Acute Crit Care.
2022 Aug;37(3):398-406. 10.4266/acc.2022.00192.
Clinical efficacy of blood purification using a polymethylmethacrylate hemofilter for the treatment of severe acute pancreatitis
- Affiliations
-
- 1Division of Blood Purification Therapy, Okinawa Kyodo Hospital, Okinawa, Japan
- 2Department of Gastroenterology, Okinawa Kyodo Hospital, Okinawa, Japan
- 3Intensive Care Unit, Okinawa Kyodo Hospital, Okinawa, Japan
- 4Department of Emergency Medicine, Okinawa Kyodo Hospital, Okinawa, Japan
- KMID: 2535304
- DOI: http://doi.org/10.4266/acc.2022.00192
Abstract
- Background
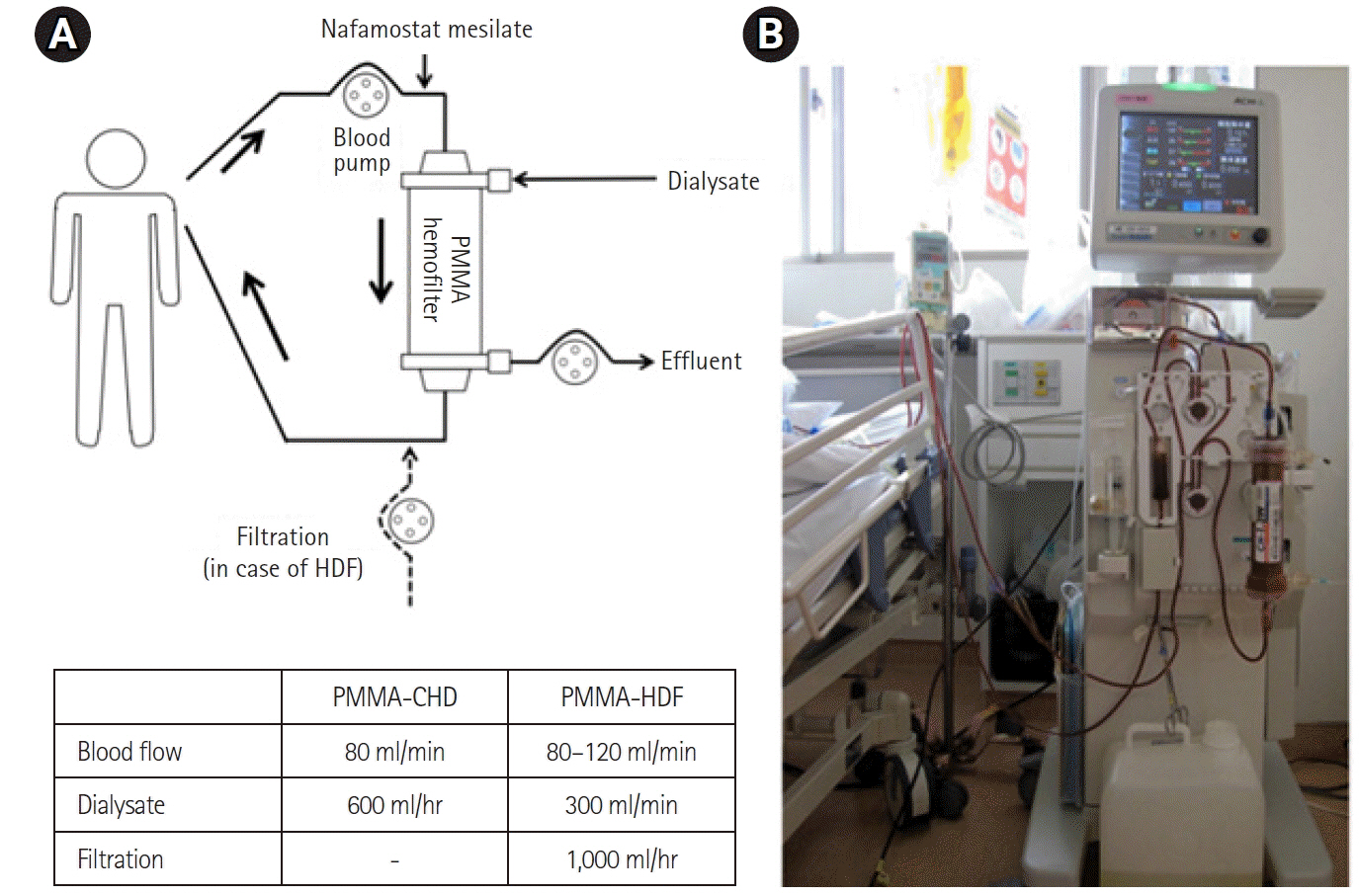
Severe acute pancreatitis (SAP) is a systemic inflammatory disease, and it can often complicate into acute kidney injury (AKI) and acute lung injury/acute respiratory distress syndrome (ALI/ARDS). This study aimed to evaluate the clinical effectiveness of blood purification using a polymethylmethacrylate (PMMA) hemofilter.
Methods
We retrospectively examined 54 patients, who were diagnosed with SAP according to the Japanese criteria from January 2011 to December 2019.
Results
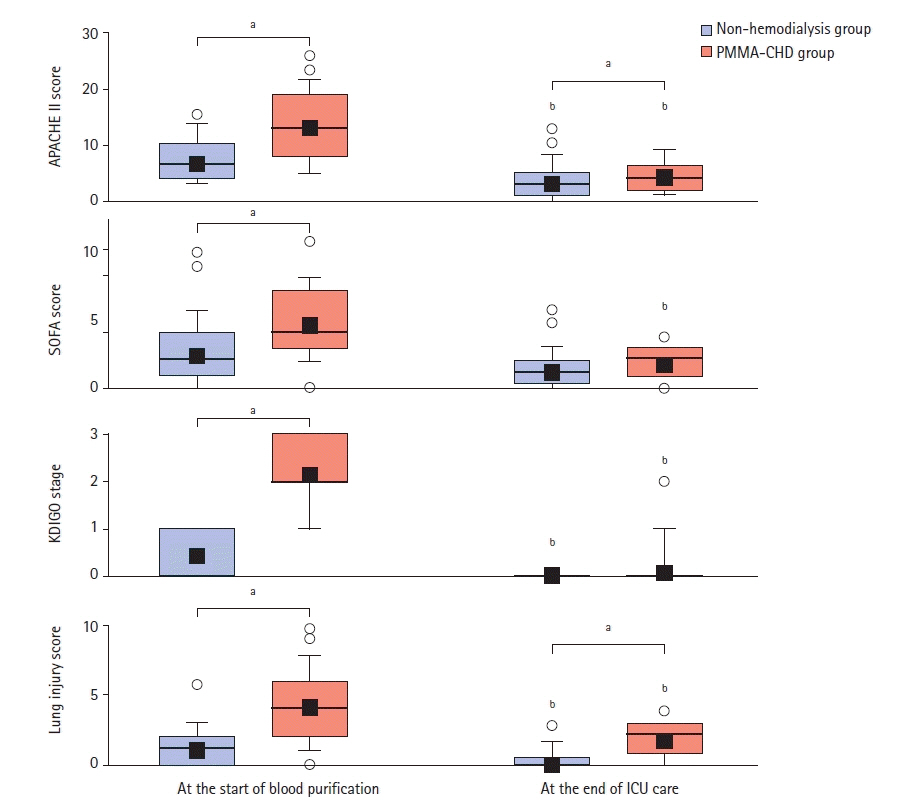
Of a total of 54 SAP patients, 26 patients progressively developed AKI and required continuous hemodialysis with a PMMA membrane hemofilter (PMMA-CHD). Acute Physiology and Chronic Health Evaluation (APACHE) II score and Sequential Organ Failure Assessment (SOFA) score were significantly higher in patients requiring PMMA-CHD than in patients not requiring hemodialysis. The lung injury scores were also significantly higher in patients requiring PMMA-CHD. Of the 26 patients, 16 patients developed ALI/ARDS and required mechanical ventilation. A total of seven patients developed severe ALI/ARDS and received additional intermittent hemodiafiltration using a PMMA hemofilter (PMMA-HDF). Although the length of intensive care unit stay was significantly longer in patients with severe ALI/ARDS, blood purification therapy was discontinued in all the patients. The survival rates at the time of discharge were 92.3% and 92.9% in patients with and without PMMA-CHD, respectively. These real mortality ratios were obviously lower than the estimated mortality ratios predicted by APACHE II scores.
Conclusions
These finding suggest that the blood purification using a PMMA hemofilter would be effective for the treatment of AKI and ALI/ARDS in SAP patients.
Keyword
Figure
Reference
-
1. Garg PK, Singh VP. Organ failure due to systemic injury in acute pancreatitis. Gastroenterology. 2019; 156:2008–23.2. Zhou J, Li Y, Tang Y, Liu F, Yu S, Zhang L, et al. Effect of acute kidney injury on mortality and hospital stay in patient with severe acute pancreatitis. Nephrology (Carlton). 2015; 20:485–91.3. Nassar TI, Qunibi WY. AKI associated with acute pancreatitis. Clin J Am Soc Nephrol. 2019; 14:1106–15.4. Devani K, Charilaou P, Radadiya D, Brahmbhatt B, Young M, Reddy C. Acute pancreatitis: trends in outcomes and the role of acute kidney injury in mortality: a propensity-matched analysis. Pancreatology. 2018; 18:870–7.5. Hu Y, Xiong W, Li C, Cui Y. Continuous blood purification for severe acute pancreatitis: a systematic review and meta-analysis. Medicine (Baltimore). 2019; 98:e14873.6. Kumar P, Gupta P, Rana S. Thoracic complications of pancreatitis. JGH Open. 2018; 3:71–9.7. Hirayama Y, Oda S, Wakabayashi K, Sadahiro T, Nakamura M, Watanabe E, et al. Comparison of interleukin-6 removal properties among hemofilters consisting of varying membrane materials and surface areas: an in vitro study. Blood Purif. 2011; 31:18–25.8. Yamashita AC, Tomisawa N. Membrane materials for blood purification in critical care. Contrib Nephrol. 2010; 166:112–8.9. Nakada TA, Oda S, Matsuda K, Sadahiro T, Nakamura M, Abe R, et al. Continuous hemodiafiltration with PMMA Hemofilter in the treatment of patients with septic shock. Mol Med. 2008; 14:257–63.10. Matsuda K, Moriguchi T, Oda S, Hirasawa H. Efficacy of continuous hemodiafiltration with a cytokine-adsorbing hemofilter in the treatment of acute respiratory distress syndrome. Contrib Nephrol. 2010; 166:83–92.
Article11. Abe R, Oda S, Shinozaki K, Hirasawa H. Continuous hemodiafiltration using a polymethyl methacrylate membrane hemofilter for severe acute pancreatitis. Contrib Nephrol. 2010; 166:54–63.
Article12. Ikeura T, Horibe M, Sanui M, Sasaki M, Kuwagata Y, Nishi K, et al. Validation of the efficacy of the prognostic factor score in the Japanese severity criteria for severe acute pancreatitis: a large multicenter study. United European Gastroenterol J. 2017; 5:389–97.
Article13. Yokoe M, Takada T, Mayumi T, Yoshida M, Isaji S, Wada K, et al. Japanese guidelines for the management of acute pancreatitis: Japanese Guidelines 2015. J Hepatobiliary Pancreat Sci. 2015; 22:405–32.
Article14. Nishida O, Nakamura T, Kuriyama N, Hara Y, Yumoto M, Shimomura Y, et al. Sustained high-efficiency daily diafiltration using a mediator-adsorbing membrane (SHEDD-fA) in the treatment of patients with severe sepsis. Contrib Nephrol. 2011; 173:172–81.
Article15. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.16. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.
Article17. Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990; 174:331–6.
Article18. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012; 120:c179–84.
Article19. Murray JF, Matthay MA, Luce JM, Flick MR. An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis. 1988; 138:720–3.
Article20. Kobashi S, Maruhashi T, Nakamura T, Hatabayashi E, Kon A. The 28-day survival rates of two cytokine-adsorbing hemofilters for continuous renal replacement therapy: a single-center retrospective comparative study. Acute Med Surg. 2018; 6:60–7.
Article21. Sharma D, Jakkampudi A, Reddy R, Reddy PB, Patil A, Murthy HV, et al. Association of systemic inflammatory and anti-inflammatory responses with adverse outcomes in acute pancreatitis: preliminary results of an ongoing study. Dig Dis Sci. 2017; 62:3468–78.
Article22. Cui HX, Xu JY, Li MQ. Efficacy of continuous renal replacement therapy in the treatment of severe acute pancreatitis associated acute respiratory distress syndrome. Eur Rev Med Pharmacol Sci. 2014; 18:2523–6.23. Rasch S, Sancak S, Erber J, Wießner J, Schulz D, Huberle C, et al. Influence of extracorporeal cytokine adsorption on hemodynamics in severe acute pancreatitis: results of the matched cohort pancreatitis cytosorbents inflammatory cytokine removal (PACIFIC) study. Artif Organs. 2022; Feb. 19. [Epub]. https://doi.org/10.1111/aor.14195.
Article24. Zhou MT, Chen CS, Chen BC, Zhang QY, Andersson R. Acute lung injury and ARDS in acute pancreatitis: mechanisms and potential intervention. World J Gastroenterol. 2010; 16:2094–9.
Article25. Gougol A, Dugum M, Dudekula A, Greer P, Slivka A, Whitcomb DC, et al. Clinical outcomes of isolated renal failure compared to other forms of organ failure in patients with severe acute pancreatitis. World J Gastroenterol. 2017; 23:5431–7.
Article26. Winkelman C, Johnson KD, Gordon N. Associations between muscle-related cytokines and selected patient outcomes in the ICU. Biol Res Nurs. 2015; 17:125–34.
Article27. Oshihara W, Fujieda H, Ueno Y. A new poly(methyl methacrylate) membrane dialyzer, NF, with adsorptive and antithrombotic properties. Contrib Nephrol. 2017; 189:230–6.
Article28. Yuzawa H, Hirose Y, Kimura T, Shinozaki K, Oguchi M, Morito T, et al. Filter lifetimes of different hemodiafiltration membrane materials in dogs: reevaluation of the optimal anticoagulant dosage. Ren Replace Ther. 2021; 7:7.
Article29. Hattori N, Oda S. Cytokine-adsorbing hemofilter: old but new modality for septic acute kidney injury. Ren Replace Ther. 2016; 2:41.
Article30. Duriseti P, Idrees N, Aldairem A, Jaber BL, Balakrishnan VS. Cost analysis of two modalities of continuous renal replacement therapy. Hemodial Int. 2021; 25:173–9.
Article