Pediatr Emerg Med J.
2022 Jun;9(1):35-40. 10.22470/pemj.2022.00465.
Changes in pediatric psychiatric emergency during the coronavirus disease 2019 pandemic
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- 2Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2531527
- DOI: http://doi.org/10.22470/pemj.2022.00465
Abstract
- Purpose
The lifestyle changes during the coronavirus disease 2019 pandemic possibly affected mental health among the pediatric population. We aimed to analyze changes in psychiatric emergency-related visits to the emergency department (ED).
Methods
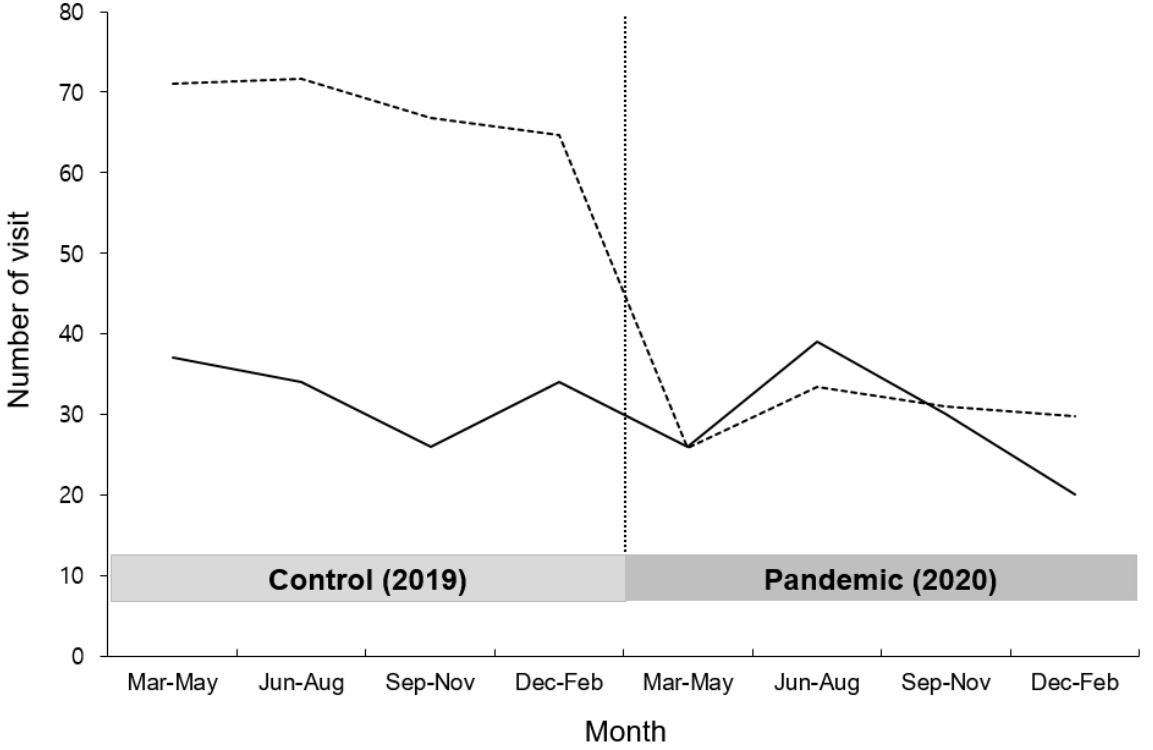
We reviewed cases of pediatric patients (≤ 18 years) who visited the ED of a tertiary hospital with psychiatric emergency as a chief complaint from March 2019 through February 2021. The study period was dichotomized by March 2020, starting point of social distancing, into the pandemic and control periods. Clinical data were collected and compared between the 2 periods.
Results
A total of 246 cases with a mean age of 15.2 years were included. The overall visits to the ED decreased to 43.8% whereas the proportion of psychiatric emergency-related visits increased during the pandemic period, compared to the control period (0.5% vs. 1.0%; P < 0.001). The cases with suicidality, including ideation and attempt, increased in both number and proportion during the pandemic period (51 [38.9%] vs. 63 [54.8%]; P = 0.013).
Conclusion
Pediatric psychiatric emergency-related visits, particularly suicidality, proportionally increased during the pandemic. This finding may be useful to prepare psychiatric resources in EDs.
Keyword
Figure
Cited by 1 articles
-
Impact of coronavirus disease 2019 pandemic on pediatric poisoning in a single emergency department in Korea
Jae-Uk Shin, Sae Jeung Kwak, Sung Hyun Yun
Pediatr Emerg Med J. 2023;10(3):87-93. doi: 10.22470/pemj.2022.00647.
Reference
-
References
1. Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:699–704.
Article2. Dopfer C, Wetzke M, Zychlinsky Scharff A, Mueller F, Dressler F, Baumann U, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - a concerning trend. BMC Pediatr. 2020; 20:427.
Article3. Kruizinga MD, Peeters D, van Veen M, van Houten M, Wieringa J, Noordzij JG, et al. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur J Pediatr. 2021; 180:2271–9.
Article4. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul Metropolitan Area, Korea. J Korean Med Sci. 2021; 36:e44.
Article5. Hwang SY, Lee JK, Ryu HS, Park SS, Choi JY, Lee HJ, et al. Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea. Pediatr Emerg Med J. 2021; 8:57–65. Korean.
Article6. Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021; 147:e2020029280.
Article7. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020; 4:421.
Article8. Ministry of Health and Wellfare, Korean Disease Control and Prevetional Agency. >Card News: COVID-19 infectious disease crisis alert “serious” issued; kindergarten, elementary, middle, and high school start of new semester postponed. Central Disaster Management Headquarter’s regular briefing [Internet]. Sejong (Korea): Ministry of Health and Wellfare;c2022 [cited 2022 May 6]. Available from: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=605&contSeq=605&board_id=311&gubun=ALL. Korean.9. Krass P, Dalton E, Doupnik SK, Esposito J. US Pediatric Emergency Department Visits for Mental Health Conditions During the COVID-19 Pandemic. JAMA Netw Open. 2021; 4:e218533.
Article10. Leff RA, Setzer E, Cicero MX, Auerbach M. Changes in pediatric emergency department visits for mental health during the COVID-19 pandemic: a cross-sectional study. Clin Child Psychol Psychiatry. 2021; 26:33–8.
Article11. Fernandez A, Gindt M, Babe P, Askenazy F. Mental health-related visits in a pediatric emergency department during the COVID-19 pandemic. Int J Emerg Med. 2021; 14:64.
Article12. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395:912–20.
Article13. Orben A, Tomova L, Blakemore SJ. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. 2020; 4:634–40.
Article14. Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021; 175:1142–50.
Article15. Kim SY, Kim HR, Park B, Choi HG. Comparison of stress and suicide-related behaviors among Korean youths before and during the COVID-19 pandemic. JAMA Netw Open. 2021; 4:e2136137.
Article16. Lewitzka U, Spirling S, Ritter D, Smolka M, Goodday S, Bauer M, et al. Suicidal ideation vs. suicide attempts: clinical and psychosocial profile differences among depressed patients: a study on personality traits, psychopathological variables, and sociodemographic factors in 228 patients. J Nerv Ment Dis. 2017; 205:361–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- State and Improvement Policy of Psychiatric Emergency during COVID-19 Pandemic
- A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic
- Changes in pediatric injury-related visits during coronavirus disease 2019 pandemic at a single regional emergency medical center in Korea
- Impact of coronavirus disease 2019 pandemic on pediatric poisoning in a single emergency department in Korea
- Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea