Endocrinol Metab.
2022 Oct;37(5):781-790. 10.3803/EnM.2022.1532.
Association of Shift Work with Normal-Weight Obesity in Community-Dwelling Adults
- Affiliations
-
- 1Yonsei University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2534630
- DOI: http://doi.org/10.3803/EnM.2022.1532
Abstract
- Background
Shift work is associated with obesity and metabolic syndrome. However, this association in the normal-weight population remains unclear. This study aimed to investigate whether shift work is associated with normal-weight obesity (NWO).
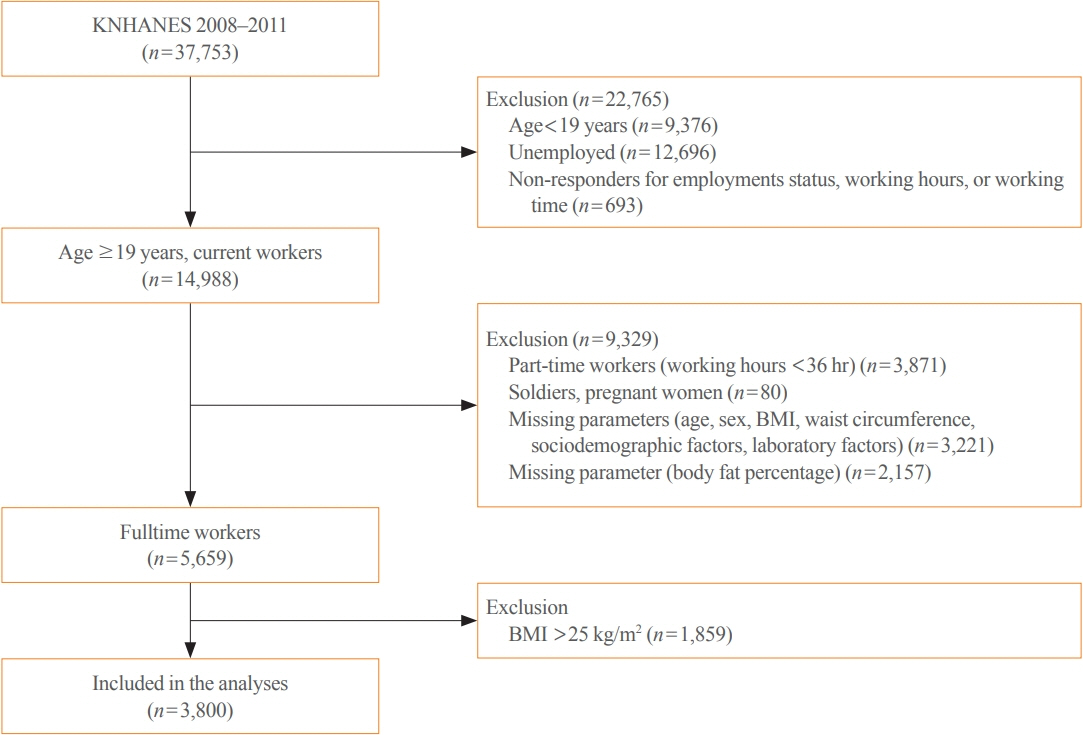
Methods
From the nationally representative Korea National Health and Nutrition Examination Survey (KNHANES) dataset (2008 to 2011), 3,800 full-time workers aged ≥19 years with a body mass index (BMI) ≤25 kg/m2 were analysed. We defined NWO as BMI ≤25 kg/m2 and body fat percentage ≥25% in men and ≥37% in women. Working patterns were classified into “daytime,” “other than daytime,” and “shift.” Multivariable logistic regression analysis was performed to evaluate the relationship between shift work and NWO.
Results
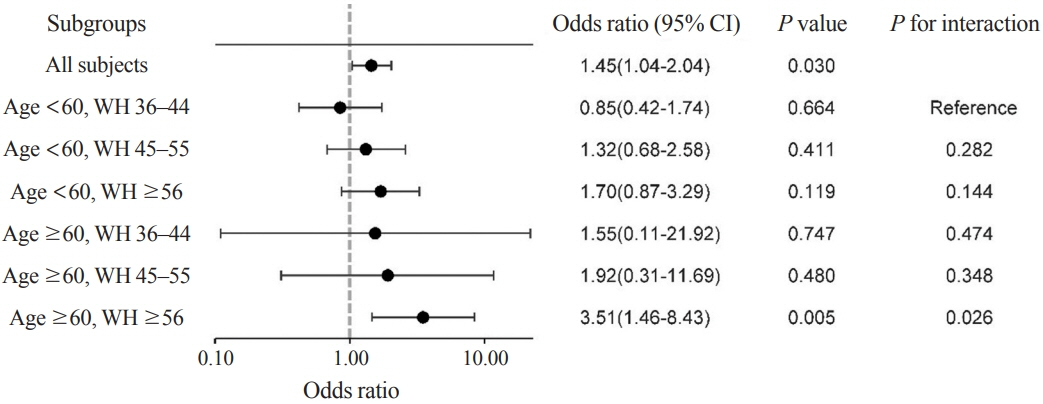
Shift work was associated with higher odds of NWO than daytime work (adjusted odds ratio [aOR], 1.47; 95% confidence interval [CI], 1.04 to 2.09) and night/evening work (aOR, 1.87; 95% CI, 1.11 to 3.14) after adjustment for type of work, working hours, age, sex, BMI, 25-hydroxyvitamin D levels, homeostatic model assessment for insulin resistance, and other sociodemographic factors. In subgroup analyses, the association between shift work and NWO was more robust in those aged ≥60 years and those working ≥56 hours/week.
Conclusion
Shift work was associated with NWO in community-dwelling Korean adults, independent of age, sex, BMI, and other covariates.
Figure
Cited by 2 articles
-
You Can’t Avoid Shift Work? Then Focus on Body Fat Rather than Weight
Eun Kyung Lee
Endocrinol Metab. 2022;37(5):756-758. doi: 10.3803/EnM.2022.501.
Reference
-
1. Williams C. Work-life balance of shift workers. Perspect Labour Income. 2008; 9:5–16.2. Messenger J. ILO future of work research paper series: working time and the future of work. Geneva: International Labour Organization;2018. p. 44.3. Wilczynska A, Cabrita J, Parent-Thirion A, Biletta I, Vargas O, et al. 6th European working conditions survey: 2017 update. Luxembourg: Publications Office of the European Union;2017. [cited 2022 Sep 29]. Available from: https://data.europa.eu/doi/10.2806/422172.4. Baek K, Ha K. Work characteristics and health status of shift workers based on the results of the Fifth Korean Working Conditions Survey. J Korean Soc Occup Environ Hyg. 2019; 29:550–61.5. Oosterman JE, Wopereis S, Kalsbeek A. The circadian clock, shift work, and tissue-specific insulin resistance. Endocrinology. 2020; 161:bqaa180.
Article6. Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001; 58:747–52.7. Rivera AS, Akanbi M, O’Dwyer LC, McHugh M. Shift work and long work hours and their association with chronic health conditions: a systematic review of systematic reviews with meta-analyses. PLoS One. 2020; 15:e0231037.
Article8. Liu Q, Shi J, Duan P, Liu B, Li T, Wang C, et al. Is shift work associated with a higher risk of overweight or obesity? A systematic review of observational studies with meta-analysis. Int J Epidemiol. 2018; 47:1956–71.
Article9. McGlynn N, Kirsh VA, Cotterchio M, Harris MA, Nadalin V, Kreiger N. Shift work and obesity among Canadian women: a cross-sectional study using a novel exposure assessment tool. PLoS One. 2015; 10:e0137561.
Article10. De Lorenzo A, Soldati L, Sarlo F, Calvani M, Di Lorenzo N, Di Renzo L. New obesity classification criteria as a tool for bariatric surgery indication. World J Gastroenterol. 2016; 22:681–703.
Article11. Franco LP, Morais CC, Cominetti C. Normal-weight obesity syndrome: diagnosis, prevalence, and clinical implications. Nutr Rev. 2016; 74:558–70.
Article12. Wijayatunga NN, Dhurandhar EJ. Normal weight obesity and unaddressed cardiometabolic health risk-a narrative review. Int J Obes (Lond). 2021; 45:2141–55.
Article13. Hong S, Oh HJ, Choi H, Kim JG, Lim SK, Kim EK, et al. Characteristics of body fat, body fat percentage and other body composition for Koreans from KNHANES IV. J Korean Med Sci. 2011; 26:1599–605.
Article14. Korea Labor Institute. Center for labor policy analysis 2015. Sejong: Korea Labor Institute;2015.15. Son M, Ye BJ, Kim JI, Kang S, Jung KY. Association between shift work and obesity according to body fat percentage in Korean wage workers: data from the fourth and the fifth Korea National Health and Nutrition Examination Survey (KNHANES 2008-2011). Ann Occup Environ Med. 2015; 27:32.
Article16. Riley EC. International standard classification of occupations. Geneva: Lippincott Williams & Wilkins;1959.17. Dickey RA, Bartuska D, Bray GW, Callaway CW, Davidson ET, Feld S, et al. AACE/ACE position statement on the prevention, diagnosis, and treatment of obesity (1998 revision). Endocr Pract. 1998; 4:297–350.18. Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F. The concept of normal weight obesity. Prog Cardiovasc Dis. 2014; 56:426–33.
Article19. Kim MK, Han K, Kwon HS, Song KH, Yim HW, Lee WC, et al. Normal weight obesity in Korean adults. Clin Endocrinol (Oxf). 2014; 80:214–20.
Article20. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003; 35:1381–95.
Article21. Zarrinpar A, Chaix A, Panda S. Daily eating patterns and their impact on health and disease. Trends Endocrinol Metab. 2016; 27:69–83.
Article22. Bayon V, Leger D, Gomez-Merino D, Vecchierini MF, Chennaoui M. Sleep debt and obesity. Ann Med. 2014; 46:264–72.
Article23. Hulsegge G, Boer JM, van der Beek AJ, Verschuren WM, Sluijs I, Vermeulen R, et al. Shift workers have a similar diet quality but higher energy intake than day workers. Scand J Work Environ Health. 2016; 42:459–68.
Article24. Nishitani N, Sakakibara H. Relationship of obesity to job stress and eating behavior in male Japanese workers. Int J Obes (Lond). 2006; 30:528–33.
Article25. Stenvers DJ, Scheer FA, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019; 15:75–89.
Article26. de Goede P, Sen S, Oosterman JE, Foppen E, Jansen R, la Fleur SE, et al. Differential effects of diet composition and timing of feeding behavior on rat brown adipose tissue and skeletal muscle peripheral clocks. Neurobiol Sleep Circadian Rhythms. 2017; 4:24–33.
Article27. Kim TW, Jeong JH, Hong SC. The impact of sleep and circadian disturbance on hormones and metabolism. Int J Endocrinol. 2015; 2015:591729.
Article28. Manenschijn L, van Kruysbergen RG, de Jong FH, Koper JW, van Rossum EF. Shift work at young age is associated with elevated long-term cortisol levels and body mass index. J Clin Endocrinol Metab. 2011; 96:E1862–5.
Article29. Lee GJ, Kim K, Kim SY, Kim JH, Suh C, Son BC, et al. Effects of shift work on abdominal obesity among 20-39-year-old female nurses: a 5-year retrospective longitudinal study. Ann Occup Environ Med. 2016; 28:69.
Article30. Shan Z, Li Y, Zong G, Guo Y, Li J, Manson JE, et al. Rotating night shift work and adherence to unhealthy lifestyle in predicting risk of type 2 diabetes: results from two large US cohorts of female nurses. BMJ. 2018; 363:k4641.
Article31. Sun M, Feng W, Wang F, Zhang L, Wu Z, Li Z, et al. Night shift work exposure profile and obesity: baseline results from a Chinese night shift worker cohort. PLoS One. 2018; 13:e0196989.
Article32. Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. Int J Obes (Lond). 2010; 34:791–9.
Article33. Bae JC, Cho NH, Kim JH, Hur KY, Jin SM, Lee MK. Association of body mass index with the risk of incident type 2 diabetes, cardiovascular disease, and all-cause mortality: a community-based prospective study. Endocrinol Metab (Seoul). 2020; 35:416–24.
Article34. Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002; 3:141–6.
Article35. Martinez KE, Tucker LA, Bailey BW, LeCheminant JD. Expanded normal weight obesity and insulin resistance in US adults of the National Health and Nutrition Examination Survey. J Diabetes Res. 2017; 2017:9502643.
Article36. Ohlsson B, Manjer J. Sociodemographic and lifestyle factors in relation to overweight defined by BMI and “normal-weight obesity”. J Obes. 2020; 2020:2070297.
Article37. Hulsegge G, van Mechelen W, Paagman H, Proper KI, Anema JR. The moderating role of lifestyle, age, and years working in shifts in the relationship between shift work and being overweight. Int Arch Occup Environ Health. 2020; 93:697–705.
Article38. Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. 2016; 355:i5210.
Article39. Guner U, Guner N. The relationship between long working hours and weight gain in older workers in Europe. Work. 2020; 67:753–9.40. Ho-Pham LT, Campbell LV, Nguyen TV. More on body fat cutoff points. Mayo Clin Proc. 2011; 86:584.
Article41. Marques-Vidal P, Chiolero A, Paccaud F. Large differences in the prevalence of normal weight obesity using various cut-offs for excess body fat. E Spen Eur E J Clin Nutr Metab. 2008; 3:e159–62.
Article42. Kwon H, Kim D, Kim JS. Body fat distribution and the risk of incident metabolic syndrome: a longitudinal cohort study. Sci Rep. 2017; 7:10955.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Contributing to Low Weight in Community-Dwelling Older Adults
- Association between Objectively Measured Sleep Quality and Obesity in Community-dwelling Adults Aged 80 Years or Older: A Cross-sectional Study
- Linear Association between Frailty as Assessed by the Kihon Checklist and Quality of Life in Community-Dwelling Older Adults: A Cross-Sectional Population-Based Study
- Comparison of Functional Independence among Community-dwelling Older Adults in Rural Areas in South Korea and the United States
- Comparison of Comprehensive Health Status and Health-related Quality of Life between Institutionalized Older Adults and Community Dwelling Older Adults