J Stroke.
2021 May;23(2):149-161. 10.5853/jos.2021.01249.
Role of Blood Lipid Levels and Lipid-Lowering Therapy in Stroke Patients with Different Levels of Cerebral Artery Diseases: Reconsidering Recent Stroke Guidelines
- Affiliations
-
- 1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2516406
- DOI: http://doi.org/10.5853/jos.2021.01249
Abstract
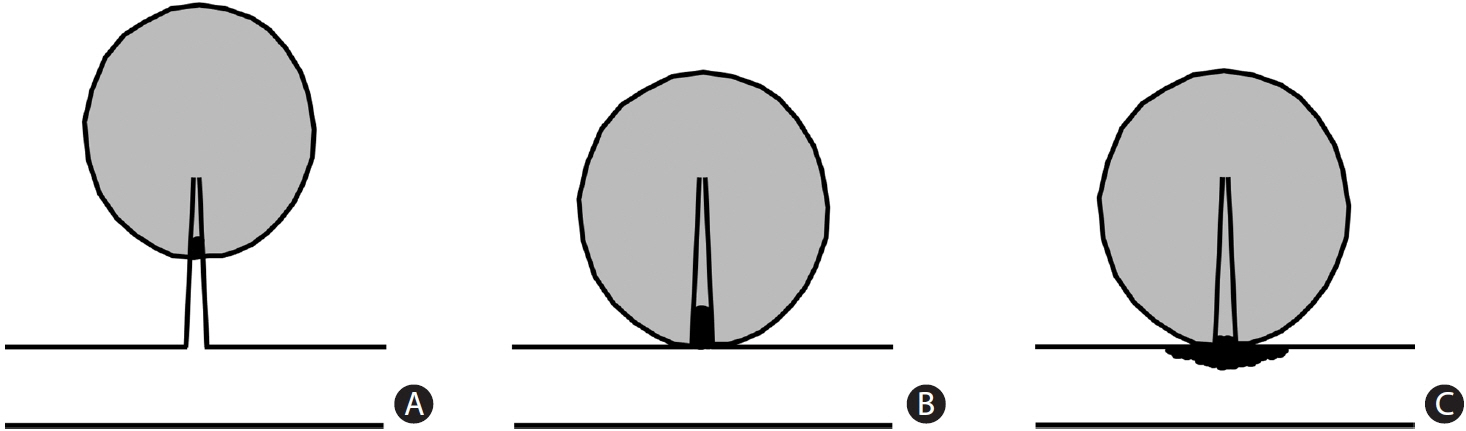
- Hyperlipidemia is an important risk factor for ischemic stroke; the Stroke Prevention by Aggressive Reduction in Cholesterol Level and Treat Stroke to Target studies have shown that statins are beneficial for patients with stroke and that a low target for low-density lipoprotein cholesterol (LDL-C) concentration may maximize this benefit. Based on these results, recent guidelines have emphasized the application of “high-intensity statins” and “low LDL-C target” strategies in patients with stroke. However, it should be kept in mind that the role of blood lipids as a risk factor and benefit of lipid-lowering therapy are different among patients with different levels of cerebral arterial diseases. Studies have suggested that hypolipidemia, but not hyperlipidemia, is a risk factor for small vessel diseases (SVDs) such as intracerebral hemorrhages, microbleeds, white matter hyperintensities, and perhaps, lacunar infarction. Although lipid-lowering agents might benefit certain patients with SVD, high-intensity statin and low LDL-C target strategies cannot be applied. In contrast, these strategies are important in patients with extracranial atherosclerosis, such as internal carotid disease, considering ample evidence of the benefits of lipid-lowering agents. Imaging studies have shown that statins stabilize vulnerable plaques in these patients. Although lipid-lowering agents are likely to benefit patients with intracranial atherosclerosis, the degree of their benefit and appropriate target LDL-C level for these patients remain unclear. More studies are needed to elucidate the appropriate lipid-modifying strategies in patients with stroke with different levels of cerebral artery disease.
Figure
Cited by 2 articles
-
Leukoaraiosis: Epidemiology, Imaging, Risk Factors, and Management of Age-Related Cerebral White Matter Hyperintensities
Wen-Qing Huang, Qing Lin, Chi-Meng Tzeng
J Stroke. 2024;26(2):131-163. doi: 10.5853/jos.2023.02719.Deep Learning-Based Automatic Classification of Ischemic Stroke Subtype Using Diffusion-Weighted Images
Wi-Sun Ryu, Dawid Schellingerhout, Hoyoun Lee, Keon-Joo Lee, Chi Kyung Kim, Beom Joon Kim, Jong-Won Chung, Jae-Sung Lim, Joon-Tae Kim, Dae-Hyun Kim, Jae-Kwan Cha, Leonard Sunwoo, Dongmin Kim, Sang-Il Suh, Oh Young Bang, Hee-Joon Bae, Dong-Eog Kim
J Stroke. 2024;26(2):300-311. doi: 10.5853/jos.2024.00535.
Reference
-
References
1. Shahar E, Chambless LE, Rosamond WD, Boland LL, Ballantyne CM, McGovern PG, et al. Plasma lipid profile and incident ischemic stroke: the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2003; 34:623–631.2. Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010; 376:1670–1681.3. Collins R, Armitage J, Parish S, Sleight P, Peto R; Heart Protection Study Collaborative Group. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet. 2004; 363:757–767.4. Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006; 355:549–559.
Article5. Amarenco P, Goldstein LB, Szarek M, Sillesen H, Rudolph AE, Callahan A 3rd, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2007; 38:3198–3204.6. Amarenco P, Kim JS, Labreuche J, Charles H, Abtan J, Béjot Y, et al. A comparison of two LDL cholesterol targets after ischemic stroke. N Engl J Med. 2020; 382:9.
Article7. Amarenco P, Kim JS, Labreuche J, Charles H, Giroud M, Lee BC, et al. Benefit of targeting a LDL (low-density lipoprotein) cholesterol <70 mg/dL during 5 years after ischemic stroke. Stroke. 2020; 51:1231–1239.8. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article9. Sagris D, Ntaios G, Georgiopoulos G, Kakaletsis N, Elisaf M, Katsiki N, et al. Recommendations for lipid modification in patients with ischemic stroke or transient ischemic attack: a clinical guide by the Hellenic Stroke Organization and the Hellenic Atherosclerosis Society. Int J Stroke. 2020. Nov. 17. [Epub]. https://doi.org/10.1177/1747493020971970.
Article10. Ahmed N, Audebert H, Turc G, Cordonnier C, Christensen H, Sacco S, et al. Consensus statements and recommendations from the ESO-Karolinska Stroke Update Conference, Stockholm 11-13 November 2018. Eur Stroke J. 2019; 4:307–317.
Article11. Sillesen H, Amarenco P, Hennerici MG, Callahan A, Goldstein LB, Zivin J, et al. Atorvastatin reduces the risk of cardiovascular events in patients with carotid atherosclerosis: a secondary analysis of the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke. 2008; 39:3297–3302.12. Iso H, Jacobs DR Jr, Wentworth D, Neaton JD, Cohen JD. Serum cholesterol levels and six-year mortality from stroke in 350,977 men screened for the multiple risk factor intervention trial. N Engl J Med. 1989; 320:904–910.
Article13. Ebrahim S, Sung J, Song YM, Ferrer RL, Lawlor DA, Davey Smith G. Serum cholesterol, haemorrhagic stroke, ischaemic stroke, and myocardial infarction: Korean National Health System prospective cohort study. BMJ. 2006; 333:22.
Article14. Choi-Kwon S, Kim JS. Lifestyle factors and risk of stroke in Seoul, South Korea. J Stroke Cerebrovasc Dis. 1998; 7:414–420.
Article15. Ma C, Na M, Neumann S, Gao X. Low-density lipoprotein cholesterol and risk of hemorrhagic stroke: a systematic review and dose-response meta-analysis of prospective studies. Curr Atheroscler Rep. 2019; 21:52.
Article16. Lee SH, Bae HJ, Yoon BW, Kim H, Kim DE, Roh JK. Low concentration of serum total cholesterol is associated with multifocal signal loss lesions on gradient-echo magnetic resonance imaging: analysis of risk factors for multifocal signal loss lesions. Stroke. 2002; 33:2845–2849.17. Konishi M, Iso H, Komachi Y, Iida M, Shimamoto T, Jacobs DR Jr, et al. Associations of serum total cholesterol, different types of stroke, and stenosis distribution of cerebral arteries. The Akita Pathology Study. Stroke. 1993; 24:954–964.
Article18. Hackam DG, Woodward M, Newby LK, Bhatt DL, Shao M, Smith EE, et al. Statins and intracerebral hemorrhage: collaborative systematic review and meta-analysis. Circulation. 2011; 124:2233–2242.19. McKinney JS, Kostis WJ. Statin therapy and the risk of intracerebral hemorrhage: a meta-analysis of 31 randomized controlled trials. Stroke. 2012; 43:2149–2156.
Article20. Åsberg S, Eriksson M. Statin therapy and the risk of intracerebral haemorrhage: a nationwide observational study. Int J Stroke. 2015; 10 Suppl A100:46–49.
Article21. Devaraj S, Rogers J, Jialal I. Statins and biomarkers of inflammation. Curr Atheroscler Rep. 2007; 9:33–41.
Article22. Jung JM, Choi JY, Kim HJ, Seo WK. Statin use in spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. Int J Stroke. 2015; 10 Suppl A100:10–17.
Article23. Katsanos AH, Lioutas VA, Charidimou A, Catanese L, Ng KKH, Perera K, et al. Statin treatment and cerebral microbleeds: a systematic review and meta-analysis. J Neurol Sci. 2021; 420:117224.
Article24. Chen PS, Cheng CL, Chang YC, Kao Yang YH, Yeh PS, Li YH. Early statin therapy in patients with acute intracerebral hemorrhage without prior statin use. Eur J Neurol. 2015; 22:773–780.
Article25. Pan YS, Jing J, Wang YL, Zhao XQ, Song B, Wang WJ, et al. Use of statin during hospitalization improves the outcome after intracerebral hemorrhage. CNS Neurosci Ther. 2014; 20:548–555.
Article26. Miura K, Yoshii Y, Nakamura Y, Ikeda K. Clinicoradiological profile and serum lipid levels of intracerebral hemorrhage in prior statin users. Intern Med. 2011; 50:1385–1391.
Article27. Mustanoja S, Strbian D, Putaala J, Meretoja A, Curtze S, Haapaniemi E, et al. Association of prestroke statin use and lipid levels with outcome of intracerebral hemorrhage. Stroke. 2013; 44:2330–2332.
Article28. Marseglia LM, Nicotera A, Salpietro V, Giaimo E, Cardile G, Bonsignore M, et al. Hyperhomocysteinemia and MTHFR polymorphisms as antenatal risk factors of white matter abnormalities in two cohorts of late preterm and full term newborns. Oxid Med Cell Longev. 2015; 2015:543134.
Article29. Dufouil C, de Kersaint-Gilly A, Besançon V, Levy C, Auffray E, Brunnereau L, et al. Longitudinal study of blood pressure and white matter hyperintensities: the EVA MRI Cohort. Neurology. 2001; 56:921–926.30. Mok V, Kim JS. Prevention and management of cerebral small vessel disease. J Stroke. 2015; 17:111–122.
Article31. Zhuang FJ, Chen Y, He WB, Cai ZY. Prevalence of white matter hyperintensities increases with age. Neural Regen Res. 2018; 13:2141–2146.
Article32. Jimenez-Conde J, Biffi A, Rahman R, Kanakis A, Butler C, Sonni S, et al. Hyperlipidemia and reduced white matter hyperintensity volume in patients with ischemic stroke. Stroke. 2010; 41:437–442.
Article33. Schmidt R, Hayn M, Fazekas F, Kapeller P, Esterbauer H. Magnetic resonance imaging white matter hyperintensities in clinically normal elderly individuals. Correlations with plasma concentrations of naturally occurring antioxidants. Stroke. 1996; 27:2043–2047.34. Longstreth WT Jr, Arnold AM, Beauchamp NJ Jr, Manolio TA, Lefkowitz D, Jungreis C, et al. Incidence, manifestations, and predictors of worsening white matter on serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke. 2005; 36:56–61.35. ten Dam VH, van den Heuvel DM, van Buchem MA, Westendorp RG, Bollen EL, Ford I, et al. Effect of pravastatin on cerebral infarcts and white matter lesions. Neurology. 2005; 64:1807–1809.
Article36. Vuorinen M, Solomon A, Rovio S, Nieminen L, Kåreholt I, Tuomilehto J, et al. Changes in vascular risk factors from midlife to late life and white matter lesions: a 20-year follow-up study. Dement Geriatr Cogn Disord. 2011; 31:119–125.
Article37. Caplan LR. Intracranial branch atheromatous disease: a neglected, understudied, and underused concept. Neurology. 1989; 39:1246–1250.
Article38. Kim JS, Yoon Y. Single subcortical infarction associated with parental arterial disease: important yet neglected sub-type of atherothrombotic stroke. Int J Stroke. 2013; 8:197–203.
Article39. Nah HW, Kang DW, Kwon SU, Kim JS. Diversity of single small subcortical infarctions according to infarct location and parent artery disease: analysis of indicators for small vessel disease and atherosclerosis. Stroke. 2010; 41:2822–2827.40. Tang H, Wang Y, Cheng A, Wang A, Xu J, Zhang C, et al. Association between low-density lipoprotein cholesterol levels and proximal single subcortical infarction in comparison with distal single subcortical infarction. J Stroke Cerebrovasc Dis. 2020; 29:105198.
Article41. Yoon Y, Lee DH, Kang DW, Kwon SU, Suh DC, Bang OY, et al. Stroke recurrence patterns are predicted by the subtypes and mechanisms of the past, non-cardiogenic stroke. Eur J Neurol. 2013; 20:928–934.
Article42. Lv P, Jin H, Liu Y, Cui W, Peng Q, Liu R, et al. Comparison of risk factor between lacunar stroke and large artery atherosclerosis stroke: a cross-sectional study in China. PLoS One. 2016; 11:e0149605.
Article43. Arboix A, Font A, Garro C, García-Eroles L, Comes E, Massons J. Recurrent lacunar infarction following a previous lacunar stroke: a clinical study of 122 patients. J Neurol Neurosurg Psychiatry. 2007; 78:1392–1394.
Article44. Hosomi N, Nagai Y, Kohriyama T, Ohtsuki T, Aoki S, Nezu T, et al. The Japan Statin Treatment Against Recurrent Stroke (J-STARS): a multicenter, randomized, open-label, parallel-group study. EBioMedicine. 2015; 2:1071–1078.
Article45. Martínez-Sánchez P, Rivera-Ordóñez C, Fuentes B, Ortega-Casarrubios MA, Idrovo L, Díez-Tejedor E. The beneficial effect of statins treatment by stroke subtype. Eur J Neurol. 2009; 16:127–133.
Article46. Heyden S, Heyman A, Goree JA. Nonembolic occlusion of the middle cerebral and carotid arteries: a comparison of predisposing factors. Stroke. 1970; 1:363–369.47. Caplan LR, Gorelick PB, Hier DB. Race, sex and occlusive cerebrovascular disease: a review. Stroke. 1986; 17:648–655.
Article48. Kuller L, Reisler DM. An explanation for variations in distribution of stroke and arteriosclerotic heart disease among populations and racial groups. Am J Epidemiol. 1971; 93:1–9.49. Uehara T, Tabuchi M, Mori E. Frequency and clinical correlates of occlusive lesions of cerebral arteries in Japanese patients without stroke. Evaluation by MR angiography. Cerebrovasc Dis. 1998; 8:267–272.50. Kim JS, Nah HW, Park SM, Kim SK, Cho KH, Lee J, et al. Risk factors and stroke mechanisms in atherosclerotic stroke: intracranial compared with extracranial and anterior compared with posterior circulation disease. Stroke. 2012; 43:3313–3318.51. Lei C, Wu B, Liu M, Chen Y. Risk factors and clinical outcomes associated with intracranial and extracranial atherosclerotic stenosis acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23:1112–1117.
Article52. Weber G. Delayed experimental atherosclerotic involvement of cerebral arteries in monkeys and rabbits (light, sem and tem observations). Pathol Res Pract. 1985; 180:353–355.
Article53. Kurozumi T, Imamura T, Tanaka K, Yae Y, Koga S. Permeation and deposition of fibrinogen and low-density lipoprotein in the aorta and cerebral artery of rabbits: immuno-electron microscopic study. Br J Exp Pathol. 1984; 65:355–364.54. Yang WJ, Fisher M, Zheng L, Niu CB, Paganini-Hill A, Zhao HL, et al. Histological characteristics of intracranial atherosclerosis in a Chinese population: a postmortem study. Front Neurol. 2017; 8:488.
Article55. Chung JW, Cha J, Lee MJ, Yu IW, Park MS, Seo WK, et al. Intensive statin treatment in acute ischaemic stroke patients with intracranial atherosclerosis: a high-resolution magnetic resonance imaging study (STAMINA-MRI Study). J Neurol Neurosurg Psychiatry. 2020; 91:204–211.
Article56. Miao H, Yang Y, Wang H, Huo L, Wang M, Zhou Y, et al. Intensive lipid-lowering therapy ameliorates asymptomatic intracranial atherosclerosis. Aging Dis. 2019; 10:258–266.
Article57. Bang OY. Intracranial atherosclerosis: current understanding and perspectives. J Stroke. 2014; 16:27–35.
Article58. Mazighi M, Labreuche J, Gongora-Rivera F, Duyckaerts C, Hauw JJ, Amarenco P. Autopsy prevalence of intracranial atherosclerosis in patients with fatal stroke. Stroke. 2008; 39:1142–1147.
Article59. Ryoo S, Park JH, Kim SJ, Kim GM, Chung CS, Lee KH, et al. Branch occlusive disease: clinical and magnetic resonance angiography findings. Neurology. 2012; 78:888–896.
Article60. Xu WH, Li ML, Gao S, Ni J, Zhou LX, Yao M, et al. Plaque distribution of stenotic middle cerebral artery and its clinical relevance. Stroke. 2011; 42:2957–2959.
Article61. Turan TN, Derdeyn CP, Fiorella D, Chimowitz MI. Treatment of atherosclerotic intracranial arterial stenosis. Stroke. 2009; 40:2257–2261.
Article62. Ryoo S, Lee MJ, Cha J, Jeon P, Bang OY. Differential vascular pathophysiologic types of intracranial atherosclerotic stroke: a high-resolution wall magnetic resonance imaging study. Stroke. 2015; 46:2815–2821.
Article63. Choi YJ, Jung SC, Lee DH. Vessel wall imaging of the intracranial and cervical carotid arteries. J Stroke. 2015; 17:238–255.
Article64. Ahn SH, Lee J, Kim YJ, Kwon SU, Lee D, Jung SC, et al. Isolated MCA disease in patients without significant atherosclerotic risk factors: a high-resolution magnetic resonance imaging study. Stroke. 2015; 46:697–703.65. Brinjikji W, Lehman VT, Kallmes DF, Rabinstein AA, Lanzino G, Murad MH, et al. The effects of statin therapy on carotid plaque composition and volume: a systematic review and meta-analysis. J Neuroradiol. 2017; 44:234–240.
Article66. Mujaj B, Bos D, Selwaness M, Leening MJG, Kavousi M, Wentzel JJ, et al. Statin use is associated with carotid plaque composition: the Rotterdam Study. Int J Cardiol. 2018; 260:213–218.
Article67. Amarenco P, Hobeanu C, Labreuche J, Charles H, Giroud M, Meseguer E, et al. Carotid atherosclerosis evolution when targeting a low-density lipoprotein cholesterol concentration <70 mg/dL after an ischemic stroke of atherosclerotic origin. Circulation. 2020; 142:748–757.68. Hussain MA, Saposnik G, Raju S, Salata K, Mamdani M, Tu JV, et al. Association between statin use and cardiovascular events after carotid artery revascularization. J Am Heart Assoc. 2018; 7:e009745.
Article69. Caplan LR. Atherosclerotic vertebral artery disease in the neck. Curr Treat Options Cardiovasc Med. 2003; 5:251–256.
Article70. Moossy J. Morphology, sites and epidemiology of cerebral atherosclerosis. Res Publ Assoc Res Nerv Ment Dis. 1966; 41:1–22.71. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2019; 73:e285–e350.72. Park HK, Lee JS, Hong KS, Cho YJ, Park JM, Kang K, et al. Statin therapy in acute cardioembolic stroke with no guidance-based indication. Neurology. 2020; 94:e1984–e1995.
Article73. Kusznir Vitturi B, José Gagliardi R. The role of statins in cardioembolic stroke. J Clin Neurosci. 2020; 72:174–179.
Article74. Wu YL, Saver JL, Chen PC, Lee JD, Wang HH, Rao NM, et al. Effect of statin use on clinical outcomes in ischemic stroke patients with atrial fibrillation. Medicine (Baltimore). 2017; 96:e5918.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent updates in dyslipidemia management: perspectives in stroke-specific situation
- Dyslipidemia Treatment and Cerebrovascular Disease: Evidence Regarding the Mechanism of Stroke
- Blood Pressure Management for Stroke Prevention and in Acute Stroke
- 2024 KSoLA Consensus on the Management of Secondary Dyslipidemia
- Changes of Plasma Lipids in Stroke Patients