Korean Circ J.
2022 Dec;52(12):890-900. 10.4070/kcj.2022.0154.
Statins and Clinical Outcomes in Patients With Low to Moderate Risk but With Non-obstructive Carotid Plaques: The SCOPE-CP Study
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2536792
- DOI: http://doi.org/10.4070/kcj.2022.0154
Abstract
- Background and Objectives
Some individuals exhibit discrepancies between risk classifications assessed using clinical factors and those obtained by vascular imaging. We aimed to evaluate whether statins provide clinical outcome benefits in patients classified as having low to moderate cardiovascular risk but with carotid plaque.
Methods
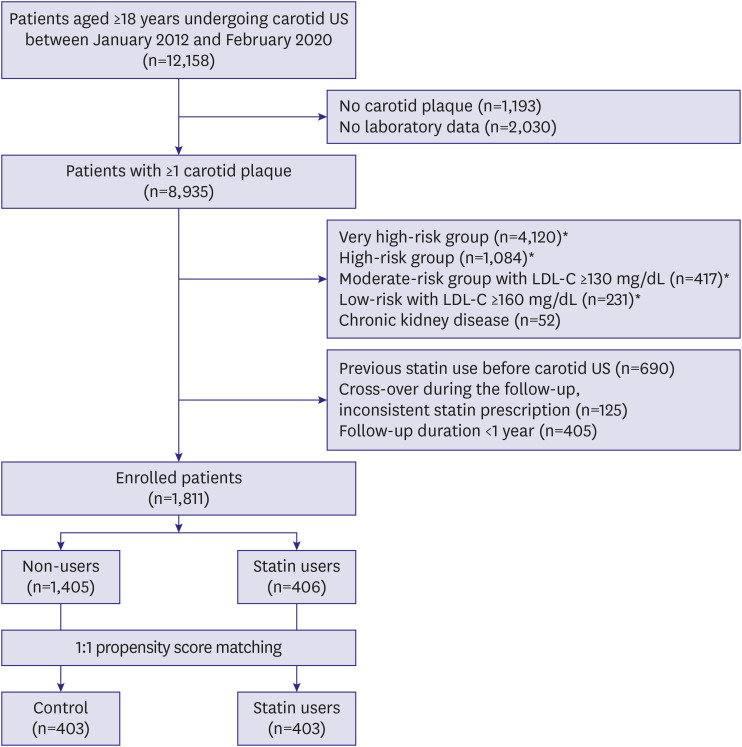
This was a retrospective propensity score matching study. A total of 12,158 consecutive patients undergoing carotid ultrasound between January 2012 to February 2020 were screened. Individuals with low to moderate cardiovascular risk who were not currently recommended for statin therapy but had carotid plaques were included. Among 1,611 enrolled individuals, 806 (statin group: 403, control group: 403) were analyzed. The primary outcomes were major adverse cardiovascular and cerebrovascular events (MACCEs: cardiovascular death, myocardial infarction, coronary revascularization, and ischemic stroke or transient ischemic attack) and all-cause mortality.
Results
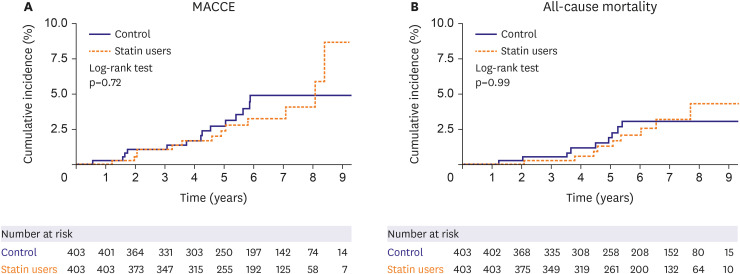
During the median follow-up of 6.0 years, the incidence of MACCEs did not differ between the groups (6.1 and 5.7/1,000 person-years in the control and statin groups, respectively; adjusted hazard ratio [HR], 0.95; p=0.90). The incidence of all-cause mortality did not differ (3.9 and 3.9/1,000 person-years, respectively; adjusted HR, 1.02; p=0.97). Kaplan-Meier curves revealed similar rates of MACCEs (log-rank p=0.72) and all-cause mortality (log-rank p=0.99) in the 2 groups. Age and smoking were independent predictors of MACCEs. Subgroups exhibited no differences in clinical outcomes with statin use.
Conclusions
Benefit of statin therapy was likely to be limited in low to moderate risk patients with carotid plaques. These results could guide physicians in clinical decision-making regarding cardiovascular prevention.
Figure
Reference
-
1. Cho SM, Lee H, Lee HH, et al. Dyslipidemia fact sheets in Korea 2020: an analysis of nationwide population-based data. J Lipid Atheroscler. 2021; 10:202–209. PMID: 34095012.2. Lee YB, Kim B, Han K, et al. Combination of statin and ezetimibe versus statin monotherapy on cardiovascular disease and type 2 diabetes incidence among adults with impaired fasting glucose: a propensity-matched nationwide cohort study. J Lipid Atheroscler. 2021; 10:303–312. PMID: 34621701.3. Rhee EJ, Kim HC, Kim JH, et al. 2018 Guidelines for the management of dyslipidemia in Korea. J Lipid Atheroscler. 2019; 8:78–131. PMID: 32821702.4. Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020; 41:111–188. PMID: 31504418.5. Nezu T, Hosomi N. Usefulness of carotid ultrasonography for risk stratification of cerebral and cardiovascular disease. J Atheroscler Thromb. 2020; 27:1023–1035. PMID: 32863299.6. Spence JD. Measurement of carotid plaque burden. Curr Opin Lipidol. 2020; 31:291–298. PMID: 32773468.7. Baber U, Mehran R, Sartori S, et al. Prevalence, impact, and predictive value of detecting subclinical coronary and carotid atherosclerosis in asymptomatic adults: the BioImage study. J Am Coll Cardiol. 2015; 65:1065–1074. PMID: 25790876.8. Mehta A, Rigdon J, Tattersall MC, et al. Association of carotid artery plaque with cardiovascular events and incident coronary artery calcium in individuals with absent coronary calcification: the MESA. Circ Cardiovasc Imaging. 2021; 14:e011701. PMID: 33827231.9. Spence JD, Coates V, Li H, et al. Effects of intensive medical therapy on microemboli and cardiovascular risk in asymptomatic carotid stenosis. Arch Neurol. 2010; 67:180–186. PMID: 20008646.10. Adams A, Bojara W, Romanens M. Effect of statin treatment in patients with advanced carotid atherosclerosis: an observational outcome study. Cardiol Rev. 2021; 12:335–339.11. Kim K, Lee CJ, Shim CY, et al. Statin and clinical outcomes of primary prevention in individuals aged >75 years: the SCOPE-75 study. Atherosclerosis. 2019; 284:31–36. PMID: 30870705.12. Talic S, Marquina C, Ofori-Asenso R, et al. Switching, persistence and adherence to statin therapy: a retrospective cohort study using the Australian National Pharmacy Data. Cardiovasc Drugs Ther. 2022; 36:867–877. PMID: 34097194.13. Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. 2012; 34:290–296. PMID: 23128470.14. Sillesen H, Sartori S, Sandholt B, Baber U, Mehran R, Fuster V. Carotid plaque thickness and carotid plaque burden predict future cardiovascular events in asymptomatic adult Americans. Eur Heart J Cardiovasc Imaging. 2018; 19:1042–1050. PMID: 29059296.15. Parish S, Arnold M, Clarke R, et al. Assessment of the role of carotid atherosclerosis in the association between major cardiovascular risk factors and ischemic stroke subtypes. JAMA Netw Open. 2019; 2:e194873. PMID: 31150080.16. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019; 73:e285–e350. PMID: 30423393.17. Baek J, Lee H, Lee HH, Heo JE, Cho SM, Kim HC. Thirty-six year trends in mortality from diseases of circulatory system in Korea. Korean Circ J. 2021; 51:320–332. PMID: 33821581.18. Lee E, Choi EK, Han KD, et al. Mortality and causes of death in patients with atrial fibrillation: a nationwide population-based study. PLoS One. 2018; 13:e0209687. PMID: 30586468.19. Mortensen MB, Fuster V, Muntendam P, et al. Negative risk markers for cardiovascular events in the elderly. J Am Coll Cardiol. 2019; 74:1–11. PMID: 31272534.20. Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid–sparing effect of benralizumab in severe asthma. N Engl J Med. 2017; 376:2448–2458. PMID: 28530840.21. Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010; 56:e50–103. PMID: 21144964.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Benefit of Statins in Korean Patients with Acute Myocardial Infarction: Experience of the Korea Acute Myocardial Infarction Registry
- Carotid Ultrasound: Carotid Plaques and Clinical Significance
- Carotid ultrasound in patients with coronary artery disease
- Role of Blood Lipid Levels and Lipid-Lowering Therapy in Stroke Patients with Different Levels of Cerebral Artery Diseases: Reconsidering Recent Stroke Guidelines
- Evaluation of Carotid Plaque Using Ultrasound Imaging