Cardiovasc Prev Pharmacother.
2019 Oct;1(2):57-62. 10.36011/cpp.2019.1.e6.
Improving Causal Inference in Observational Studies: Propensity Score Matching
- Affiliations
-
- 1Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Department of Precision Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2536964
- DOI: http://doi.org/10.36011/cpp.2019.1.e6
Abstract
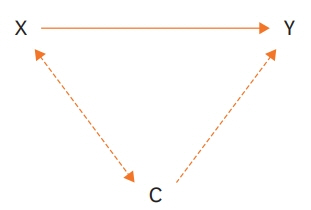
- Propensity score matching (PSM) is a useful statistical methods to improve causal inference in observational studies. It guarantees comparability between 2 comparison groups are required. PSM is based on a “counterfactual” framework, where a causal effect on study participants (factual) and assumed participants (counterfactual) are compared. All participants are divided into 2 groups with the same covariates matched as much as possible. Propensity score is used for matching, and it reflects the conditional probabilities that individuals will be included in the experimental group when covariates are controlled for all subjects. The counterfactuals for the experimental group are matched between groups with characteristics as similar as possible. In this article, we introduce the concept of PSM, PSM methods, limitations, and statistical tools.
Figure
Reference
-
1. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011; 46:399–424.
Article2. Gum PA, Thamilarasan M, Watanabe J, Blackstone EH, Lauer MS. Aspirin use and all-cause mortality among patients being evaluated for known or suspected coronary artery disease: a propensity analysis. JAMA. 2001; 286:1187–94.
Article3. Seung KB, Park DW, Kim YH, Lee SW, Lee CW, Hong MK, Park SW, Yun SC, Gwon HC, Jeong MH, Jang Y, Kim HS, Kim PJ, Seong IW, Park HS, Ahn T, Chae IH, Tahk SJ, Chung WS, Park SJ. Stents versus coronaryartery bypass grafting for left main coronary artery disease. N Engl J Med. 2008; 358:1781–92.
Article4. Yao X, Gersh BJ, Holmes DR Jr, Melduni RM, Johnsrud DO, Sangaralingham LR, Shah ND, Noseworthy PA. Association of surgical left atrial appendage occlusion with subsequent stroke and mortality among patients undergoing cardiac surgery. JAMA. 2018; 319:2116–26.
Article5. Rubin DB. Bayesian inference for causal effects: the role of randomization. Ann Stat. 1978; 6:34–58.
Article6. Rubin DB. Estimating causal effects of treatments in randomized and nonrandomized studies. J Educ Psychol. 1974; 66:688–701.
Article7. Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2008; 22:31–72.
Article8. D'Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a nonrandomized control group. Stat Med. 1998; 17:2265–81.9. Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983; 70:41–55.
Article10. Stuart EA, Rubin DB. Best practices in quasi-experimental designs: matching methods for causal inference. In : Osborne J, editor. Best Practices in Quantitative Methods. Thousand Oaks, CA: Sage Publications;2008. p. 155–76.11. Dehejia RH, Wahba S. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002; 84:151–61.
Article12. Iacus SM, King G, Porro G. Causal inference without balance checking: Coarsened exact matching. Polit Anal. 2012; 20:1–24.
Article13. Hansen BB, Bowers J. Covariate balance in simple, stratified and clustered comparative studies. Stat Sci. 2008; 23:219–36.
Article14. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009; 28:3083–107.
Article15. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000; 11:550–60.
Article16. In : Coca-Perraillon M, editor. Local and global optimal propensity score matching. SAS Global Forum 2007; 2007 Apr 16-19; Orlando, FL. Cary. SAS Institute. 2007 Apr. 9 p.17. Ho DE, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011; 42:1–28.18. Leuven E, Sianesi B. PSMATCH2: stata module to perform full Mahalanobis and propensity score matching, common support graphing, and covariate imbalance testing. [place unknown]: RePEc; [cited 2018 February]. Available from http://EconPapers.repec.org/RePEc:boc:bocode:s432001.19. Thoemmes F. Propensity score matching in SPSS [Internet]. Ithaca, NY: arXiv, Cornell University Library; [cited 2012 January]. Available from https://arxiv.org/abs/1201.6385.20. King G, Nielsen R. Why propensity scores should not be used for matching. Polit Anal 2016:1-20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An introduction to propensity score matching methods
- Applications of propensity score matching: a case series of articles published in Annals of Coloproctology
- Propensity Score Matching: A Conceptual Review for Radiology Researchers
- Propensity score matching for comparative studies: a tutorial with R and Rex
- Application of Standardization for Causal Inference in Observational Studies: A Step-by-step Tutorial for Analysis Using R Software