Ann Hepatobiliary Pancreat Surg.
2022 May;26(2):159-167. 10.14701/ahbps.21-125.
Optimal timing of percutaneous transhepatic gallbladder drainage and subsequent laparoscopic cholecystectomy according to the severity of acute cholecystitis
- Affiliations
-
- 1Department of Surgery, Konyang University Hospital, Konyang University College of Medicine, Daejeon, Korea
- KMID: 2530095
- DOI: http://doi.org/10.14701/ahbps.21-125
Abstract
- Backgrounds/Aims
The optimal timing of percutaneous transhepatic gallbladder drainage (PTGBD) and subsequent laparoscopic cholecystectomy (LC) according to the severity of acute cholecystitis (AC) has not been established yet.
Methods
This single-center, retrospective study included 695 patients with grade I or II AC without common bile duct stones who underwent PTGBD and subsequent LC between January 2010 and December 2019. Difficult surgery (DS) (open conversion, subtotal cholecystectomy, adjacent organ injury, transfusion, operation time ≥ 90 minutes, or estimated blood loss ≥ 100 mL) and poor postoperative outcome (PPO) (postoperative hospital stay ≥ 7 days or Clavien-Dindo grade ≥ II postoperative complication) were defined to comprehensively evaluate intraoperative and postoperative outcomes, respectively.
Results
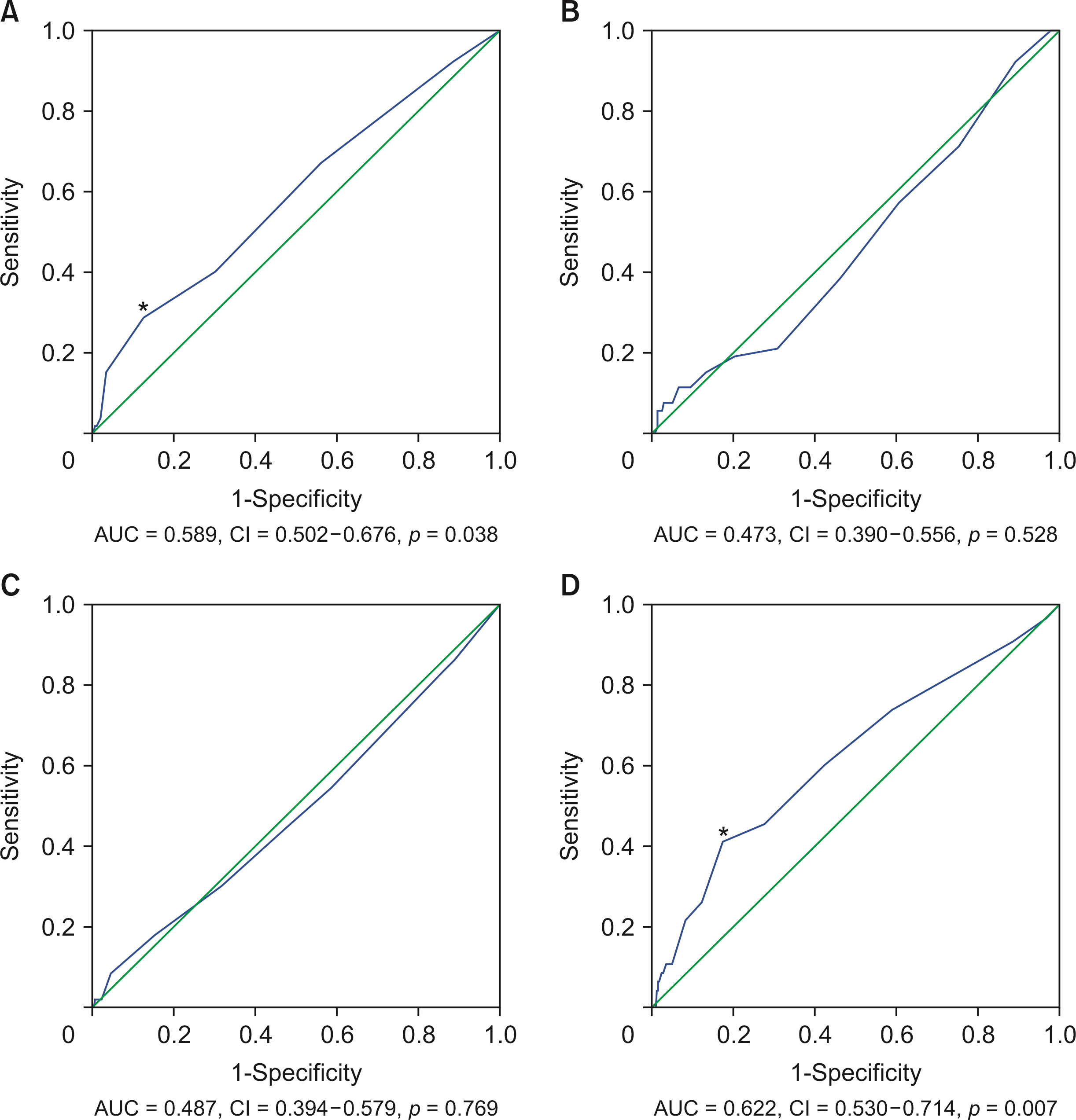
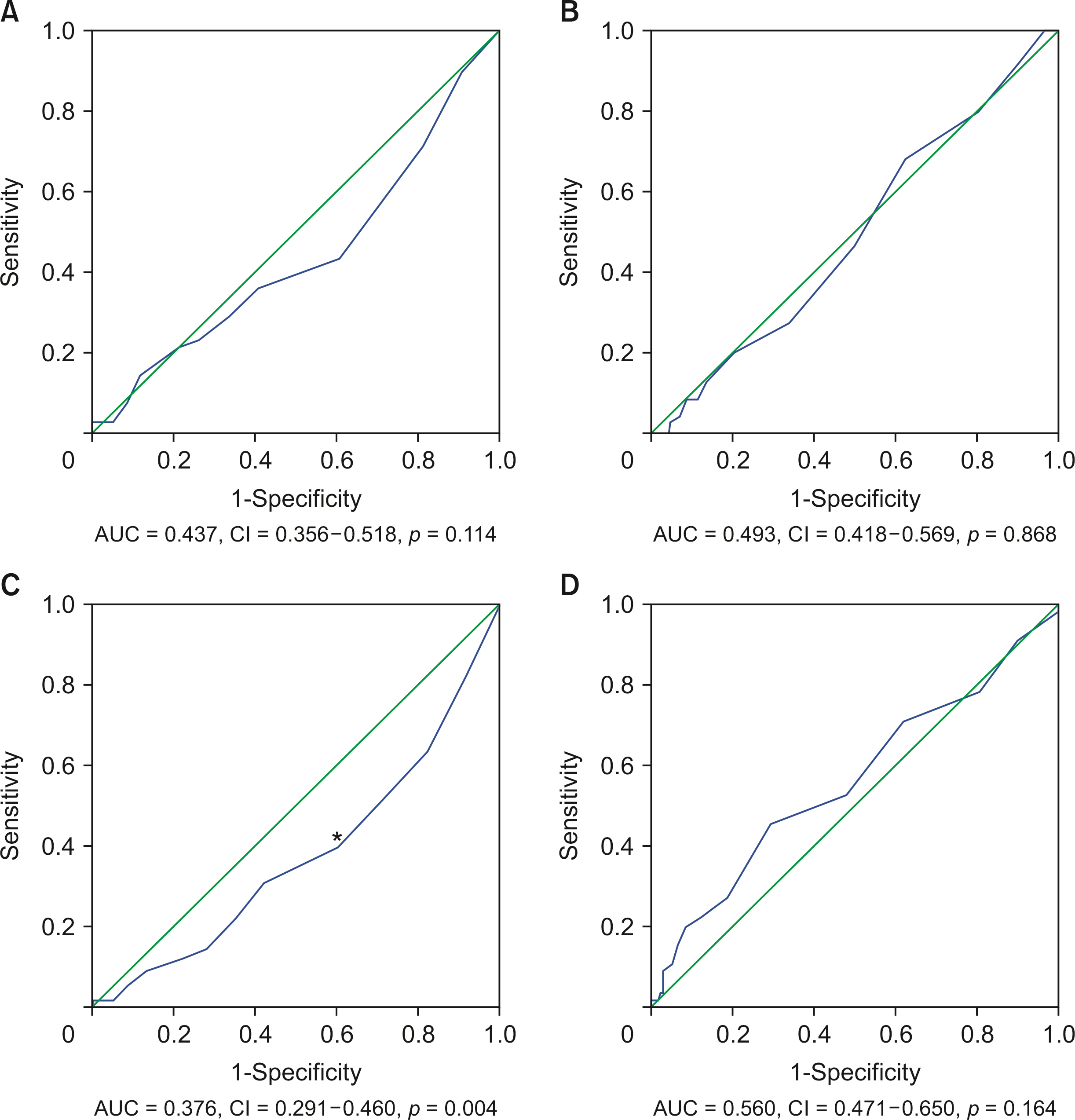
Of 695 patients, 403 had grade I AC and 292 had grade II AC. According to the receiver operating characteristic curve and multivariate logistic regression analyses, an interval from symptom onset to PTGBD of > 3.5 days and an interval from PTGBD to LC of > 7.5 days were significant predictors of DS and PPO, respectively, in grade I AC. In grade II AC, the timing of PTGBD and subsequent LC were not statistically related to DS or PPO.
Conclusions
In grade I AC, performing PTGBD within 3.5 days after symptom onset can reduce surgical difficulties and subsequently performing LC within 7.5 days after PTGBD can improve postoperative outcomes. In grade II AC, early PTGBD cannot improve the surgical difficulty. In addition, the timing of subsequent LC is not correlated with surgical difficulties or postoperative outcomes.
Figure
Cited by 1 articles
-
Comparison between percutaneous transhepatic gallbladder drainage and upfront laparoscopic cholecystectomy in patients with moderate-to-severe acute cholecystitis: a propensity score-matched analysis
Okjoo Lee, Yong Chan Shin, Youngju Ryu, So Jeong Yoon, Hongbeom Kim, Sang Hyun Shin, Jin Seok Heo, Woohyun Jung, Chang-Sup Lim, In Woong Han
Ann Surg Treat Res. 2023;105(5):310-318. doi: 10.4174/astr.2023.105.5.310.
Reference
-
1. Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, et al. Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018; 25:55–72. DOI: 10.1002/jhbp.516. PMID: 29045062.2. Radder RW. 1980; Ultrasonically guided percutaneous catheter drainage for gallbladder empyema. Diagn Imaging. 49:330–333. PMID: 7215096.3. Horn T, Christensen SD, Kirkegård J, Larsen LP, Knudsen AR, Mortensen FV. 2015; Percutaneous cholecystostomy is an effective treatment option for acute calculous cholecystitis: a 10-year experience. HPB (Oxford). 17:326–331. DOI: 10.1111/hpb.12360. PMID: 25395238. PMCID: PMC4368396.
Article4. Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018; 25:41–54. DOI: 10.1002/jhbp.515. PMID: 29032636.5. Habib FA, Kolachalam RB, Khilnani R, Preventza O, Mittal VK. 2001; Role of laparoscopic cholecystectomy in the management of gangrenous cholecystitis. Am J Surg. 181:71–75. DOI: 10.1016/S0002-9610(00)00525-0. PMID: 11248180.
Article6. Mayhew D, Mendonca V, Murthy BVS. 2019; A review of ASA physical status - historical perspectives and modern developments. Anaesthesia. 74:373–379. DOI: 10.1111/anae.14569. PMID: 30648259.
Article7. Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, et al. Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018; 25:73–86. DOI: 10.1002/jhbp.517. PMID: 29095575.8. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. 2009; The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 250:187–196. DOI: 10.1097/SLA.0b013e3181b13ca2. PMID: 19638912.9. Han IW, Jang JY, Kang MJ, Lee KB, Lee SE, Kim SW. 2012; Early versus delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage. J Hepatobiliary Pancreat Sci. 19:187–193. DOI: 10.1007/s00534-011-0458-6. PMID: 21938408.
Article10. Choi JW, Park SH, Choi SY, Kim HS, Kim TH. 2012; Comparison of clinical result between early laparoscopic cholecystectomy and delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage for patients with complicated acute cholecystitis. Korean J Hepatobiliary Pancreat Surg. 16:147–153. DOI: 10.14701/kjhbps.2012.16.4.147. PMID: 26388926. PMCID: PMC4575000.
Article11. Sakamoto T, Fujiogi M, Matsui H, Fushimi K, Yasunaga H. 2020; Timing of cholecystectomy after percutaneous transhepatic gallbladder drainage for acute cholecystitis: a nationwide inpatient database study. HPB (Oxford). 22:920–926. DOI: 10.1016/j.hpb.2019.10.2438. PMID: 31732466.
Article12. Inoue K, Ueno T, Nishina O, Douchi D, Shima K, Goto S, et al. 2017; Optimal timing of cholecystectomy after percutaneous gallbladder drainage for severe cholecystitis. BMC Gastroenterol. 17:71. DOI: 10.1186/s12876-017-0631-8. PMID: 28569137. PMCID: PMC5452332.
Article13. Yamada K, Yamashita Y, Yamada T, Takeno S, Noritomi T. 2015; Optimal timing for performing percutaneous transhepatic gallbladder drainage and subsequent cholecystectomy for better management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 22:855–861. DOI: 10.1002/jhbp.294. PMID: 26479740.
Article14. Iwashita Y, Ohyama T, Honda G, Hibi T, Yoshida M, Miura F, et al. 2016; What are the appropriate indicators of surgical difficulty during laparoscopic cholecystectomy? Results from a Japan-Korea-Taiwan multinational survey. J Hepatobiliary Pancreat Sci. 23:533–547. DOI: 10.1002/jhbp.375. PMID: 27490841.
Article15. Schrenk P, Woisetschläger R, Rieger R, Wayand WU. 1998; A diagnostic score to predict the difficulty of a laparoscopic cholecystectomy from preoperative variables. Surg Endosc. 12:148–150. DOI: 10.1007/s004649900616. PMID: 9479730.
Article16. Sakuramoto S, Sato S, Okuri T, Sato K, Hiki Y, Kakita A. 2000; Preoperative evaluation to predict technical difficulties of laparoscopic cholecystectomy on the basis of histological inflammation findings on resected gallbladder. Am J Surg. 179:114–121. DOI: 10.1016/S0002-9610(00)00248-8. PMID: 10773146.
Article17. Simopoulos C, Botaitis S, Polychronidis A, Tripsianis G, Karayiannakis AJ. 2005; Risk factors for conversion of laparoscopic cholecystectomy to open cholecystectomy. Surg Endosc. 19:905–909. DOI: 10.1007/s00464-004-2197-0. PMID: 15868267.
Article18. Lipman JM, Claridge JA, Haridas M, Martin MD, Yao DC, Grimes KL, et al. 2007; Preoperative findings predict conversion from laparoscopic to open cholecystectomy. Surgery. 142:556–563. discussion 563–565. DOI: 10.1016/j.surg.2007.07.010. PMID: 17950348.
Article19. Ábrahám S, Tóth I, Benkő R, Matuz M, Kovács G, Morvay Z, et al. Surgical outcome of percutaneous transhepatic gallbladder drainage in acute cholecystitis: ten years' experience at a tertiary care centre. Surg Endosc. 2021. https://doi.org/10.1007/s00464-021-08573-0[in press]. DOI: 10.1007/s00464-021-08573-0. PMID: 34415432. PMCID: PMC9001534.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Early Versus Delayed Laparoscopic Cholecystectomy after Percutaneous Transhepatic Gallbladder Drainage (PTGBD) for Patient with Complicated Acute Cholecystitis
- Percutaneous Gallbladder Drainage and Optimal Timing for Successful Laparoscopic Cholecystectomy in Acute Complicated Cholecystitis
- The Benefits of Percutaneous Transhepatic Gallbladder Drainage prior to Laparoscopic Cholecystectomy for Acute Cholecystitis
- A Case of Gallbladder Perforation Treated By Percutaneous Transhepatic Cholecystic Drainage and Percutaneous Peritoneal Drainage
- Current Status of Endoscopic Gallbladder Drainage