Korean J Pain.
2022 Oct;35(4):361-382. 10.3344/kjp.2022.35.4.361.
Prevention, diagnosis, and treatment of opioid use disorder under the supervision of opioid stewardship programs: it’s time to act now
- Affiliations
-
- 1Department of Pharmacy, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Department of Anesthesia and Pain Medicine, School of Medicine, Pusan National University, Yangsan, Korea
- KMID: 2533977
- DOI: http://doi.org/10.3344/kjp.2022.35.4.361
Abstract
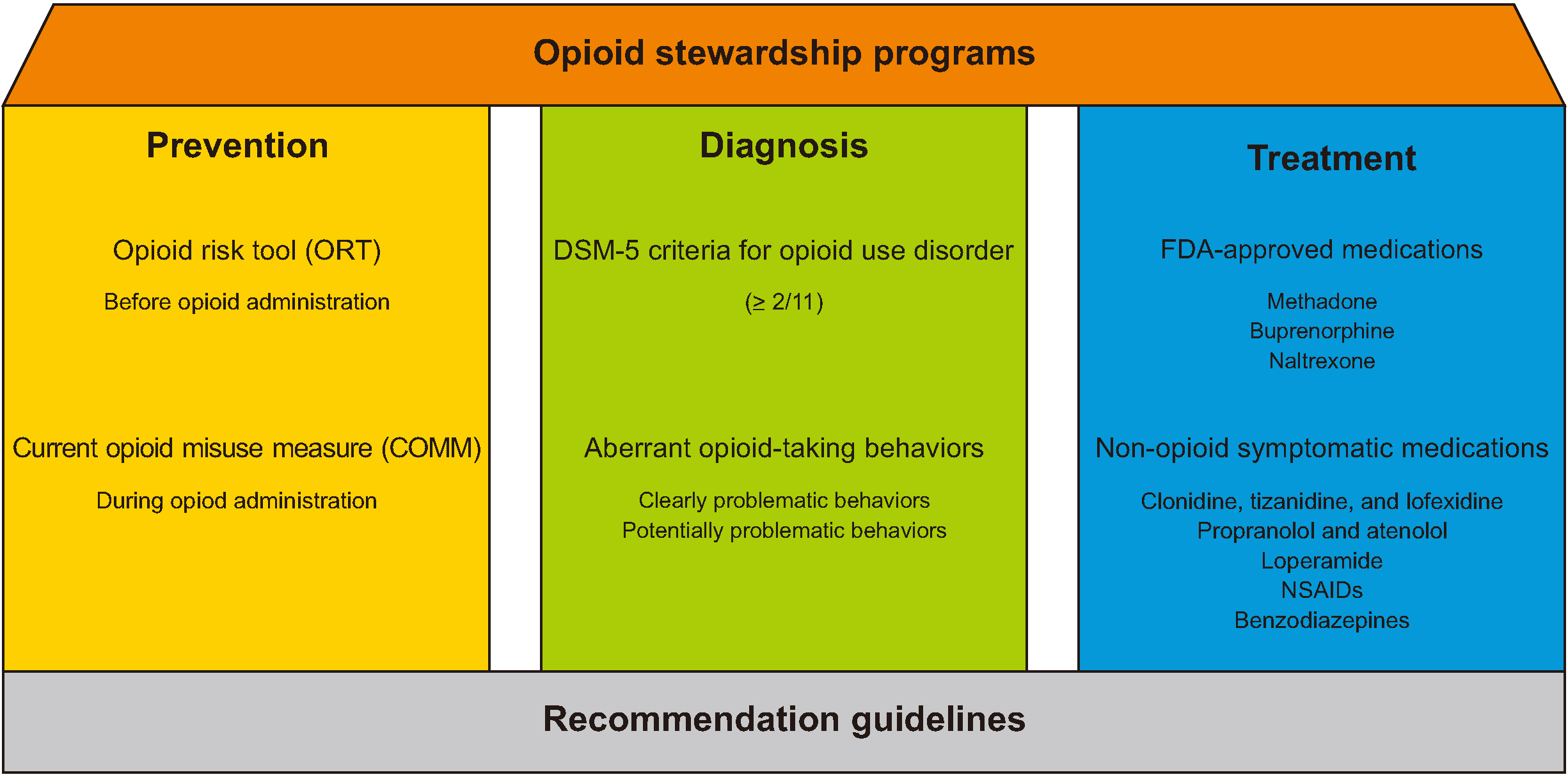
- The third opium war may have already started, not only due to illicit opioid trafficking from the Golden Crescent and Golden Triangle on the international front but also through indiscriminate opioid prescription and opioid diversion at home. Opioid use disorder (OUD), among unintentional injuries, has become one of the top 4 causes of death in the United States (U.S.). An OUD is defined as a problematic pattern of opioid use resulting in clinically significant impairment or distress, consisting of 2 or more of 11 problems within 1 year, as described by the Diagnostic and Statistical Manual for Mental Disorders, Fifth Edition. Observation of aberrant behaviors of OUD is also helpful for overworked clinicians. For the prevention of OUD, the Opioid Risk Tool and the Current Opioid Misuse Measure are appropriate screening tests before and during opioid administration, respectively. Treatment of OUD consists of 3 opioid-based U.S. Food and Drug Administration-approved medications, including methadone, buprenorphine, and naltrexone, and non-opioid-based symptomatic medications for reducing opioid withdrawal syndromes, such as α 2 agonists, β-blockers, antidiarrheals, antiemetics, non-steroidal anti-inflammatory drugs, and benzodiazepines. There are at least 6 recommendable guidelines and essential terms related to OUD. Opioid stewardship programs are now critical to promoting appropriate use of opioid medications, improving patient outcomes, and reducing misuse of opioids, influenced by the successful implementation of antimicrobial stewardship programs. Despite the lack of previous motivation, now is the critical time for trying to reduce the risk of OUD.
Keyword
Figure
Cited by 1 articles
-
Addressing the opioid crisis in the Philippines: recognizing the severity and calling for proactive action
Dalmacito A. Cordero Jr.
Korean J Pain. 2024;37(2):182-184. doi: 10.3344/kjp.24020.
Reference
-
1. Shapiro JL. 2019; The third opium war?: understanding China through history. Horizons. 13:52–65.2. Jayawardana S, Forman R, Johnston-Webber C, Campbell A, Berterame S, de Joncheere C, et al. 2021; Global consumption of prescription opioid analgesics between 2009-2019: a country-level observational study. EClinicalMedicine. 42:101198. DOI: 10.1016/j.eclinm.2021.101198. PMID: 34820610. PMCID: PMC8599097. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85119043938&origin=inward.
Article3. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. 2016; Increases in drug and opioid overdose deaths--United States, 2000-2014. MMWR Morb Mortal Wkly Rep. 64:1378–82. DOI: 10.15585/mmwr.mm6450a3. PMID: 26720857. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84955313404&origin=inward.
Article4. Soffin EM, Lee BH, Kumar KK, Wu CL. 2019; The prescription opioid crisis: role of the anaesthesiologist in reducing opioid use and misuse. Br J Anaesth. 122:e198–208. DOI: 10.1016/j.bja.2018.11.019. PMID: 30915988. PMCID: PMC8176648. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85059153949&origin=inward.
Article5. Yang J, Bauer BA, Wahner-Roedler DL, Chon TY, Xiao L. 2020; The modified WHO analgesic ladder: is it appropriate for chronic non-cancer pain? J Pain Res. 13:411–7. DOI: 10.2147/JPR.S244173. PMID: 32110089. PMCID: PMC7038776. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85079665468&origin=inward.6. Woolf CJ. 2020; Capturing novel non-opioid pain targets. Biol Psychiatry. 87:74–81. DOI: 10.1016/j.biopsych.2019.06.017. PMID: 31399256. PMCID: PMC6898770. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85075107861&origin=inward.
Article7. Siegel RL, Miller KD, Fuchs HE, Jemal A. 2021; Cancer statistics, 2021. CA Cancer J Clin. 71:7–33. Erratum in: CA Cancer J Clin 2021; 71: 359. DOI: 10.3322/caac.21654. PMID: 33433946. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85099242992&origin=inward.
Article8. Collett BJ. 2001; Chronic opioid therapy for non-cancer pain. Br J Anaesth. 87:133–43. DOI: 10.1093/bja/87.1.133. PMID: 11460802. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0034940234&origin=inward.
Article9. Classification of chronic pain. 1986; Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 3:S1–226. PMID: 3461421. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0022523784&origin=inward.10. Uritsky TJ, Busch ME, Chae SG, Genord C. 2020; Opioid stewardship: building on antibiotic stewardship principles. J Pain Palliat Care Pharmacother. 34:181–3. DOI: 10.1080/15360288.2020.1765066. PMID: 32757904. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85089077066&origin=inward.
Article11. Centers for Disease Control and Prevention (CDC). 2019. Core elements of hospital antibiotic stewardship programs [Internet]. CDC;Atlanta (GA): Available at: https://www.cdc.gov/antibiotic-use/healthcare/pdfs/hospital-core-elements-H.pdf.12. Institute for Safe Medication Practices (ISMP) Canada. 2017. Opioid stewardship [Internet]. ISMP Canada;Toronto (ON): Available at: https://www.ismp-canada.org/opioid_stewardship/.13. Dowell D, Haegerich TM, Chou R. 2016; CDC guideline for prescribing opioids for chronic pain--United States, 2016. JAMA. 315:1624–45. DOI: 10.1001/jama.2016.1464. PMID: 26977696. PMCID: PMC6390846. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84964402250&origin=inward.
Article14. National Quality Forum (NQF). 2018. National Quality Partners PlaybookTM: opioid stewardship. NQF;Washington, D.C.: DOI: 10.1080/15360288.2020.1765066. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85089077066&origin=inward.15. American Hospital Association (AHA). 2020. Stem the tide: opioid stewardship measurement implementation guide [Internet]. AHA;Chicago (IL): https://www.aha.org/system/files/media/file/2020/07/HIIN-opioid-guide-0520.pdf.16. Trescot AM, Datta S, Lee M, Hansen H. 2008; Opioid pharmacology. Pain Physician. 11(2 Suppl):S133–53. DOI: 10.36076/ppj.2008/11/S133. PMID: 18443637.
Article17. World Health Organization (WHO). 2009. Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence. WHO Press;Geneva: p. 5. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=43649084815&origin=inward.18. World Health Organization (WHO). 2016. ICD-10. International statistical classification of diseases and related health problems. 10th ed. WHO Press;Geneva: p. 289–92. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=43649084815&origin=inward.19. World Health Organization (WHO). 2022. International Classification of Diseases 11th edition: the global standard for diagnostic health information [Internet]. Available at: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1023217081.20. American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Association Publishing;Washington, D.C.: p. 1–947. DOI: 10.1176/appi.books.9780890425596.21. Brady KT, McCauley JL, Back SE. 2016; Prescription opioid misuse, abuse, and treatment in the United States: an update. Am J Psychiatry. 173:18–26. DOI: 10.1176/appi.ajp.2015.15020262. PMID: 26337039. PMCID: PMC4782928. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84954305419&origin=inward.
Article22. Volkow ND, McLellan AT. 2016; Opioid abuse in chronic pain--misconceptions and mitigation strategies. N Engl J Med. 374:1253–63. DOI: 10.1056/NEJMra1507771. PMID: 27028915. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84962349036&origin=inward.
Article23. Ballantyne JC, LaForge SK. 2007; Opioid dependence and addiction during opioid treatment of chronic pain. Pain. 129:235–55. Erratum in: Pain 2007; 131: 350. DOI: 10.1016/j.pain.2007.07.021. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34548493466&origin=inward.
Article24. ivastava AB Sr, Mariani JJ, Levin FR. 2020; New directions in the treatment of opioid withdrawal. Lancet. 395:1938–48. DOI: 10.1016/S0140-6736(20)30852-7. PMID: 32563380. PMCID: PMC7385662. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086515264&origin=inward.
Article25. Kosten TR, Baxter LE. 2019; Review article: effective management of opioid withdrawal symptoms: a gateway to opioid dependence treatment. Am J Addict. 28:55–62. DOI: 10.1111/ajad.12862. PMID: 30701615. PMCID: PMC6590307. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85060992029&origin=inward.
Article26. Inciardi JA, Surratt HL, Lugo Y, Cicero TJ. 2007; The diversion of prescription opioid analgesics. Law Enforc Exec Forum. 7:127–41. PMID: 25267926. PMCID: PMC4176900.27. Iwanicki JL, Severtson SG, McDaniel H, Rosenblum A, Fong C, Cicero TJ, et al. 2016; Abuse and diversion of immediate release opioid analgesics as compared to extended release formulations in the United States. PLoS One. 11:e0167499. DOI: 10.1371/journal.pone.0167499. PMID: 27936038. PMCID: PMC5147916. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85006062465&origin=inward.
Article28. Berge KH, Dillon KR, Sikkink KM, Taylor TK, Lanier WL. 2012; Diversion of drugs within health care facilities, a multiple-victim crime: patterns of diversion, scope, consequences, detection, and prevention. Mayo Clin Proc. 87:674–82. DOI: 10.1016/j.mayocp.2012.03.013. PMID: 22766087. PMCID: PMC3538481. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84863441502&origin=inward.
Article29. Perry JC, Vandenhouten CL. 2019; Drug diversion detection. Nurs Manage. 50:16–21. DOI: 10.1097/01.NUMA.0000552735.56577.4b. PMID: 30652981. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85060569629&origin=inward.
Article30. O'Brien T, Christrup LL, Drewes AM, Fallon MT, Kress HG, McQuay HJ, et al. 2017; European Pain Federation position paper on appropriate opioid use in chronic pain management. Eur J Pain. 21:3–19. DOI: 10.1002/ejp.970. PMID: 27991730. PMCID: PMC6680203. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85006314811&origin=inward.31. Nafziger AN, Barkin RL. 2018; Opioid therapy in acute and chronic pain. J Clin Pharmacol. 58:1111–22. DOI: 10.1002/jcph.1276. PMID: 29985526. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85050489634&origin=inward.
Article32. Gustorff B, Nahlik G, Hoerauf KH, Kress HG. 2002; The absence of acute tolerance during remifentanil infusion in volunteers. Anesth Analg. 94:1223–8. DOI: 10.1097/00000539-200205000-00032. PMID: 11973194. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0036233609&origin=inward.
Article33. Cortínez LI, Brandes V, Muñoz HR, Guerrero ME, Mur M. 2001; No clinical evidence of acute opioid tolerance after remifentanil-based anaesthesia. Br J Anaesth. 87:866–9. DOI: 10.1093/bja/87.6.866. PMID: 11878688. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0035199571&origin=inward.
Article34. Guignard B, Bossard AE, Coste C, Sessler DI, Lebrault C, Alfonsi P, et al. 2000; Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 93:409–17. DOI: 10.1097/00000542-200008000-00019. PMID: 10910490. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0033860934&origin=inward.35. Yu EH, Tran DH, Lam SW, Irwin MG. 2016; Remifentanil tolerance and hyperalgesia: short-term gain, long-term pain? Anaesthesia. 71:1347–62. DOI: 10.1111/anae.13602. PMID: 27734470. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84994876841&origin=inward.
Article36. Ilkjaer S, Petersen KL, Brennum J, Wernberg M, Dahl JB. 1996; Effect of systemic N-methyl-D-aspartate receptor antagonist (ketamine) on primary and secondary hyperalgesia in humans. Br J Anaesth. 76:829–34. DOI: 10.1093/bja/76.6.829. PMID: 8679358. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0030006460&origin=inward.
Article37. Felsby S, Nielsen J, Arendt-Nielsen L, Jensen TS. 1996; NMDA receptor blockade in chronic neuropathic pain: a comparison of ketamine and magnesium chloride. Pain. 64:283–91. DOI: 10.1016/0304-3959(95)00113-1. PMID: 8740606. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0029988675&origin=inward.
Article38. Ramasubbu C, Gupta A. 2011; Pharmacological treatment of opioid-induced hyperalgesia: a review of the evidence. J Pain Palliat Care Pharmacother. 25:219–30. DOI: 10.3109/15360288.2011.589490. PMID: 21834699. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=82155180464&origin=inward.
Article39. Kim KH. 2014; Safe sedation and hypnosis using dexmedetomidine for minimally invasive spine surgery in a prone position. Korean J Pain. 27:313–20. DOI: 10.3344/kjp.2014.27.4.313. PMID: 25317279. PMCID: PMC4196495. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84907803142&origin=inward.
Article40. Zhao Y, He J, Yu N, Jia C, Wang S. 2020; Mechanisms of dexmedetomidine in neuropathic pain. Front Neurosci. 14:330. DOI: 10.3389/fnins.2020.00330. PMID: 32431587. PMCID: PMC7214625. PMID: 6f02da2b70c84fc88c5da551bbede601. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85085210624&origin=inward.
Article41. Grape S, Kirkham KR, Frauenknecht J, Albrecht E. 2019; Intra-operative analgesia with remifentanil vs. dexmedetomidine: a systematic review and meta-analysis with trial sequential analysis. Anaesthesia. 74:793–800. DOI: 10.1111/anae.14657. PMID: 30950522. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85063896909&origin=inward.
Article42. Kim KH, Seo HJ, Abdi S, Huh B. 2020; All about pain pharmacology: what pain physicians should know. Korean J Pain. 33:108–20. DOI: 10.3344/kjp.2020.33.2.108. PMID: 32235011. PMCID: PMC7136290. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85091120149&origin=inward.
Article43. Conrad KA, Fagan TC, Mackie MJ, Mayshar PV. 1988; Effects of ketorolac tromethamine on hemostasis in volunteers. Clin Pharmacol Ther. 43:542–6. DOI: 10.1038/clpt.1988.70. PMID: 3259170. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0023880911&origin=inward.
Article44. Shrestha M, Chen A. 2018; Modalities in managing postherpetic neuralgia. Korean J Pain. 31:235–43. DOI: 10.3344/kjp.2018.31.4.235. PMID: 30310548. PMCID: PMC6177534. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85054667459&origin=inward.
Article45. Raja SN, Haythornthwaite JA, Pappagallo M, Clark MR, Travison TG, Sabeen S, et al. 2002; Opioids versus antidepressants in postherpetic neuralgia: a randomized, placebo-controlled trial. Neurology. 59:1015–21. DOI: 10.1212/WNL.59.7.1015. PMID: 12370455. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0037044286&origin=inward.
Article46. Adejumo AC, Akanbi O, Alayo Q, Ejigah V, Onyeakusi NE, Omede OF, et al. 2021; Predictors, rates, and trends of opioid use disorder among patients hospitalized with chronic pancreatitis. Ann Gastroenterol. 34:262–72. DOI: 10.20524/aog.2021.0579. PMID: 33654369. PMCID: PMC7903576. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85103042445&origin=inward.
Article47. Toskes PP. 2001; Alcohol consumption and chronic pancreatitis. Mayo Clin Proc. 76:241. DOI: 10.4065/76.3.241. PMID: 11243269. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0035095325&origin=inward.
Article48. Berna C, Kulich RJ, Rathmell JP. 2015; Tapering long-term opioid therapy in chronic noncancer pain: evidence and recommendations for everyday practice. Mayo Clin Proc. 90:828–42. DOI: 10.1016/j.mayocp.2015.04.003. PMID: 26046416. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84930989592&origin=inward.49. Palmer G. 2015; Complex regional pain syndrome. Aust Prescr. 38:82–6. DOI: 10.18773/austprescr.2015.029. PMID: 26648626. PMCID: PMC4653964. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84933042590&origin=inward.
Article50. Donegan D, Bancos I. 2018; Opioid-induced adrenal insufficiency. Mayo Clin Proc. 93:937–44. DOI: 10.1016/j.mayocp.2018.04.010. PMID: 29976376. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85048943337&origin=inward.
Article51. Lee SJ, Yoo YM, You JA, Shin SW, Kim TK, Abdi S, et al. 2019; Successful removal of permanent spinal cord stimulators in patients with complex regional pain syndrome after complete relief of pain. Korean J Pain. 32:47–50. DOI: 10.3344/kjp.2018.32.1.47. PMID: 30671203. PMCID: PMC6333578. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85059589194&origin=inward.
Article52. Koulousakis A, Kuchta J, Bayarassou A, Sturm V. 2007; Intrathecal opioids for intractable pain syndromes. Acta Neurochir Suppl. 97(Pt 1):43–8. DOI: 10.1007/978-3-211-33079-1_5. PMID: 17691355. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85052610124&origin=inward.
Article53. Kim WS, Kim KH. 2021; Percutaneous osteoplasty for painful bony lesions: a technical survey. Korean J Pain. 34:375–93. DOI: 10.3344/kjp.2021.34.4.375. PMID: 34593656. PMCID: PMC8494954. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85117890984&origin=inward.
Article54. Lipton A, Uzzo R, Amato RJ, Ellis GK, Hakimian B, Roodman GD, et al. 2009; The science and practice of bone health in oncology: managing bone loss and metastasis in patients with solid tumors. J Natl Compr Canc Netw. 7(Suppl 7):S1–29. DOI: 10.6004/jnccn.2009.0080. PMID: 19878635. PMCID: PMC3047391. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=71949095197&origin=inward.
Article55. Yang S, Park DH, Ahn SH, Kim J, Lee JW, Han JY, et al. 2017; Prevalence and risk factors of adhesive capsulitis of the shoulder after breast cancer treatment. Support Care Cancer. 25:1317–22. DOI: 10.1007/s00520-016-3532-4. PMID: 27942856. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85003794421&origin=inward.
Article56. Del Fabbro E. 2014; Assessment and management of chemical coping in patients with cancer. J Clin Oncol. 32:1734–8. DOI: 10.1200/JCO.2013.52.5170. PMID: 24799476. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84905744075&origin=inward.
Article57. Pergolizzi JV Jr, Magnusson P, Christo PJ, LeQuang JA, Breve F, Mitchell K, et al. 2021; Opioid therapy in cancer patients and survivors at risk of addiction, misuse or complex dependency. Front Pain Res (Lausanne). 2:691720. DOI: 10.3389/fpain.2021.691720. PMID: 35295520. PMCID: PMC8915703. PMID: d8aa530fb1c442bfb61e322a5a85994a.
Article58. Goodlev ER, Discala S, Darnall BD, Hanson M, Petok A, Silverman M. 2019; Managing cancer pain, monitoring for cancer recurrence, and mitigating risk of opioid use disorders: a team-based, interdisciplinary approach to cancer survivorship. J Palliat Med. 22:1308–17. DOI: 10.1089/jpm.2019.0171. PMID: 31329500. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85074308055&origin=inward.
Article59. Trescot AM, Helm S, Hansen H, Benyamin R, Glaser SE, Adlaka R, et al. 2008; Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians' (ASIPP) Guidelines. Pain Physician. 11(2 Suppl):S5–62. DOI: 10.36076/ppj.2008/11/S5. PMID: 18443640.60. Drug Enforcement Administration, US Department of Justice. 2020. US Department of Justice. Drugs of abuse. A DEA resource guide: 2020 ed. [Internet]. DEA;Springfield (VA): Available at: https://www.dea.gov/sites/default/files/2020-04/Drugs%20of%20Abuse%202020-Web%20Version-508%20compliant-4-24-20_0.pdf.61. Pagel JF, Parnes BL. 2001; Medications for the treatment of sleep disorders: an overview. Prim Care Companion J Clin Psychiatry. 3:118–25. DOI: 10.4088/PCC.v03n0303. PMID: 15014609. PMCID: PMC181172. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=20344372479&origin=inward.62. Busse JW, Craigie S, Juurlink DN, Buckley DN, Wang L, Couban RJ, et al. 2017; Guideline for opioid therapy and chronic noncancer pain. CMAJ. 189:E659–66. DOI: 10.1503/cmaj.170363. PMID: 28483845. PMCID: PMC5422149. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85019153936&origin=inward.
Article63. Barker C, Taylor A, Johnson M. 2014; Problematic pain - redefining how we view pain? Br J Pain. 8:9–15. DOI: 10.1177/2049463713512618. PMID: 26516529. PMCID: PMC4590175. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85006215397&origin=inward.
Article64. Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. 2009; Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 10:113–30. DOI: 10.1016/j.jpain.2008.10.008. PMID: 19187889. PMCID: PMC4043401. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=58949087497&origin=inward.
Article65. 2020; The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med. 14(2S Suppl 1):1–91. Erratum in: J Addict Med 2020; 14: 267. DOI: 10.1097/ADM.0000000000000633. PMID: 32511106. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85086297536&origin=inward.66. Crotty K, Freedman KI, Kampman KM. 2020; Executive summary of the focused update of the ASAM national practice guideline for the treatment of opioid use disorder. J Addict Med. 14:99–112. Erratum in: J Addict Med 2020; 14: 267. DOI: 10.1097/ADM.0000000000000635. PMID: 32209915. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85082380852&origin=inward.
Article67. US Food and Drug Administration. 2016. FDA Drug Safety Communications: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning [Internet]. US Food and Drug Administration;Silver Spring (MD): Available at: http://www.fda.gov/media/99761/download.68. National Institute on Drug Abuse (NIDA). 2016. Medications to treat opioid use disorder research report: how much does opioid treatment cost? [Internet]. NIDA;Gaithersburg (MD): Available at: https://nida.nih.gov/publications/research-reports/medications-to-treat-opioid-addiction/how-much-does-opioid-treatment-cost.69. Substance Abuse and Mental Health Services Administration (SAMHSA). 2015. Federal guidelines for opioid treatment programs [Internet]. SAMHSA;Rockville (MD): Available at: https://store.samhsa.gov/sites/default/files/d7/priv/pep15-fedguideotp.pdf.70. Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE. 2000; A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. N Engl J Med. 343:1290–7. DOI: 10.1056/NEJM200011023431802. PMID: 11058673. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0034597736&origin=inward.
Article71. Cheattle MD. 2019. Risk assessment: safe opioid prescribing tools [Internet]. Practical Pain Management;New York (NY): Available at: https://www.practicalpainmanagement.com/resource-centers/opioid-prescribing-monitoring/risk-assessment-safe-opioid-prescribing-tools.72. Webster LR, Webster RM. 2005; Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 6:432–42. DOI: 10.1111/j.1526-4637.2005.00072.x. PMID: 16336480. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=30944460282&origin=inward.
Article73. Butler SF, Fernandez K, Benoit C, Budman SH, Jamison RN. 2008; Validation of the revised Screener and Opioid Assessment for Patients with Pain (SOAPP-R). J Pain. 9:360–72. DOI: 10.1016/j.jpain.2007.11.014. PMID: 18203666. PMCID: PMC2359825. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=40949118164&origin=inward.
Article74. Coambs RE, Jarry JL, Santhiapillai AC, Abrahamsohn RV, Atance CM. 1996; The SISAP: a new screening instrument for identifying potential opioid abusers in the management of chronic nonmalignant pain within general medical practice. Pain Res Manag. 1:155–62. DOI: 10.1155/1996/391248. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0041324481&origin=inward.
Article75. Belgrade MJ, Schamber CD, Lindgren BR. 2006; The DIRE score: predicting outcomes of opioid prescribing for chronic pain. J Pain. 7:671–81. DOI: 10.1016/j.jpain.2006.03.001. PMID: 16942953. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=33747892369&origin=inward.
Article76. Compton PA, Wu SM, Schieffer B, Pham Q, Naliboff BD. 2008; Introduction of a self-report version of the Prescription Drug Use Questionnaire and relationship to medication agreement noncompliance. J Pain Symptom Manage. 36:383–95. DOI: 10.1016/j.jpainsymman.2007.11.006. PMID: 18508231. PMCID: PMC2630195. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=52149083219&origin=inward.
Article77. Butler SF, Budman SH, Fernandez KC, Houle B, Benoit C, Katz N, et al. 2007; Development and validation of the Current Opioid Misuse Measure. Pain. 130:144–56. Erratum in: Pain 2009; 142: 169. DOI: 10.1016/j.pain.2008.12.020. PMID: 17493754. PMCID: PMC1950245. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=60149109841&origin=inward.
Article78. Adams LL, Gatchel RJ, Robinson RC, Polatin P, Gajraj N, Deschner M, et al. 2004; Development of a self-report screening instrument for assessing potential opioid medication misuse in chronic pain patients. J Pain Symptom Manage. 27:440–59. DOI: 10.1016/j.jpainsymman.2003.10.009. PMID: 15120773. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=2342642074&origin=inward.
Article79. Compton P, Darakjian J, Miotto K. 1998; Screening for addiction in patients with chronic pain and "problematic" substance use: evaluation of a pilot assessment tool. J Pain Symptom Manage. 16:355–63. DOI: 10.1016/S0885-3924(98)00110-9. PMID: 9879160. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0032415875&origin=inward.80. Passik SD, Kirsh KL, Whitcomb L, Schein JR, Kaplan MA, Dodd SL, et al. 2005; Monitoring outcomes during long-term opioid therapy for noncancer pain: results with the Pain Assessment and Documentation Tool. J Opioid Manag. 1:257–66. DOI: 10.5055/jom.2005.0055. PMID: 17319559. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=33644766967&origin=inward.
Article81. Wu SM, Compton P, Bolus R, Schieffer B, Pham Q, Baria A, et al. 2006; The addiction behaviors checklist: validation of a new clinician-based measure of inappropriate opioid use in chronic pain. J Pain Symptom Manage. 32:342–51. DOI: 10.1016/j.jpainsymman.2006.05.010. PMID: 17000351. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=33748933250&origin=inward.
Article82. Brown RL, Rounds LA. 1995; Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 94:135–40. PMID: 7778330. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0028939436&origin=inward.83. Substance Abuse and Mental Health Services Administration (SAMHSA). 2022. Screening, brief intervention, and referral to treatment (SBIRT) [Internet]. Available at: http://www.samhsa.gov/sbirt.84. Bastiaens L, Riccardi K, Sakhrani D. 2002; The RAFFT as a screening tool for adult substance use disorders. Am J Drug Alcohol Abuse. 28:681–91. DOI: 10.1081/ADA-120015876. PMID: 12492264. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0036447513&origin=inward.
Article85. Skinner HA. 1982; The drug abuse screening test. Addict Behav. 7:363–71. DOI: 10.1016/0306-4603(82)90005-3. PMID: 7183189. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0020446368&origin=inward.
Article86. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. 1998; The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 158:1789–95. DOI: 10.1001/archinte.158.16.1789. PMID: 9738608. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0032517042&origin=inward.
Article87. Berman AH, Palmstierna T, Källmén H, Bergman H. 2007; The self-report Drug Use Disorders Identification Test: Extended (DUDIT-E): reliability, validity, and motivational index. J Subst Abuse Treat. 32:357–69. DOI: 10.1016/j.jsat.2006.10.001. PMID: 17481459. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=34247504522&origin=inward.88. Wakeman SE. 2020; Diagnosis and treatment of opioid use disorder in 2020. JAMA. 323:2082–3. DOI: 10.1001/jama.2020.4104. PMID: 32329798. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85084071419&origin=inward.
Article89. US Food and Drug Administration. 2019. Information about medication-assisted treatment (MAT) [Internet]. US Food and Drug Administration;Silver Spring (MD): Available at: https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat.90. Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. 2017; Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 357:j1550. DOI: 10.1136/bmj.j1550. PMID: 28446428. PMCID: PMC5421454. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85019393374&origin=inward.
Article91. Whelan PJ, Remski K. 2012; Buprenorphine vs methadone treatment: a review of evidence in both developed and developing worlds. J Neurosci Rural Pract. 3:45–50. DOI: 10.4103/0976-3147.91934. PMID: 22346191. PMCID: PMC3271614. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84856386075&origin=inward.
Article92. Oakley B, Wilson H, Hayes V, Lintzeris N. 2021; Managing opioid withdrawal precipitated by buprenorphine with buprenorphine. Drug Alcohol Rev. 40:567–71. DOI: 10.1111/dar.13228. PMID: 33480051. PMCID: PMC8248003. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85100179642&origin=inward.
Article93. Connery HS. 2015; Medication-assisted treatment of opioid use disorder: review of the evidence and future directions. Harv Rev Psychiatry. 23:63–75. DOI: 10.1097/HRP.0000000000000075. PMID: 25747920. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84925357081&origin=inward.94. Patterson Silver Wolf DA, Gold M. 2020; Treatment resistant opioid use disorder (TROUD): definition, rationale, and recommendations. J Neurol Sci. 411:116718. DOI: 10.1016/j.jns.2020.116718. PMID: 32078842. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85079552677&origin=inward.95. Substance Abuse and Mental Health Services Administration (SAMHSA). 2010. Protracted withdrawal. Substance abuse treatment advisory. News for the treatment field. 2010; 9: 1-8. US Department of Health and Human Services. Substance Abuse and Mental Health Services Administration (SAMHSA). HHS Publication No. (SMA) 10-4554 [Internet]. SAMHSA;Rockville (MD): https://store.samhsa.gov/sites/default/files/d7/priv/sma10-4554.pdf.96. Nicholson SC, Peterson J, Yektashenas B. 2012; Risk evaluation and mitigation strategies (REMS): educating the prescriber. Drug Saf. 35:91–104. DOI: 10.2165/11597840-000000000-00000. PMID: 22171604. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84855823712&origin=inward.97. Korea Institute of Drug Safety and Risk Management. 2012. Introduction of DUR [Internet]. Korea Institute of Drug Safety and Risk Management;Anyang: Available at: https://www.drugsafe.or.kr/iwt/ds/en/useinfo/EgovIntroductionDur.do;jsessionid=53QMnC26k99DG3u2FY638AOG8BogWIuUVYkBEqwtKqklSoVgUOBjwLqbWlZlxoH4.webint_2_servlet_engine1.98. Korea Institute of Drug Safety and Risk Management. 2015. Introduction of narcotics handling report system (NHRS) [Internet]. Korea Institute of Drug Safety and Risk Management;Anyang: Available at: https://www.drugsafe.or.kr/iwt/ds/en/introduction/HandlingReporting.do;jsessionid=ZNaCx119JkUJTu1c62TzYUJudPH4D1aeUucLyaaU6cjG1geHyEWfRC0yuF0lD171.webint_2_servlet_engine1.99. Health Insurance Review and Assessment Service. 2020. Drug utilization review (DUR) [Internet]. Health Insurance Review and Assessment Service;Wonju: Available at: https://www.hira.or.kr/eng/about/05/01/04/index.html.100. Baldini A, Von Korff M, Lin EH. 2012; A review of potential adverse effects of long-term opioid therapy: a practitioner's guide. Prim Care Companion CNS Disord. 14:PCC. DOI: 10.4088/PCC.11m01326. PMID: 23106029. PMCID: PMC3466038. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84864724424&origin=inward.101. Petzke F, Bock F, Hüppe M, Nothacker M, Norda H, Radbruch L, et al. 2020; Long-term opioid therapy for chronic noncancer pain: second update of the German guidelines. Pain Rep. 5:e840. DOI: 10.1097/PR9.0000000000000840. PMID: 32904018. PMCID: PMC7447355. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85105915220&origin=inward.
Article102. Ford C, Barnard J, Bury J, Carnwath T, Gerada C, Joyce A, et al. 2005. Royal College of General Practitioners: guidance for the use of methadone for the treatment of opioid dependence in primary care [Internet]. Royal College of General Practitioners;London: Available at: https://www.drugsandalcohol.ie/13635/1/RCGP_meth_guidance.pdf.103. Sofuoglu M, DeVito EE, Carroll KM. 2019; Pharmacological and behavioral treatment of opioid use disorder. Psychiatr Res Clin Pract. 1:4–15. DOI: 10.1176/appi.prcp.20180006. PMCID: PMC9175946.
Article104. Reddy S, Hui D, El Osta B, de la Cruz M, Walker P, Palmer JL, et al. 2010; The effect of oral methadone on the QTc interval in advanced cancer patients: a prospective pilot study. J Palliat Med. 13:33–8. DOI: 10.1089/jpm.2009.0184. PMID: 19824814. PMCID: PMC2939847. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=74549168886&origin=inward.
Article105. Khanna IK, Pillarisetti S. 2015; Buprenorphine - an attractive opioid with underutilized potential in treatment of chronic pain. J Pain Res. 8:859–70. DOI: 10.2147/JPR.S85951. PMID: 26672499. PMCID: PMC4675640. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84949811193&origin=inward.106. Fischer A, Jönsson M, Hjelmström P. 2015; Pharmaceutical and pharmacokinetic characterization of a novel sublingual buprenorphine/naloxone tablet formulation in healthy volunteers. Drug Dev Ind Pharm. 41:79–84. DOI: 10.3109/03639045.2013.846365. PMID: 24099551. PMCID: PMC4364559. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=84918832438&origin=inward.
Article107. Substance Abuse and Mental Health Services Administration (SAMHSA). 2022. Medication-assisted treatment (MAT): MAT medications, counseling, and related conditions - naltrexone [Internet]. SAMHSA;Rockville (MD): Available at: https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/naltrexone.108. Kunzler NM, Wightman RS, Nelson LS. 2020; Opioid withdrawal precipitated by long-acting antagonists. J Emerg Med. 58:245–53. DOI: 10.1016/j.jemermed.2019.12.015. PMID: 32005608. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85078430627&origin=inward.
Article109. Wesson DR, Ling W. 2003; The clinical opiate withdrawal scale (COWS). J Psychoactive Drugs. 35:253–9. DOI: 10.1080/02791072.2003.10400007. PMID: 12924748. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=0041665111&origin=inward.
Article110. Kim J, Shin SJ, Yoon J, Kim HS, Lee JW, Kim YS, et al. 2022; Recent trends in opioid prescriptions in Korea from 2002 to 2015 based on the Korean NHIS-NSC cohort. Epidemiol Health. 44:e2022029. DOI: 10.4178/epih.e2022029. PMID: 35209705. PMCID: PMC9117092. PMID: 1c140eab304b41bfa1e15ab7abce5976. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85130767708&origin=inward.
Article111. Oh TK, Jeon YT, Choi JW. 2019; Trends in chronic opioid use and association with five-year survival in South Korea: a population-based cohort study. Br J Anaesth. 123:655–63. DOI: 10.1016/j.bja.2019.08.012. PMID: 31558315. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85072384311&origin=inward.
Article112. Cho NR, Chang YJ, Lee D, Kim JR, Ko DS, Choi JJ. 2021; Trends in opioid prescribing practices in South Korea, 2009-2019: are we safe from an opioid epidemic? PLoS One. 16:e0250972. DOI: 10.1371/journal.pone.0250972. PMID: 33979378. PMCID: PMC8115784. PMID: 69d86f514f0541bfa44b009bf800f6cc. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85105620114&origin=inward.
Article113. Noh Y, Heo KN, Yu YM, Lee JY, Ah YM. 2022; Trends in potentially inappropriate opioid prescribing and associated risk factors among Korean noncancer patients prescribed non-injectable opioid analgesics. Ther Adv Drug Saf. 13:20420986221091001. DOI: 10.1177/20420986221091001. PMID: 35509350. PMCID: PMC9058459. PMID: aed801643d0542f6bae43e5435f1a1b2. PMID: https://www.scopus.com/inward/record.uri?partnerID=HzOxMe3b&scp=85129202683&origin=inward.
Article114. The Korea Orphan and Essential Drug Center (KOEDC). 2021. Example of request for supply of narcotic drugs [Internet]. KOEDC;Seoul: Available at: https://www.kodc.or.kr/cntnts/219.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Opioid-induced Muscle Rigidity with a Delayed Manifestation Misunderstood as a Tension Pneumothorax: A case report
- Visual and Auditory Reaction Times of Patients with Opioid Use Disorder
- Successful Treatment with Transdermal Buprenorphine Patch in Opioid-Dependent Cancer Patients: Case Series
- Effects of Opioid Agonists on the Suppressed Spontaneous Alternation Behaviour in Rats
- Opioid pharmacogenetics in anesthesia and pain management