Korean J Orthod.
2022 Mar;52(2):85-101. 10.4041/kjod.2022.52.2.85.
Characterization of facial asymmetry phenotypes in adult patients with skeletal Class III malocclusion using three-dimensional computed tomography and cluster analysis
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Seoul National University, Seoul, Korea
- 2Department of Orthodontics, Kyung Hee University School of Dentistry, Seoul, Korea
- 3Department of Oral and Maxillofacial Surgery, School of Dentistry, Seoul National University, Seoul, Korea
- 4Department of Orthodontics, School of Dentistry and Dental Research Institute, Seoul National University, Seoul, Korea
- KMID: 2527453
- DOI: http://doi.org/10.4041/kjod.2022.52.2.85
Abstract
Objective
To classify facial asymmetry (FA) phenotypes in adult patients with skeletal Class III (C-III) malocclusion.
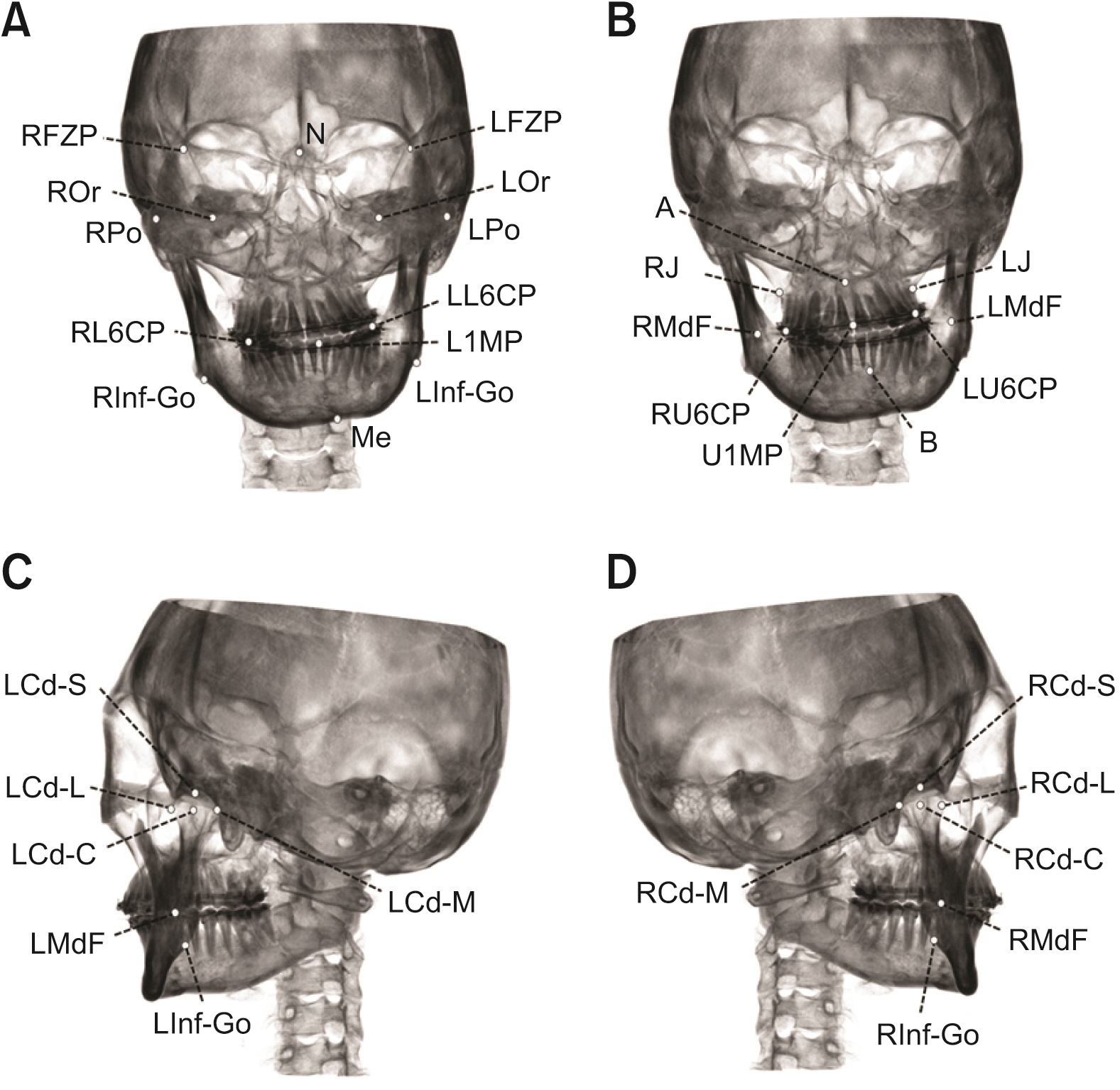
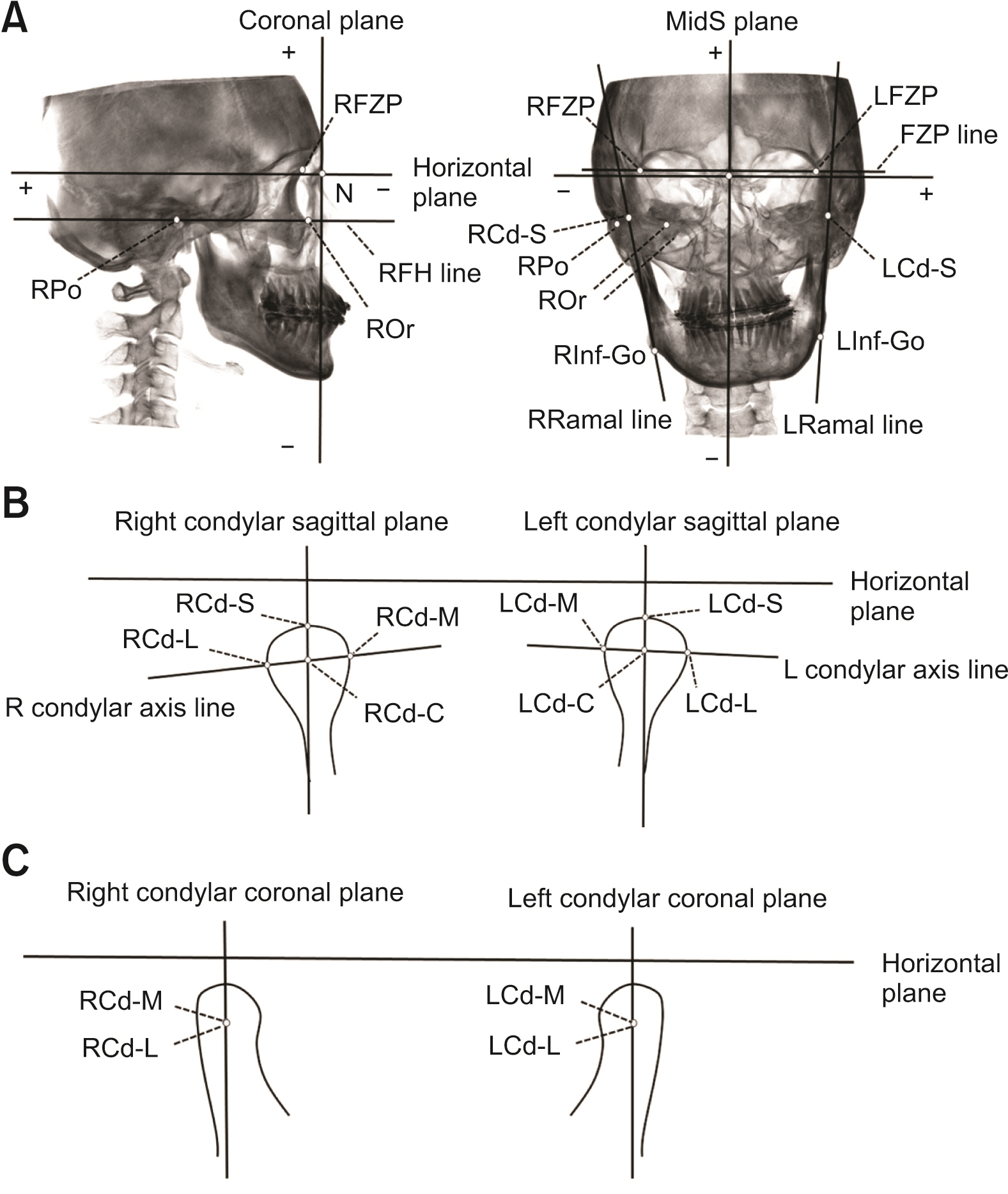
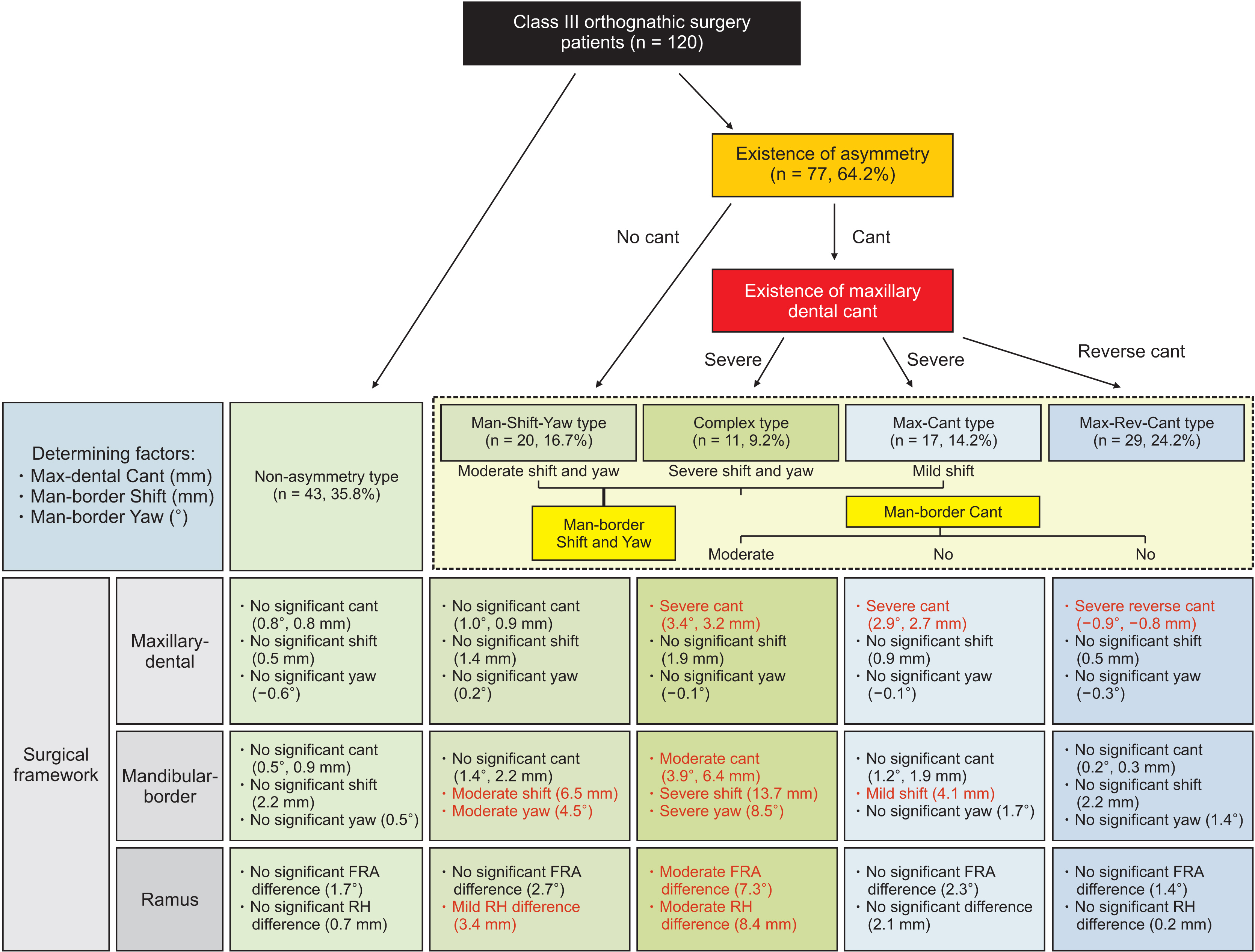
Methods
A total of 120 C-III patients who underwent orthognathic surgery (OGS) and whose three-dimensional computed tomography images were taken one month prior to OGS were evaluated. Thirty hard tissue landmarks were identified. After measurement of 22 variables, including cant (°, mm), shift (mm), and yaw (°) of the maxilla, maxillary dentition (Max-dent), mandibular dentition, mandible, and mandibular border (Man-border) and differences in the frontal ramus angle (FRA, °) and ramus height (RH, mm), K-means cluster analysis was conducted using three variables (cant in the Max-dent [mm] and shift [mm] and yaw [°] in the Manborder). Statistical analyses were conducted to characterize the differences in the FA variables among the clusters.
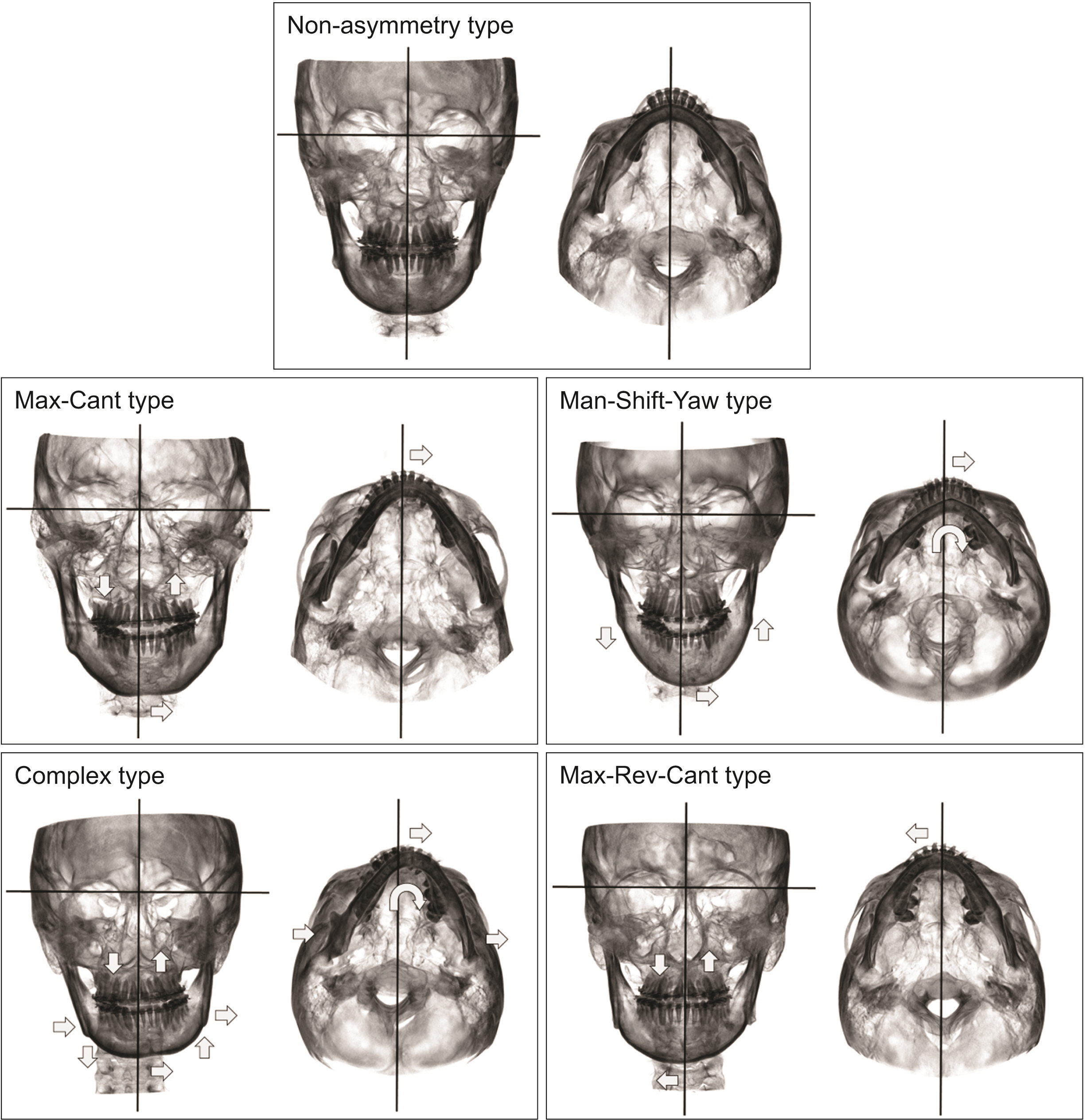
Results
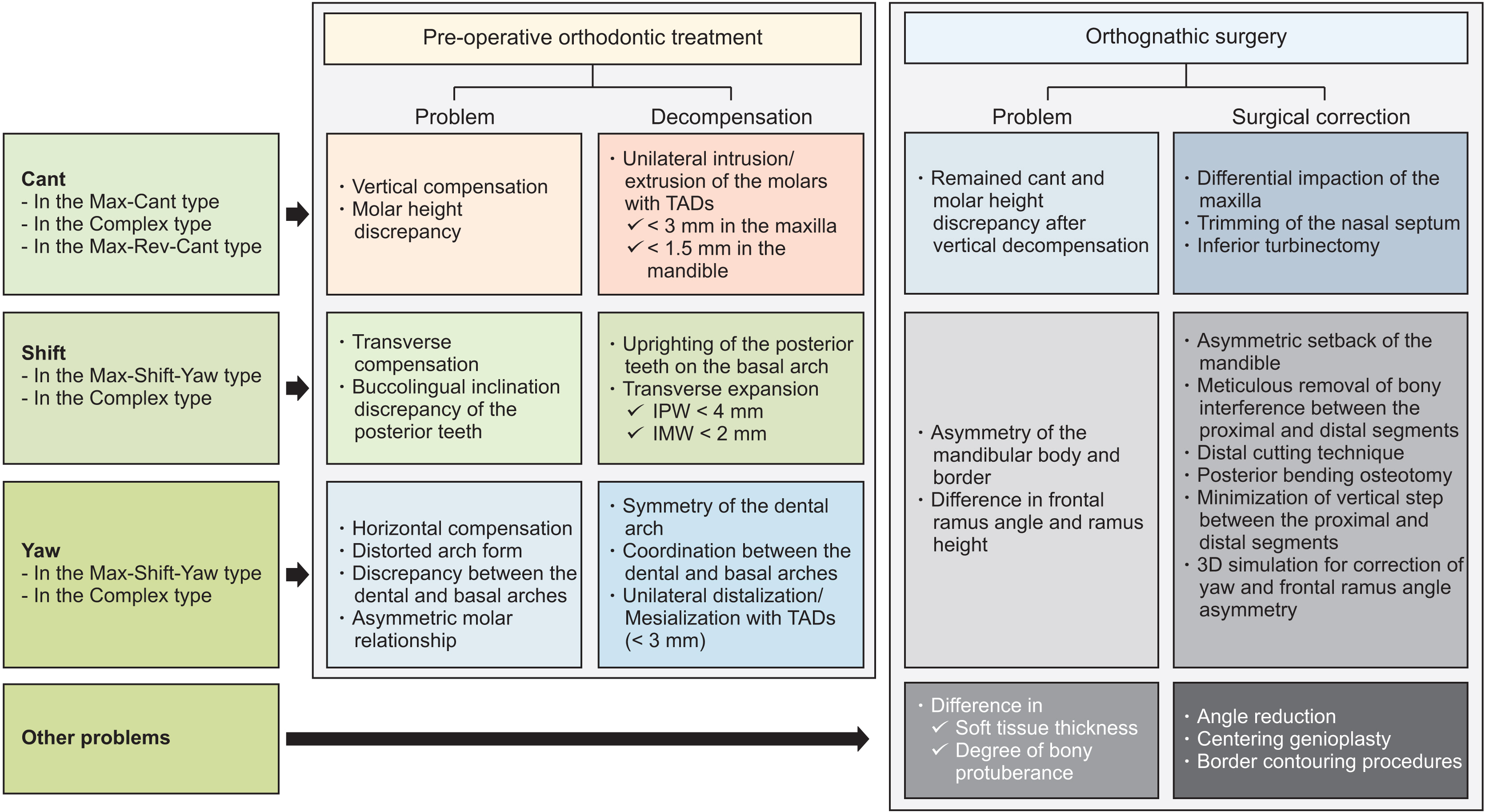
The FA phenotypes were classified into five types: 1) non-asymmetry type (35.8%); 2) maxillary-cant type (14.2%; severe cant of the Max-dent, mild shift of the Man-border); 3) mandibularshift and yaw type (16.7%; moderate shift and yaw of the Man-border, mild RH-difference); 4) complex type (9.2%; severe cant of the Max-dent, moderate cant, severe shift, and severe yaw of the Man-border, moderate differences in FRA and RH); and 5) maxillary reverse-cant type (24.2%; reverse-cant of the Max-dent). Strategic decompensation by pre-surgical orthodontic treatment and considerations for OGS planning were proposed according to the FA phenotypes.
Conclusions
This FA phenotype classification may be an effective tool for differential diagnosis and surgical planning for Class III patients with FA.
Figure
Reference
-
References
1. Cheong YW, Lo LJ. 2011; Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J. 34:341–51.2. Piao Y, Kim SJ, Yu HS, Cha JY, Baik HS. 2016; Five-year investigation of a large orthodontic patient population at a dental hospital in South Korea. Korean J Orthod. 46:137–45. DOI: 10.4041/kjod.2016.46.3.137. PMID: 27226959. PMCID: PMC4879316.
Article3. Bergersen EO. 1980; Enlargement and distortion in cephalometric radiography: compensation tables for linear measurements. Angle Orthod. 50:230–44. DOI: 10.1043/0003-3219(1980)050<0230:EADICR>2.0.CO;2. PMID: 6931505.4. Katsumata A, Fujishita M, Maeda M, Ariji Y, Ariji E, Langlais RP. 2005; 3D-CT evaluation of facial asymmetry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 99:212–20. DOI: 10.1016/j.tripleo.2004.06.072. PMID: 15660095.
Article5. Hwang HS, Hwang CH, Lee KH, Kang BC. 2006; Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. Am J Orthod Dentofacial Orthop. 130:779–85. DOI: 10.1016/j.ajodo.2005.02.021. PMID: 17169741.
Article6. Maeda M, Katsumata A, Ariji Y, Muramatsu A, Yoshida K, Goto S, et al. 2006; 3D-CT evaluation of facial asymmetry in patients with maxillofacial deformities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 102:382–90. DOI: 10.1016/j.tripleo.2005.10.057. PMID: 16920547.
Article7. Baek SH, Cho IS, Chang YI, Kim MJ. 2007; Skeletodental factors affecting chin point deviation in female patients with class III malocclusion and facial asymmetry: a three-dimensional analysis using computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 104:628–39. DOI: 10.1016/j.tripleo.2007.03.002. PMID: 17656131.
Article8. Akhil G, Senthil Kumar KP, Raja S, Janardhanan K. 2015; Three-dimensional assessment of facial asymmetry: a systematic review. J Pharm Bioallied Sci. 7(Suppl 2):S433–7. DOI: 10.4103/0975-7406.163491. PMID: 26538893. PMCID: PMC4606635.
Article9. Hwang HS, Youn IS, Lee KH, Lim HJ. 2007; Classification of facial asymmetry by cluster analysis. Am J Orthod Dentofacial Orthop. 132:279.e1–6. DOI: 10.1016/j.ajodo.2007.01.017. PMID: 17826592.
Article10. Baek C, Paeng JY, Lee JS, Hong J. 2012; Morphologic evaluation and classification of facial asymmetry using 3-dimensional computed tomography. J Oral Maxillofac Surg. 70:1161–9. DOI: 10.1016/j.joms.2011.02.135. PMID: 21763045.
Article11. Kim JY, Jung HD, Jung YS, Hwang CJ, Park HS. 2014; A simple classification of facial asymmetry by TML system. J Craniomaxillofac Surg. 42:313–20. DOI: 10.1016/j.jcms.2013.05.019. PMID: 23810748.
Article12. López DF, Botero JR, Muñoz JM, Cárdenas-Perilla R, Moreno M. 2019; Are there mandibular morphological differences in the various facial asymmetry etiologies? A tomographic three-dimensional reconstruction study. J Oral Maxillofac Surg. 77:2324–38. DOI: 10.1016/j.joms.2019.05.020. PMID: 31276657.
Article13. Tyan S, Park HS, Janchivdorj M, Han SH, Kim SJ, Ahn HW. 2016; Three-dimensional analysis of molar compensation in patients with facial asymmetry and mandibular prognathism. Angle Orthod. 86:421–30. DOI: 10.2319/030915-142.1. PMID: 26192894. PMCID: PMC8601728.
Article14. Kim KA, Lee JW, Park JH, Kim BH, Ahn HW, Kim SJ. 2017; Targeted presurgical decompensation in patients with yaw-dependent facial asymmetry. Korean J Orthod. 47:195–206. DOI: 10.4041/kjod.2017.47.3.195. PMID: 28523246. PMCID: PMC5432441.
Article15. Chen YJ, Yao CC, Chang ZC, Lai HH, Yeh KJ, Kok SH. 2019; Characterization of facial asymmetry in skeletal Class III malocclusion and its implications for treatment. Int J Oral Maxillofac Surg. 48:1533–41. DOI: 10.1016/j.ijom.2019.06.014. PMID: 31235392.
Article16. Kwon SM, Baik HS, Jung HD, Jang W, Choi YJ. 2019; Diagnosis and surgical outcomes of facial asymmetry according to the occlusal cant and menton deviation. J Oral Maxillofac Surg. 77:1261–75. DOI: 10.1016/j.joms.2019.01.028. PMID: 30794815.
Article17. Hong M, Kim MJ, Shin HJ, Cho HJ, Baek SH. 2020; Three-dimensional surgical accuracy between virtually planned and actual surgical movements of the maxilla in two-jaw orthognathic surgery. Korean J Orthod. 50:293–303. DOI: 10.4041/kjod.2020.50.5.293. PMID: 32938822. PMCID: PMC7500567.
Article18. Hwang HS, Thiesen G, Araújo TM, Freitas MP, Motta AT. 2016; An interview with Hyeon-Shik Hwang. Dental Press J Orthod. 21:24–33. DOI: 10.1590/2177-6709.21.1.024-033.int. PMID: 27007758. PMCID: PMC4816582.
Article19. Joondeph DR. 2000; Mysteries of asymmetries. Am J Orthod Dentofacial Orthop. 117:577–9. DOI: 10.1016/S0889-5406(00)70205-8. PMID: 10799120.
Article20. Tay DK. 1994; Physiognomy in the classification of individuals with a lateral preference in mastication. J Orofac Pain. 8:61–72. PMID: 8032332.21. Jeon YJ, Kim YH, Son WS, Hans MG. 2006; Correction of a canted occlusal plane with miniscrews in a patient with facial asymmetry. Am J Orthod Dentofacial Orthop. 130:244–52. DOI: 10.1016/j.ajodo.2006.04.016. PMID: 16905071.
Article22. Takano-Yamamoto T, Kuroda S. 2007; Titanium screw anchorage for correction of canted occlusal plane in patients with facial asymmetry. Am J Orthod Dentofacial Orthop. 132:237–42. DOI: 10.1016/j.ajodo.2005.12.032. PMID: 17693376.
Article23. Fleming PS, Lee RT, Mcdonald T, Pandis N, Johal A. 2014; The timing of significant arch dimensional changes with fixed orthodontic appliances: data from a multicenter randomised controlled trial. J Dent. 42:1–6. DOI: 10.1016/j.jdent.2013.11.010. PMID: 24269833.
Article24. Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, Kawamura H, et al. 2004; Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 125:130–8. DOI: 10.1016/j.ajodo.2003.02.003. PMID: 14765050.
Article25. Yu J, Park JH, Bayome M, Kim S, Kook YA, Kim Y, et al. 2016; Treatment effects of mandibular total arch distalization using a ramal plate. Korean J Orthod. 46:212–9. DOI: 10.4041/kjod.2016.46.4.212. PMID: 27478798. PMCID: PMC4965592.
Article26. On SW, Baek SH, Choi JY. 2020; Quantitative evaluation of the postoperative changes in nasal septal deviation by diverse movement of the maxilla after Le Fort I osteotomy. J Craniofac Surg. 31:1251–15. DOI: 10.1097/SCS.0000000000006430. PMID: 32282480.
Article27. Baek SH, Kim TK, Kim MJ. 2006; Is there any difference in the condylar position and angulation after asymmetric mandibular setback? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 101:155–63. DOI: 10.1016/j.tripleo.2005.04.007. PMID: 16448915.
Article28. Yang HJ, Hwang SJ. 2014; Change in condylar position in posterior bending osteotomy minimizing condylar torque in BSSRO for facial asymmetry. J Craniomaxillofac Surg. 42:325–32. DOI: 10.1016/j.jcms.2013.05.021. PMID: 23816144.
Article29. Ho CT, Lin HH, Liou EJ, Lo LJ. 2017; Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: a qualitative and quantitative study. Sci Rep. 7:40423. DOI: 10.1038/srep40423. PMID: 28071714. PMCID: PMC5223192.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cone-beam computed tomography analysis of transverse dental compensation in patients with skeletal Class III malocclusion and facial asymmetry
- A cehalometric study on facial morphology in angle's Class III malocclusion patients with facial asymmetry
- Comparison of changes in the transverse dental axis between patients with skeletal Class III malocclusion and facial asymmetry treated by orthognathic surgery with and without presurgical orthodontic treatment
- The attrition pattern in Angle Class III malocclusion with facial asymmetry
- Differences in positions of cone-beam computed tomography landmarks in patients with skeletal Class III facial asymmetry according to midsagittal planes