Pediatr Emerg Med J.
2023 Jul;10(3):87-93. 10.22470/pemj.2022.00647.
Impact of coronavirus disease 2019 pandemic on pediatric poisoning in a single emergency department in Korea
- Affiliations
-
- 1Department of Emergency Medicine, Catholic Kwandong University International St. Mary’s Hospital, Incheon, Republic of Korea
- KMID: 2543575
- DOI: http://doi.org/10.22470/pemj.2022.00647
Abstract
- Purpose
This study was performed to investigate the coronavirus disease 2019 pandemic-related changes in epidemiological features of pediatric patients with poisoning who visited a local emergency medical center in Incheon, Korea.
Methods
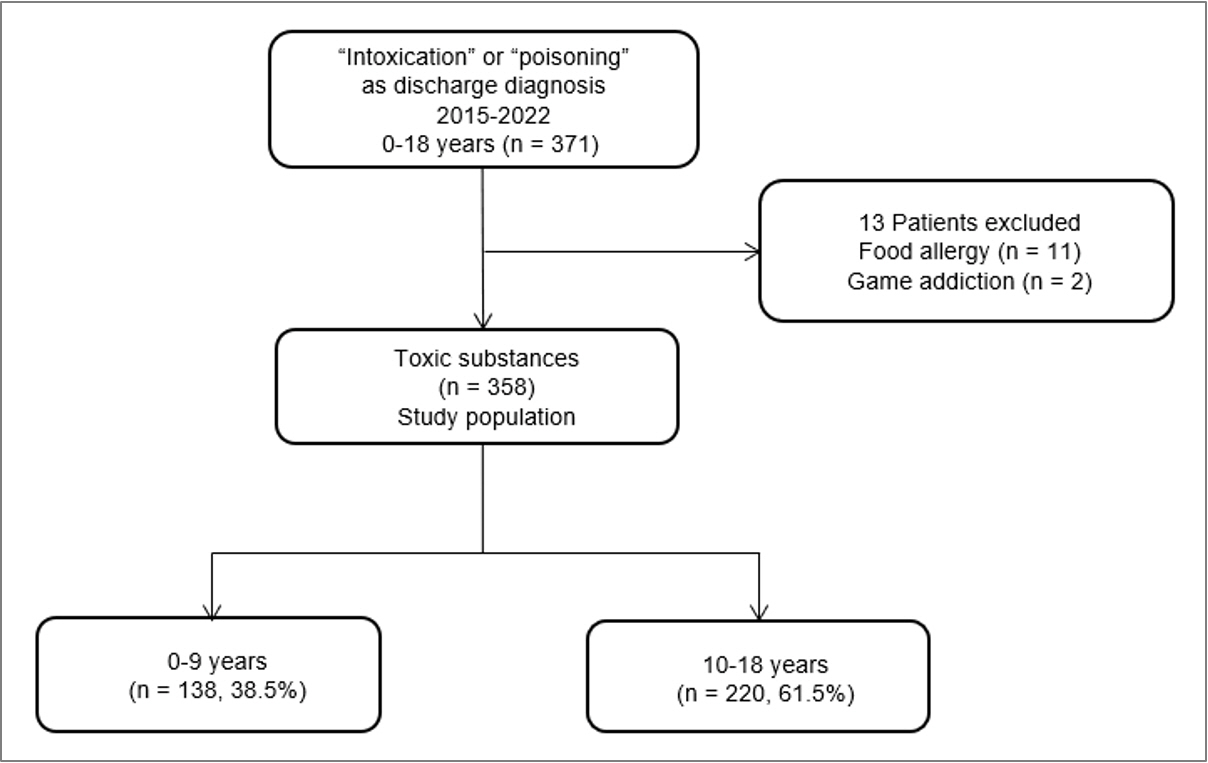
We reviewed medical records of the patients (aged ≤ 18 years) who visited the emergency department (ED) from 2015 through 2022 and obtained discharge diagnoses containing "intoxication" or "poisoning," excluding food allergy and game addiction. Time of visit was categorized as pre-pandemic (2015-2019) and pandemic (2020-2022) periods. They were investigated for age, age groups (children [0-9 years] vs. adolescents [10-18 years]), sex, visits during weekend or holiday, exposure-to-ED time, psychiatric history, intentionality, alcohol consumption, substances, therapeutic interventions, and outcomes. The outcomes included need for hospitalization and discharge against medical advice.
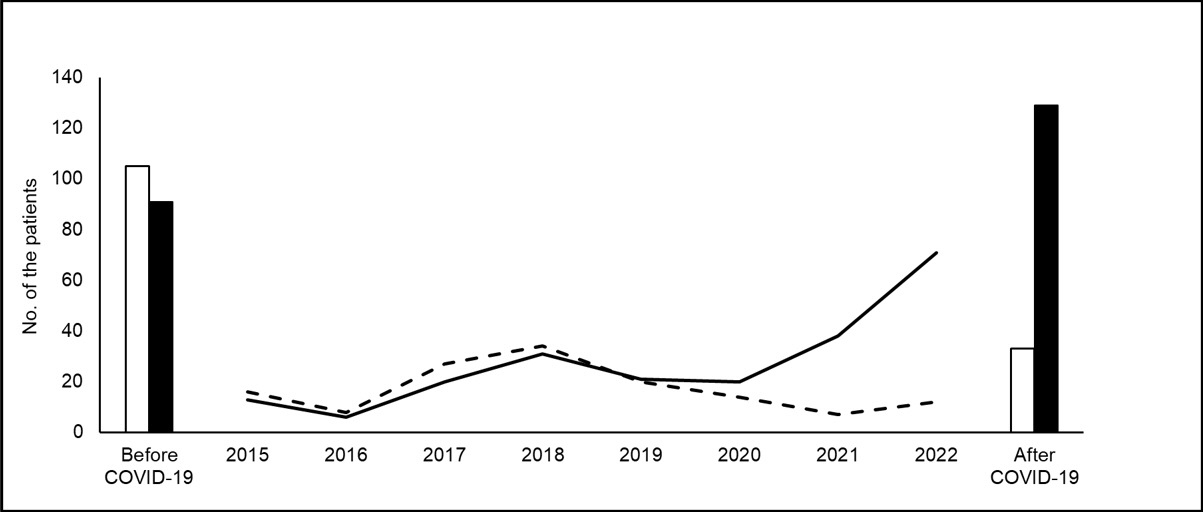
Results
Among a total of 358 patients with poisoning, 162 (45.3%) visited during the pandemic period, and 220 (61.5%) were adolescents. Compared to the patients who visited during the pre-pandemic period, those who visited during the pandemic period showed significantly higher frequencies of girls (45.9% vs. 81.5%), age of 10-18 years (46.4% vs. 79.6%), intentionality (33.7% vs. 74.7%), alcohol consumption (4.1% vs. 11.7%), need for hospitalization (24.5% vs. 62.3%), and discharge against medical advice (3.1% vs. 25.9%).
Conclusion
In the ED, pediatric poisoning became more intentional, female and adolescent-dominant, and severe in their outcomes during the pandemic.
Keyword
Figure
Reference
-
References
1. Lee J, Fan NC, Yao TC, Hsia SH, Lee EP, Huang JL, et al. Clinical spectrum of acute poisoning in children admitted to the pediatric emergency department. Pediatr Neonatol. 2019; 60:59–67.
Article2. Sahin S, Carman KB, Dinleyici EC. Acute poisoning in children; data of a pediatric emergency unit. Iran J Pediatr. 2011; 21:479–84.3. Gokalp G. Evaluation of poisoning cases admitted to pediatric emergency department. Int J Pediatr Adolesc Med. 2019; 6:109–14.
Article4. Korea Disease Control and Prevention Agency (KDCA). 2020 Injury types and cause statistics [Internet]. Cheongju (Korea): KDCA;c2019 [cited 2023 Jan 5]. Available from: https://www.kdca.go.kr/injury/biz/injury/recsroom/statsSmMain.do. Korean.5. Han CS, Jeon WC, Min YG, Choi SC, Lee JS. Retrospective analysis on the clinical differences of children and adolescents treated for acute pediatric poisoning in an emergency department? J Korean Soc Emerg Med. 2013; 24:742–9. Korean.6. Halhalli HC, Uslu T. Evaluation of pediatric patients admitted to the emergency department due to drug intoxication. Cureus. 2021; 13:e13366.
Article7. Tay EY, Tan GF, Yeo AWC, Tham EH. Intentional poisoning in pediatric patients: examining the risk factors. Pediatr Emerg Care. 2021; 1(37):e1510–4.8. Kwak JI, Park JS, Choi SJ, Lee JS, Ryu JM, Lee JY. Changes in pediatric psychiatric emergency during the coronavirus disease 2019 pandemic. Pediatr Emerg Med J. 2022; 9:35–40. Korean.
Article9. An YJ, Paek SH, Kim OJ, Kim JA, Kwon JH, Kim MJ. Gender differences in characteristics of adolescents with suicide attempt at the emergency department. Pediatr Emerg Med J. 2020; 7:120–6. Korean.
Article10. Gracia R, Pamias M, Mortier P, Alonso J, Pérez V, Palao D. Is the COVID-19 pandemic a risk factor for suicide attempts in adolescent girls? J Affect Disord. 2021; 292:139–41.
Article11. Warheit GJ, Zimmerman RS, Khoury EL, Vega WA, Gil AG. Disaster related stresses, depressive signs and symptoms, and suicidal ideation among a multi-racial/ethnic sample of adolescents: a longitudinal analysis. J Child Psychol Psychiatry. 1996; 37:435–44.
Article12. Garza K, Jovanovic T. Impact of gender on child and adolescent PTSD. Curr Psychiatry Rep. 2017; 19:87.
Article13. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020; 29:749–58.
Article14. Manouchehrifar M, Derakhshandeh N, Shojaee M, Sabzghabaei A, Farnaghi F. An epidemiologic study of pediatric poisoning; a six-month cross-sectional study. Emerg (Tehran). 2016; 4:21–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A potential impact of the donning and doffing policy on emergency department length of stay during the coronavirus disease 2019 pandemic
- Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea
- Changes in pediatric injury-related visits during coronavirus disease 2019 pandemic at a single regional emergency medical center in Korea
- Changes in the characteristics of acute carbon monoxide poisoning patients who visited the emergency department during the COVID-19 pandemic
- Characteristics of poisoning patients visiting emergency departments before and after the COVID-19 pandemic