Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea
- Affiliations
-
- 1Department of Emergency Medicine, Konyang University Hospital, Daejeon, Korea
- KMID: 2523996
- DOI: http://doi.org/10.22470/pemj.2021.00346
Abstract
- Purpose
As coronavirus disease 2019 pandemic has been prolonged, it became crucial to analyze the long-term impact of the pandemic on emergency department (ED) utilization for efficient use of emergency medicine resources.
Methods
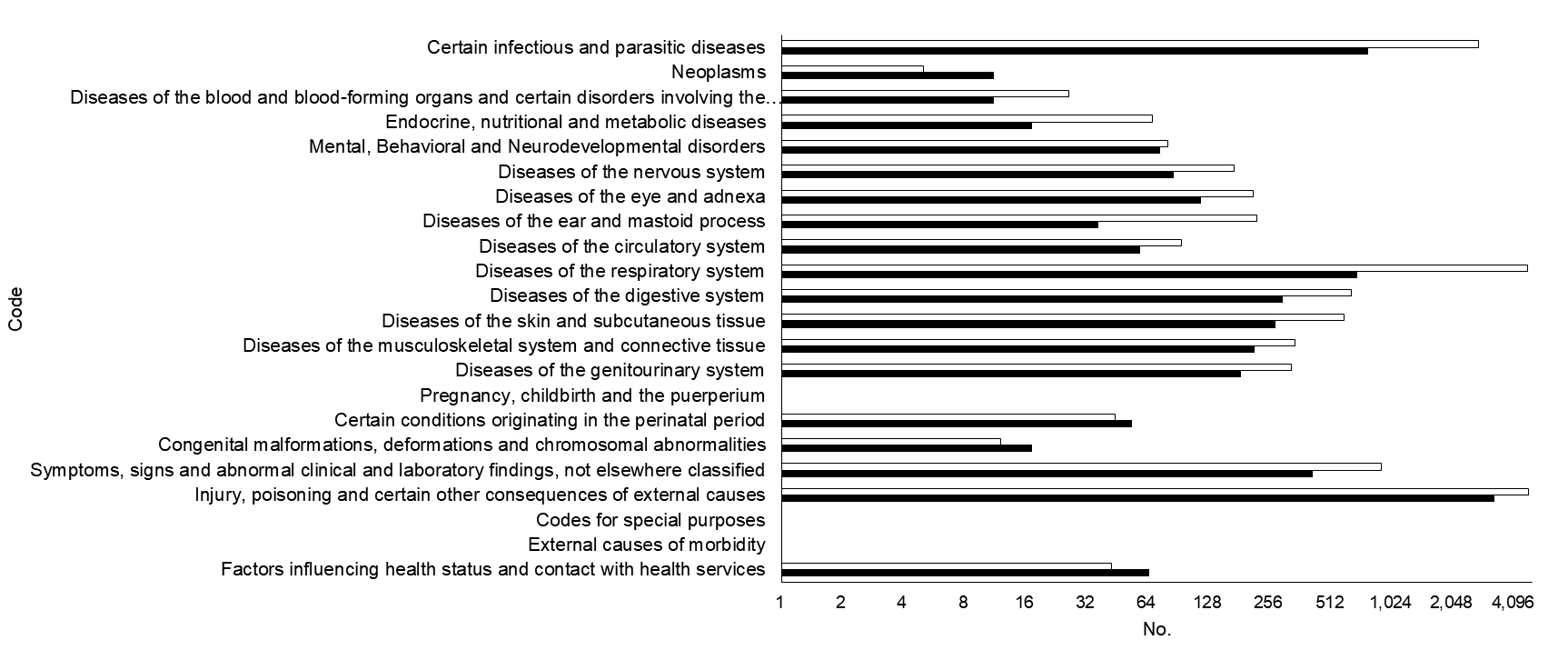
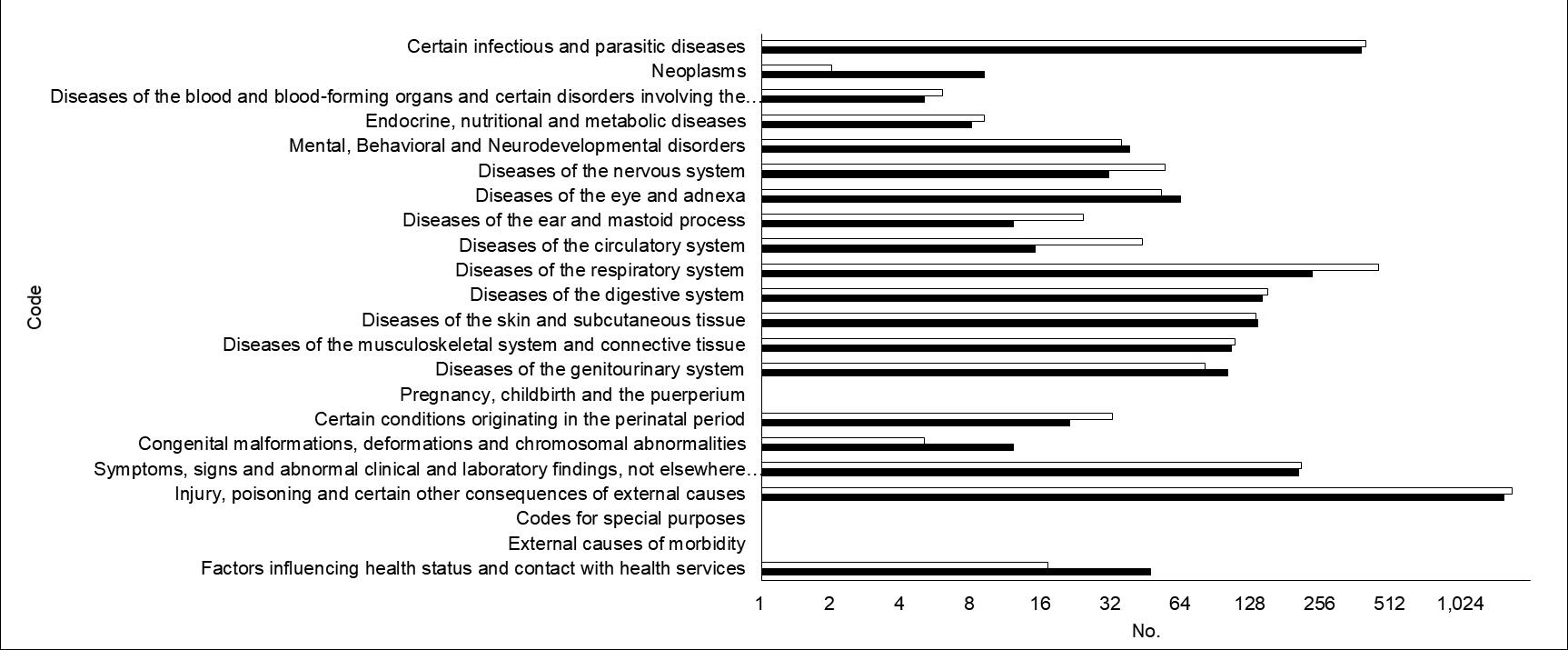
We reviewed the data of children (≤ 18 years) who visited the ED in Daejeon, Korea, from February 2019 through January 2021. This period was dichotomized by February 2020 into the reference and pandemic periods. The latter period was further divided into the early (February-August 2020) and late pandemic periods. Between the reference and pandemic periods, and between the early and late pandemic periods, we respectively compared proportions of children in all patients (including adults), age groups, high acuity (the Korean Triage and Acuity Scale 1-2), diagnostic codes, visits via ambulances, ED length of stay, and ED disposition.
Results
Compared to the reference and early pandemic periods, the pandemic and late pandemic periods respectively showed changes as follows: proportion of children in all patients (from 29.8% to 19.0% and from 19.8% to 18.1%; all Ps < 0.001), children younger than 5 years (from 56.7% to 49.9% and from 52.1% to 47.4%; all Ps < 0.001), high acuity (from 12.0% to 7.8% [P < 0.001] and from 8.8% to 6.7% [P = 0.004]), “Injury, poisoning and certain other consequences of external causes (S00-T98; from 30.0% to 49.0% and from 48.3% to 49.8%),” and “Diseases of the respiratory system (J00-J99; from 29.6% to 10.3% and from 12.8% to 7.5%).” Increases in the visits via ambulances, ED length of stay, children undergoing intensive care unit hospitalization or death were noted only in comparison between the reference and pandemic periods.
Conclusion
A long-term impact of the pandemic on ED use may be a decrease in the proportion of young or ill children.
Keyword
Figure
Cited by 4 articles
-
Effect of coronavirus disease 2019 pandemic on children’s visits to the emergency department
Hong Min Kim, Sang Ook Ha, Won Seok Yang, Young Sun Park, Jin Hyouk Kim
Pediatr Emerg Med J. 2022;9(1):10-16. doi: 10.22470/pemj.2021.00381.Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department
Dae Ho Kang
Pediatr Emerg Med J. 2022;9(1):29-34. doi: 10.22470/pemj.2022.00451.Changes in pediatric psychiatric emergency during the coronavirus disease 2019 pandemic
Jung Il Kwak, Jun Sung Park, Seung Jun Choi, Jong Seung Lee, Jeong-Min Ryu, Jeong-Yong Lee
Pediatr Emerg Med J. 2022;9(1):35-40. doi: 10.22470/pemj.2022.00465.Changes in emergency department utilization by neonates during the coronavirus disease 2019 pandemic: a single-center study in Korea
Sung Hee Lee, Shin Won Yoon, Ju Hyun Jin
Pediatr Emerg Med J. 2024;11(3):107-114. doi: 10.22470/pemj.2024.00976.
Reference
-
References
1. Heiber M, Lou WY. Effect of the SARS outbreak on visits to a community hospital emergency department. CJEM. 2006; 8:323–8.
Article2. Lee SY, Khang YH, Lim HK. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019; 60:796–803.
Article3. Dopfer C, Wetzke M, Zychlinsky Scharff A, Mueller F, Dressler F, Baumann U, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - a concerning trend. BMC Pediatr. 2020; 20:427.
Article4. Kruizinga MD, Peeters D, van Veen M, van Houten M, Wieringa J, Noordzij JG, et al. The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur J Pediatr. 2021; 180:2271–9.
Article5. Li H, Yu G, Duan H, Fu J, Shu Q. Changes in children’s healthcare visits during coronavirus disease-2019 pandemic in Hangzhou, China. J Pediatr. 2020; 224:146–9.
Article6. Korea Disease Control and Prevention Agency. Current status of COVID-19 outbreak in Korea [Internet]. Cheongju (Korea): Korea Disease Control and Prevention Agency;2020 [cited 2021 Aug 19]. Available from: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=4541&contSeq=4541&board_id=312&gubun=ALL. Korean.7. National Medical Center. 2019 Emergency medical statistical year book [Internet]. Seoul (Korea): National Medical Center;2020 [cited 2021 Aug 9]. Available from: https://www.nmc.or.kr/nmc/singl/convert/convertToHtml.do?viewType=CONTBODY&atchFileId=9f5929f6af304fe59cdf96f6d725e4f8&fileSn=1. Korean.8. Choi H, Ok JS, An SY. Evaluation of validity of the Korean Triage and Acuity Scale. J Korean Acad Nurs. 2019; 49:26–35. Korean.
Article9. Hwang Y, Jo HY, Yoo HW, Kim YM, Kim HY. Characteristics of children with trauma compared to those with disease in the emergency department: a Korean single regional emergency medical center study. Pediatr Emerg Med J. 2020; 7:108–13. Korean.
Article10. Lee KJ, Park MH, Suh J, Jung SY, Lee SJ, Cha M. Triage results of children who visited the emergency department via emergency medical service providers: an observational study in a regional emergency medical center. Pediatr Emerg Med J. 2017; 4:18–24. Korean.
Article11. Lim T, Park J, Je S. Pediatric Korean Triage and Acuity Scale. Pediatr Emerg Med J. 2015; 2:53–8. Korean.
Article12. Vital Statistics Division, Statistics Korea, Shin HY, Lee JY, Kim JE, Lee S, Youn H, et al. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018; 61:573–84.
Article13. Jang KM, Ahn JY, Choi HJ, Lee S, Kim D, Lee DW, et al. Pediatric emergency department utilization and coronavirus disease in Daegu, Korea. J Korean Med Sci. 2021; 36:e11.
Article14. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, Kwak YH, Kim DK. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul Metropolitan Area, Korea. J Korean Med Sci. 2021; 36:e44.
Article15. DeLaroche AM, Rodean J, Aronson PL, Fleegler EW, Florin TA, Goyal M, et al. Pediatric emergency department visits at US children's hospitals during the covid-19 pandemic. Pediatrics. 2021; 147:e2020039628.
Article16. Adjemian J, Hartnett KP, Kite-Powell A, DeVies J, Azondekon R, Radhakrishnan L, et al. Update: COVID-19 pandemic-associated changes in emergency department visits - United States, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021; 70:552–6.
Article17. Gaythorpe KA, Bhatia S, Mangal T, Unwin HJ, Imai N, Cuomo-Dannenburg G, et al. Children’s role in the COVID-19 pandemic: a systematic review of early surveillance data on susceptibility, severity, and transmissibility. Sci Rep. 2021; 11:13903.
Article18. Ministry of Health and Welfare. Public perception survey on social distancing [Internet]. Sejong (Korea): Ministry of Health and Welfare;2021 [cited 2021 May 12]. Available from: http://www.mohw.go.kr/react/modules/download.jsp?BOARD_ID=140&CONT_SEQ=363364&FILE_SEQ=312491. Korean.19. Hankook Research. [COVID-19] Situational awareness and government response evaluation [Internet]. Seoul (Korea): Hankook Research;2021 [cited 2021 May 12]. Available from: https://hrcopinion.co.kr/archives/17477. Korean.20. Lee T, Kwon HD, Lee J. The effect of control measures on COVID-19 transmission in South Korea. PLoS One. 2021; 16:e0249262.
Article21. Lee H, Lee H, Song KH, Kim ES, Park JS, Jung J, et al. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin Infect Dis. 2021; 73:e132–40.
Article22. Kim S, Ko Y, Kim YJ, Jung E. The impact of social distancing and public behavior changes on COVID-19 transmission dynamics in the Republic of Korea. PLoS One. 2020; 15:e0238684.
Article23. Jang WM, Jang DH, Lee JY. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 Middle East respiratory syndrome coronavirus outbreaks in Korea. J Korean Med Sci. 2020; 35:e220.
Article24. Kim JA, Son MH, Park M. Effect of coronavirus disease 2019 on febrile children’s visits to the emergency department of a tertiary hospital. Pediatr Emerg Med J. 2021; 8:8–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic
- The impacts of the COVID-19 pandemic on emergency care utilization in patients with major emergency diseases in Chungnam Province
- Impact of COVID-19 pandemic on emergency department visits during daytime and nighttime
- Changes in emergency department utilization by neonates during the coronavirus disease 2019 pandemic: a single-center study in Korea
- The proposed algorithm for emergency endoscopy during the coronavirus disease 2019 outbreak