Diabetes Metab J.
2022 Mar;46(2):260-272. 10.4093/dmj.2021.0125.
Impact of COVID-19 Lockdown on the Metabolic Control Parameters in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Faculty of Medicine, Airlangga University, Surabaya, Indonesia
- 2Department of Public Health and Preventive Medicine, Airlangga University, Surabaya, Indonesia
- 3Department of Internal Medicine, Airlangga University, Surabaya, Indonesia
- KMID: 2527719
- DOI: http://doi.org/10.4093/dmj.2021.0125
Abstract
- Background
Abrupt implementation of lockdowns during the coronavirus disease 2019 (COVID-19) pandemic affected the management of diabetes mellitus in patients worldwide. Limited access to health facilities and lifestyle changes potentially affected metabolic parameters in patients at risk. We conducted a meta-analysis to determine any differences in the control of metabolic parameters in patients with diabetes, before and during lockdown.
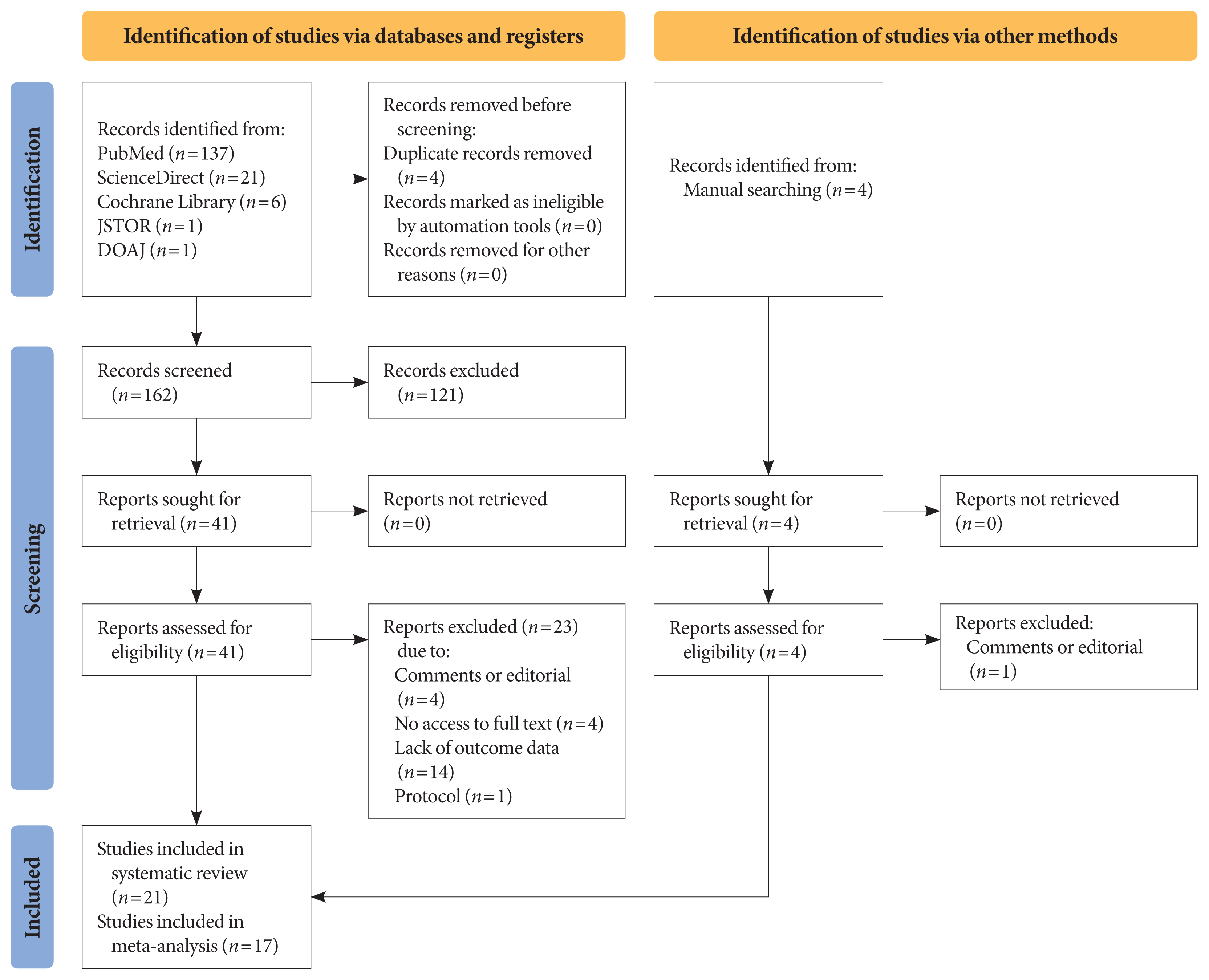
Methods
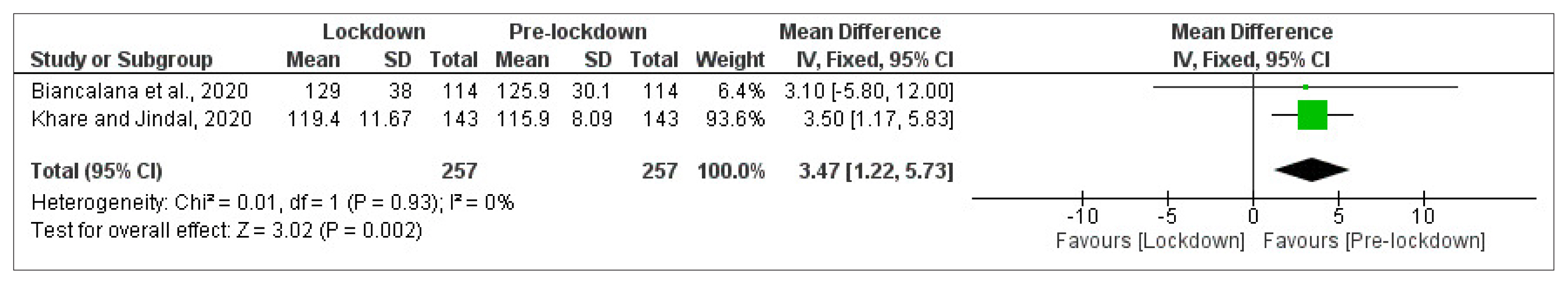
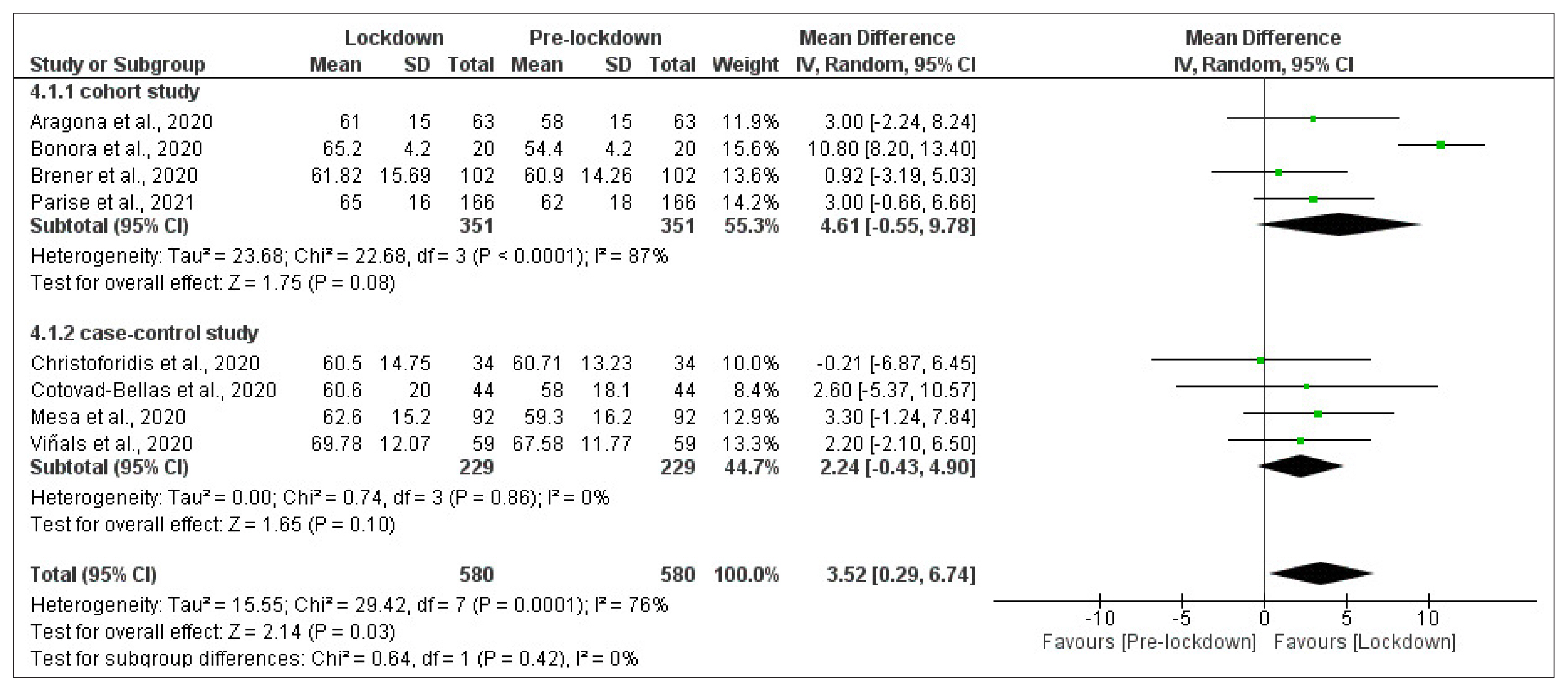
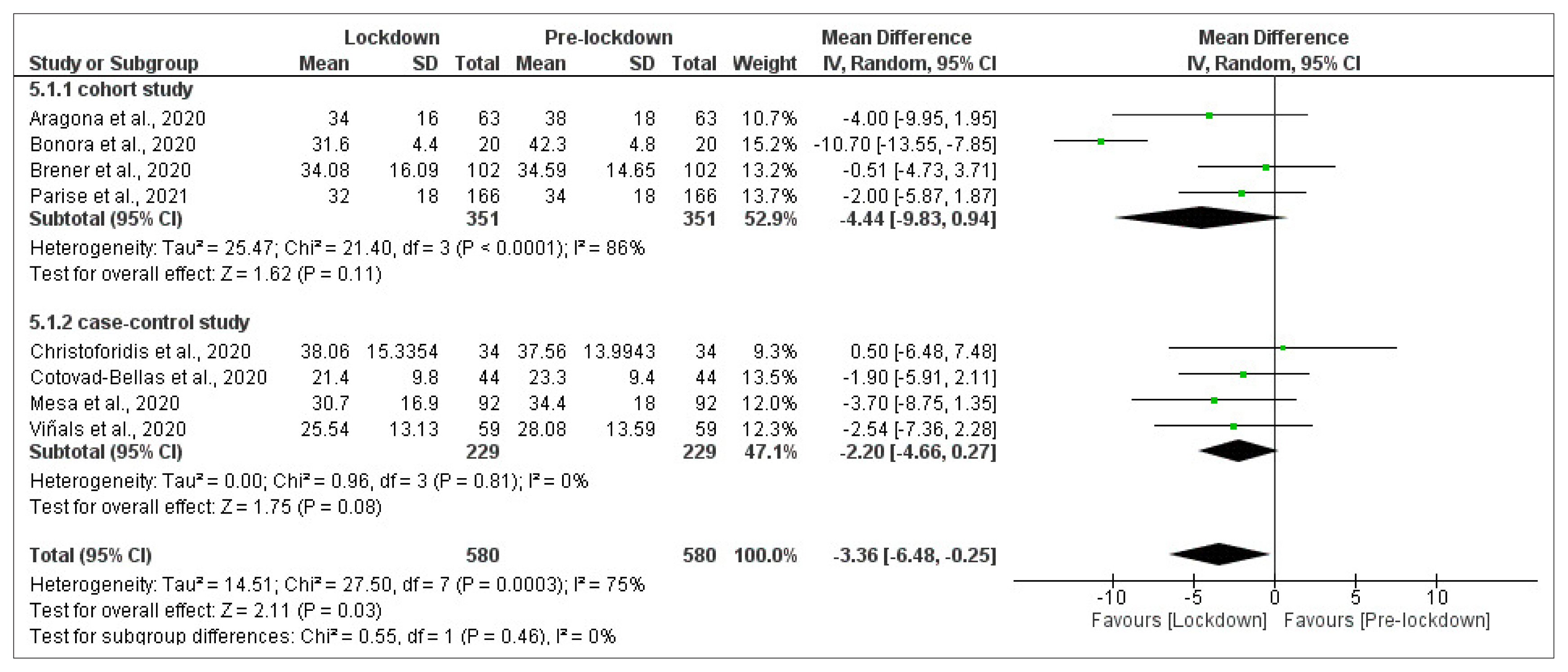
We performed searches of five databases. Meta-analyses were carried out using random- or fixed-effect approaches to glycaemic control parameters as the primary outcome: glycosylated hemoglobin (HbA1c), random blood glucose (RBG), fasting blood glucose (FBG), time-in-range (TIR), time-above-range (TAR), time-below-range (TBR). Mean difference (MD), confidence interval (CI), and P value were calculated. Lipid profile was a secondary outcome and is presented as a descriptive analysis.
Results
Twenty-one studies enrolling a total of 3,992 patients with type 1 or type 2 diabetes mellitus (T1DM or T2DM) were included in the study. Patients with T1DM showed a significant improvement of TIR and TAR (MD=3.52% [95% CI, 0.29 to 6.74], I2=76%, P=0.03; MD=–3.36% [95% CI, –6.48 to –0.25], I2=75%, P=0.03), while FBG among patients with T2DM significantly worsened (MD=3.47 mg/dL [95% CI, 1.22 to 5.73], I2=0%, P<0.01). No significant difference was found in HbA1c, RBG, and TBR. Use of continuous glucose monitoring in T1DM facilitated good glycaemic control. Significant deterioration of lipid parameters during lockdown, particularly triglyceride, was observed.
Conclusion
Implementation of lockdowns during the COVID-19 pandemic did not worsen glycaemic control in patients with diabetes. Other metabolic parameters improved during lockdown, though lipid parameters, particularly triglyceride, worsened.
Figure
Reference
-
1. Alshareef R, Al Zahrani A, Alzahrani A, Ghandoura L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab Syndr. 2020; 14:1583–7.
Article2. Cheikh Ismail L, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Abu Jamous DO, et al. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: a cross-sectional study. Nutrients. 2020; 12:3314.
Article3. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attina A, Cinelli G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020; 18:229.
Article4. Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartin A, Sampedro-Nunez MA, Davalos A, et al. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020; 12:2327.
Article5. Ghosh A, Arora B, Gupta R, Anoop S, Misra A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab Syndr. 2020; 14:917–20.
Article6. van der Linden J, Welsh JB, Hirsch IB, Garg SK. Real-time continuous glucose monitoring during the coronavirus disease 2019 pandemic and its impact on time in range. Diabetes Technol Ther. 2021; 23:S1–7.
Article7. Rodbard D. Continuous glucose monitoring: a review of recent studies demonstrating improved glycemic outcomes. Diabetes Technol Ther. 2017; 19:S25–37.
Article8. Vettoretti M, Cappon G, Acciaroli G, Facchinetti A, Sparacino G. Continuous glucose monitoring: current use in diabetes management and possible future applications. J Diabetes Sci Technol. 2018; 12:1064–71.
Article9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71.10. Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool. Methodological research. J Eval Clin Pract. 2012; 18:12–8.
Article11. Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019; 42:1593–603.12. Alaqeel A, Aljuraibah F, Alsuhaibani M, Huneif M, Alsaheel A, Dubayee MA, et al. The impact of COVID-19 pandemic lockdown on the incidence of new-onset type 1 diabetes and ketoacidosis among Saudi children. Front Endocrinol (Lausanne). 2021; 12:669302.
Article13. Aragona M, Rodia C, Bertolotto A, Campi F, Coppelli A, Giannarelli R, et al. Type 1 diabetes and COVID-19: the “lockdown effect”. Diabetes Res Clin Pract. 2020; 170:108468.
Article14. Biancalana E, Parolini F, Mengozzi A, Solini A. Short-term impact of COVID-19 lockdown on metabolic control of patients with well-controlled type 2 diabetes: a single-centre observational study. Acta Diabetol. 2021; 58:431–6.
Article15. Parise M, Tartaglione L, Cutruzzola A, Maiorino MI, Esposito K, Pitocco D, et al. Teleassistance for patients with type 1 diabetes during the COVID-19 pandemic: results of a pilot study. J Med Internet Res. 2021; 23:e24552.
Article16. Ruissen MM, Regeer H, Landstra CP, Schroijen M, Jazet I, Nijhoff MF, et al. Increased stress, weight gain and less exercise in relation to glycemic control in people with type 1 and type 2 diabetes during the COVID-19 pandemic. BMJ Open Diabetes Res Care. 2021; 9:e002035.
Article17. Cotovad-Bellas L, Tejera-Perez C, Prieto-Tenreiro A, Sanchez-Bao A, Bellido-Guerrero D. The challenge of diabetes home control in COVID-19 times: proof is in the pudding. Diabetes Res Clin Pract. 2020; 168:108379.
Article18. Karatas S, Yesim T, Beysel S. Impact of lockdown COVID-19 on metabolic control in type 2 diabetes mellitus and healthy people. Prim Care Diabetes. 2021; 15:424–7.
Article19. Mesa A, Vinals C, Pueyo I 1st, Roca D, Vidal M, Gimenez M, et al. The impact of strict COVID-19 lockdown in Spain on glycemic profiles in patients with type 1 diabetes prone to hypoglycemia using standalone continuous glucose monitoring. Diabetes Res Clin Pract. 2020; 167:108354.
Article20. Vinals C, Mesa A, Roca D, Vidal M, Pueyo I, Conget I, et al. Management of glucose profile throughout strict COVID-19 lockdown by patients with type 1 diabetes prone to hypoglycaemia using sensor-augmented pump. Acta Diabetol. 2021; 58:383–8.
Article21. Al Agha AE, Alharbi RS, Almohammadi OA, Yousef SY, Sulimani AE, Alaama RA. Impact of COVID-19 lockdown on glycemic control in children and adolescents. Saudi Med J. 2021; 42:44–8.
Article22. Verma A, Rajput R, Verma S, Balania V, Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 diabetes mellitus. Diabetes Metab Syndr. 2020; 14:1213–6.
Article23. Barchetta I, Cimini FA, Bertoccini L, Ceccarelli V, Spaccarotella M, Baroni MG, et al. Effects of work status changes and perceived stress onglycaemiccontrol in individuals with type 1 diabetes during COVID-19 lockdown in Italy. Diabetes Res Clin Pract. 2020; 170:108513.24. Bonora BM, Boscari F, Avogaro A, Bruttomesso D, Fadini GP. Glycaemic control among people with type 1 diabetes during lockdown for the SARS-CoV-2 outbreak in Italy. Diabetes Ther. 2020; 11:1–11.
Article25. Brener A, Mazor-Aronovitch K, Rachmiel M, Levek N, Barash G, Pinhas-Hamiel O, et al. Lessons learned from the continuous glucose monitoring metrics in pediatric patients with type 1 diabetes under COVID-19 lockdown. Acta Diabetol. 2020; 57:1511–7.
Article26. Christoforidis A, Kavoura E, Nemtsa A, Pappa K, Dimitriadou M. Coronavirus lockdown effect on type 1 diabetes management on children wearing insulin pump equipped with continuous glucose monitoring system. Diabetes Res Clin Pract. 2020; 166:108307.27. Potier L, Hansel B, Larger E, Gautier JF, Carreira D, Assemien R, et al. Stay-at-home orders during the COVID-19 pandemic, an opportunity to improve glucose control through behavioral changes in type 1 diabetes. Diabetes Care. 2021; 44:839–43.
Article28. Khare J, Jindal S. Observational study on effect of lock down due to COVID 19 on glycemic control in patients with diabetes: experience from Central India. Diabetes Metab Syndr. 2020; 14:1571–4.
Article29. Martens T, Beck RW, Bailey R, Ruedy KJ, Calhoun P, Peters AL, et al. Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: a randomized clinical trial. JAMA. 2021; 325:2262–72.30. Jung CH, Choi KM. Impact of high-carbohydrate diet on metabolic parameters in patients with type 2 diabetes. Nutrients. 2017; 9:322.
Article31. Figueiro TH, Arins G, Santos C, Cembranel F, Medeiros PA, d’Orsi E, et al. Association of objectively measured sedentary behavior and physical activity with cardiometabolic risk markers in older adults. PLoS One. 2019; 14:e0210861.
Article32. Umpierrez GE, P Kovatchev B. Glycemic variability: how to measure and its clinical implication for type 2 diabetes. Am J Med Sci. 2018; 356:518–27.
Article33. Dover AR, Ritchie SA, McKnight JA, Strachan M, Zammitt NN, Wake DJ, et al. Assessment of the effect of the COVID-19 lockdown on glycaemic control in people with type 1 diabetes using flash glucose monitoring. Diabet Med. 2021; 38:e14374.
Article34. Zachary Z, Brianna F, Brianna L, Garrett P, Jade W, Alyssa D, et al. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes Res Clin Pract. 2020; 14:210–6.
Article35. Longo M, Caruso P, Petrizzo M, Castaldo F, Sarnataro A, Gicchino M, et al. Glycemic control in people with type 1 diabetes using a hybrid closed loop system and followed by telemedicine during the COVID-19 pandemic in Italy. Diabetes Res Clin Pract. 2020; 169:108440.
Article36. Neto JCGL, da Silva AP, de Araujo MFM, Damasceno MMC, Landim MBP, de Freitas RWJF. Metabolic control and medication adherence in people with diabetes mellitus. Acta Paul Enferm. 2017; 30:152–8.37. Ghesquiere L, Garabedian C, Drumez E, Lemaitre M, Cazaubiel M, Bengler C, et al. Effects of COVID-19 pandemic lockdown on gestational diabetes mellitus: a retrospective study. Diabetes Metab. 2021; 47:101201.38. Di Dalmazi G, Maltoni G, Bongiorno C, Tucci L, Di Natale V, Moscatiello S, et al. Comparison of the effects of lockdown due to COVID-19 on glucose patterns among children, adolescents, and adults with type 1 diabetes: CGM study. BMJ Open Diabetes Res Care. 2020; 8:e001664.
Article39. Tornese G, Ceconi V, Monasta L, Carletti C, Faleschini E, Barbi E. Glycemic control in type 1 diabetes mellitus during COVID-19 quarantine and the role of in-home physical activity. Diabetes Technol Ther. 2020; 22:462–7.
Article40. Cappon G, Vettoretti M, Sparacino G, Facchinetti A. Continuous glucose monitoring sensors for diabetes management: a review of technologies and applications. Diabetes Metab J. 2019; 43:383–97.
Article41. Edelman SV, Argento NB, Pettus J, Hirsch IB. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care. 2018; 41:2265–74.
Article42. Polonsky WH, Hessler D, Ruedy KJ, Beck RW. DIAMOND Study Group. The impact of continuous glucose monitoring on markers of quality of life in adults with type 1 diabetes: further findings from the DIAMOND randomized clinical trial. Diabetes Care. 2017; 40:736–41.
Article43. Maiorino MI, Signoriello S, Maio A, Chiodini P, Bellastella G, Scappaticcio L, et al. Effects of continuous glucose monitoring on metrics of glycemic control in diabetes: a systematic review with meta-analysis of randomized controlled trials. Diabetes Care. 2020; 43:1146–56.
Article44. Langendam M, Luijf YM, Hooft L, Devries JH, Mudde AH, Scholten RJ. Continuous glucose monitoring systems for type 1 diabetes mellitus. Cochrane Database Syst Rev. 2012; 1:CD008101.
Article45. Costantino S, Paneni F, Battista R, Castello L, Capretti G, Chiandotto S, et al. Impact of glycemic variability on chromatin remodeling, oxidative stress, and endothelial dysfunction in patients with type 2 diabetes and with target HbA1c levels. Diabetes. 2017; 66:2472–82.
Article46. Kaze AD, Santhanam P, Erqou S, Ahima RS, Echouffo-Tcheugui JB. Long-term variability of glycemic markers and risk of all-cause mortality in type 2 diabetes: the Look AHEAD study. BMJ Open Diabetes Res Care. 2020; 8:e001753.
Article47. Azizi F, Hadaegh F, Hosseinpanah F, Mirmiran P, Amouzegar A, Abdi H, et al. Metabolic health in the Middle East and North Africa. Lancet Diabetes Endocrinol. 2019; 7:866–79.
Article48. Seghieri M, Trico D, Natali A. The impact of triglycerides on glucose tolerance: lipotoxicity revisited. Diabetes Metab. 2017; 43:314–22.
Article49. Marston NA, Giugliano RP, Im K, Silverman MG, O’Donoghue ML, Wiviott SD, et al. Association between triglyceride lowering and reduction of cardiovascular risk across multiple lipid-lowering therapeutic classes: a systematic review and meta-regression analysis of randomized controlled trials. Circulation. 2019; 140:1308–17.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of COVID-19 lockdown on blood glucose levels in pediatric patients with type 1 diabetes mellitus
- Diabetes Prevention and Measures to Ensuring a Healthy Lifestyle during COVID-19 Pandemic and after
- Did the COVID-19 pandemic impact the surgical treatment of febrile acute appendicitis at a single center in Korea, a country not under lockdown? Observational cohort study
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis
- Predictors of Mortality in Patients with COVID-19: A Systematic Review and Meta-analysis