–616.29. Ebigbo A, Mendel R, Probst A, et al. Multimodal imaging for detection and segmentation of Barrett’s esophagus-related neoplasia using artificial intelligence. Endoscopy. 2022; 54:E587.30. Ebigbo A, Mendel R, Rückert T, et al. Endoscopic prediction of submucosal invasion in Barrett’s cancer with the use of artificial intelligence: a pilot study. Endoscopy. 2021; 53:878–883.31. Lui TK, Tsui VW, Leung WK. Accuracy of artificial intelligence-assisted detection of upper GI lesions: a systematic review and meta-analysis. Gastrointest Endosc. 2020; 92:821–830.32. Elsbernd BL, Dunbar KB. Volumetric laser endomicroscopy in Barrett’s esophagus. Tech Innov Gastrointest Endosc. 2021; 23:P69–P76.33. Smith MS, Cash B, Konda V, et al. Volumetric laser endomicroscopy and its application to Barrett’s esophagus: results from a 1,000 patient registry. Dis Esophagus. 2019; 32:doz029.34. Trindade AJ, McKinley MJ, Fan C, et al. Endoscopic surveillance of Barrett’s esophagus using volumetric laser endomicroscopy with artificial intelligence image enhancement. Gastroenterology. 2019; 157:303–305.35. Struyvenberg MR, de Groof AJ, Fonollà R, et al. Prospective development and validation of a volumetric laser endomicroscopy computer algorithm for detection of Barrett’s neoplasia. Gastrointest Endosc. 2021; 93:871–879.36. Waterhouse DJ, Januszewicz W, Ali S, et al. Spectral endoscopy enhances contrast for neoplasia in surveillance of Barrett’s esophagus. Cancer Res. 2021; 81:3415–3425.37. Sharma P, Savides TJ, Canto MI, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on imaging in Barrett’s Esophagus. Gastrointest Endosc. 2012; 76:252–254.38. Pan W, Li X, Wang W, et al. Identification of Barrett’s esophagus in endoscopic images using deep learning. BMC Gastroenterol. 2021; 21:479.39. Ali S, Bailey A, Ash S, et al. A pilot study on automatic three-dimensional quantification of Barrett’s esophagus for risk stratification and therapy monitoring. Gastroenterology. 2021; 161:865–878.40. Beg S, Ragunath K, Wyman A, et al. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017; 66:1886–1899.41. Bisschops R, Areia M, Coron E, et al. Performance measures for upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2016; 48:843–864.42. Wu L, Zhang J, Zhou W, et al. Randomised controlled trial of WISENSE, a real-time quality improving system for monitoring blind spots during esophagogastroduodenoscopy. Gut. 2019; 68:2161–2169.