Obstet Gynecol Sci.
2022 Mar;65(2):176-187. 10.5468/ogs.21308.
Impact of hematologic toxicities during concurrent chemoradiation for cervical cancer
- Affiliations
-
- 1Department of Radiation Oncology, Baylor College of Medicine, Houston, TX, USA
- 2Department of Radiation Oncology, University of Texas Health Science Center at Houston McGovern School of Medicine, Houston, TX, USA
- 3Department of Radiation Oncology, Department of Obstetrics and Gynecology, Houston, TX, USA
- 4Department of Radiation Oncology, Department of Radiation Oncology, Baylor College of Medicine, Houston, TX, USA
- 5Department of Radiation Oncology, Division of Gynecologic Oncology, Morsani College of Medicine, University of South Florida/Moffitt Cancer Center, Tempa, FL, USA
- KMID: 2527269
- DOI: http://doi.org/10.5468/ogs.21308
Abstract
Objective
To evaluate the prognostic significance of hematological toxicities during cervical cancer treatment.
Methods
Patients treated for cervical carcinoma with definitive chemoradiation were identified. Toxicities were assessed during weeks 1 to 6 of concurrent external beam radiation and chemotherapy. Outcomes were analyzed using Cox regression analysis.
Results
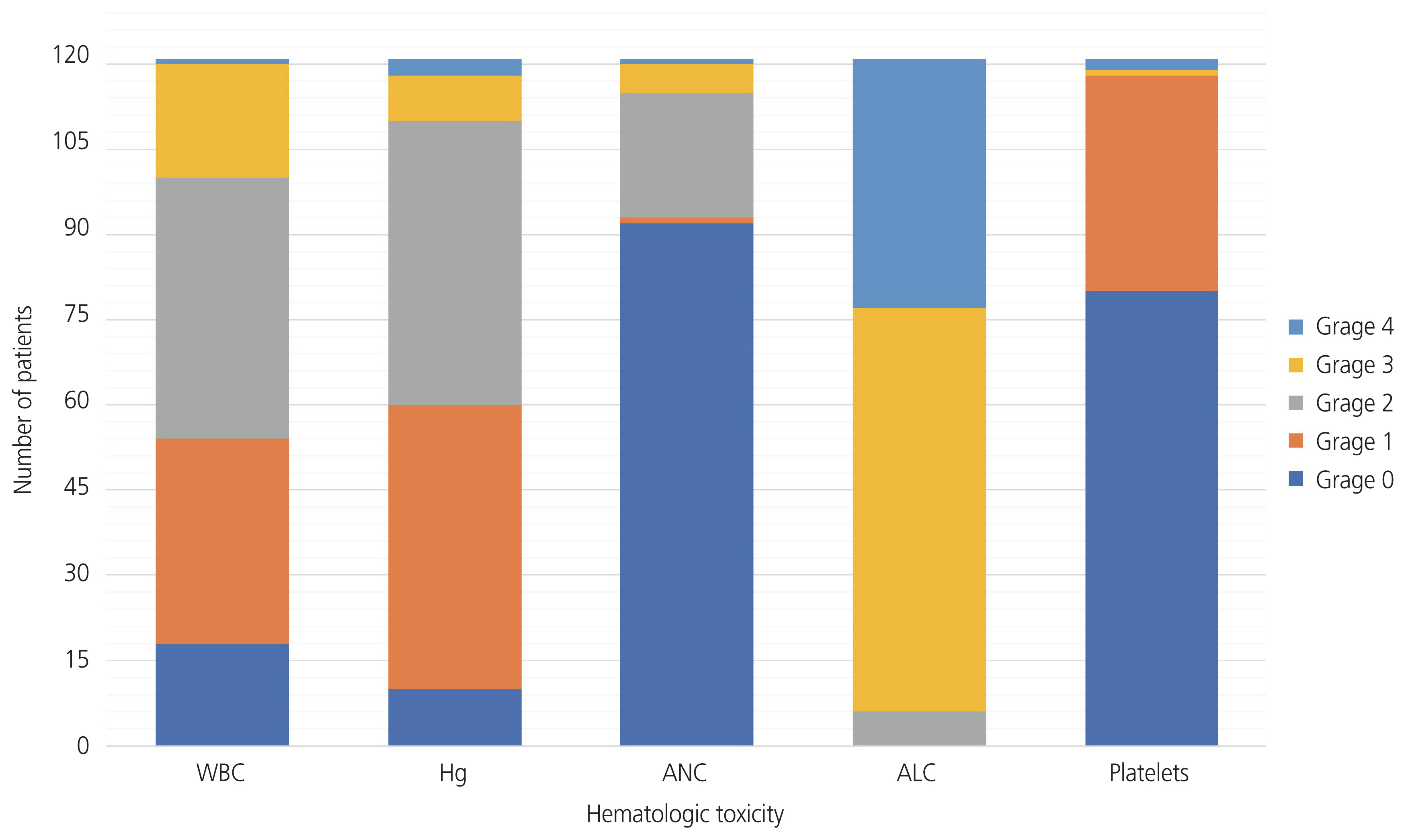
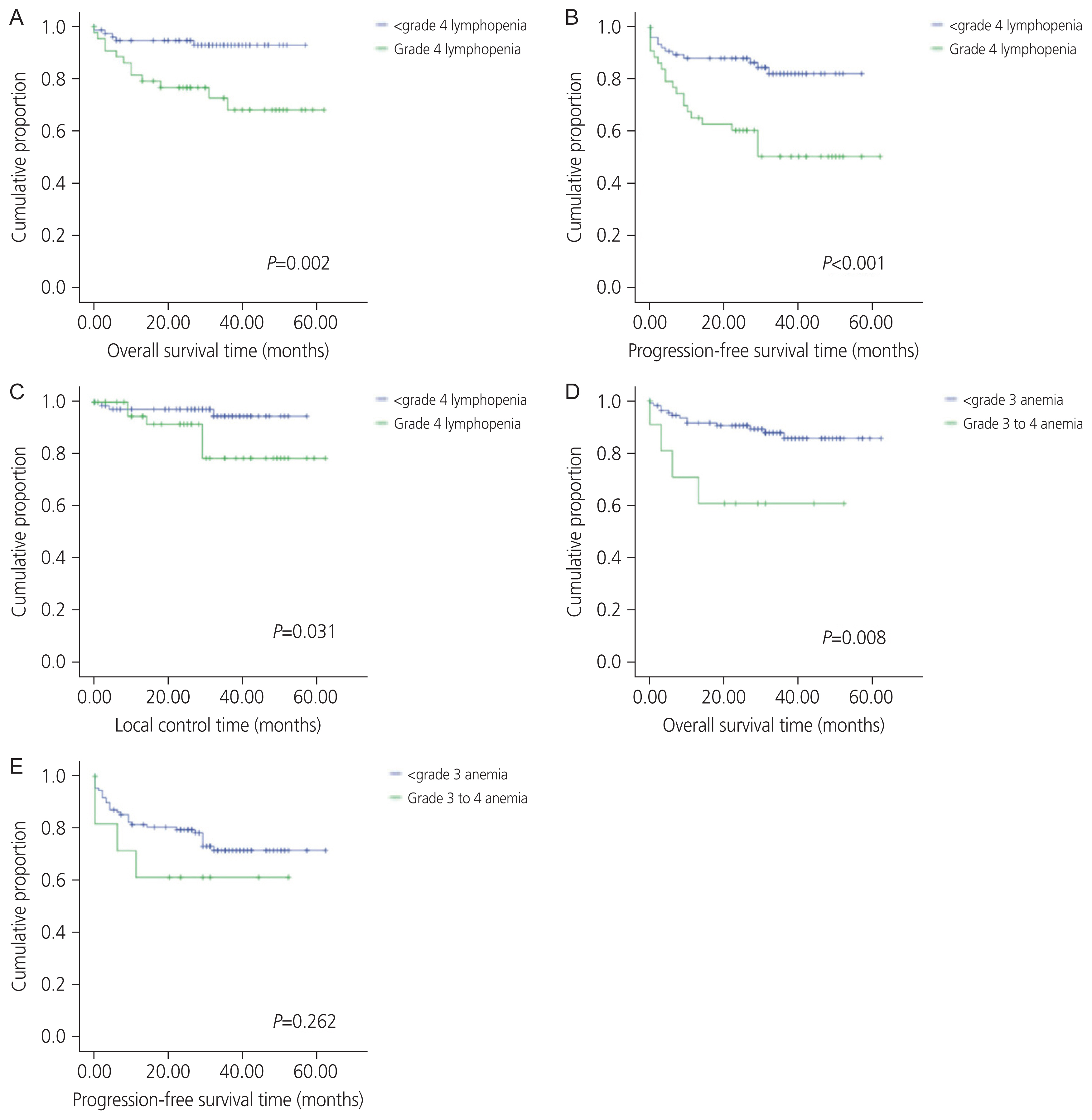
One hundred twenty-one patients with Federation of Gynecology and Obstetrics stage I-III disease were eligible for analysis. Median age at diagnosis was 45 years (interquartile range, 40-52) with median follow-up time of 34 months (95% confidence interval, 30.8-37.2). All patients experienced some grade of hematologic toxicity. The most common grade 3+ toxicities were low absolute lymphocyte count (n=115, 95%), low white blood cell count (n=21, 17%), and anemia (n=11, 9%). The most common grade 4 toxicity was lymphopenia, experienced by 36% of patients (n=44). Grade 4 lymphopenia was associated with reduced overall survival (hazard ratio [HR], 4.5; P=0.005), progression-free survival (HR, 3.4; P=0.001), and local control (HR, 4.1; P=0.047). Anemia grade 3, 4 was also associated with reduced overall survival (HR, 4.1; P=0.014). After controlling for disease and treatment variables, grade 4 lymphopenia remained significantly associated with reduced overall survival (HR, 9.85; P=0.007). The association with grade 4 lymphopenia only remained significant in women of Hispanic ethnicity.
Conclusion
Severe lymphopenia was associated with reduced overall survival and progression-free survival in Hispanic women undergoing definitive chemoradiation for cervical cancer, but not associated with outcomes in non-Hispanic women.
Figure
Reference
-
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7–34.
Article2. Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N, et al. Cervical cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017; 28(suppl_4):iv72–83.
Article3. Yang T, Oh J, Apte A, Son CH, Deasy JO, Goodman KA. Predictors of hematologic toxicity during pelvic radiation therapy. Int J Radiat Oncol Biol Phys. 2012; 84(3):S346.
Article4. Abu-Rustum NR, Lee S, Correa A, Massad LS. Compliance with and acute hematologic toxic effects of chemoradiation in indigent women with cervical cancer. Gynecol Oncol. 2001; 81:88–91.
Article5. van Meir H, Nout RA, Welters MJ, Loof NM, de Kam ML, van Ham JJ, et al. Impact of (chemo)radiotherapy on immune cell composition and function in cervical cancer patients. Oncoimmunology. 2016; 6:e1267095.
Article6. Schrijvers D. Management of anemia in cancer patients: transfusions. Oncologist. 2011; 16(Suppl 3):12–8.
Article7. Berke G. The binding and lysis of target cells by cytotoxic lymphocytes: molecular and cellular aspects. Annu Rev Immunol. 1994; 12:735–73.
Article8. Clemente CG, Mihm MC Jr, Bufalino R, Zurrida S, Collini P, Cascinelli N. Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer. 1996; 77:1303–10.
Article9. Sato E, Olson SH, Ahn J, Bundy B, Nishikawa H, Qian F, et al. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc Natl Acad Sci U S A. 2005; 102:18538–43.10. Wu ES, Oduyebo T, Cobb LP, Cholakian D, Kong X, Fader AN, et al. Lymphopenia and its association with survival in patients with locally advanced cervical cancer. Gynecol Oncol. 2016; 140:76–82.
Article11. Wild AT, Herman JM, Dholakia AS, Moningi S, Lu Y, Rosati LM, et al. lymphocyte-sparing effect of stereotactic body radiation therapy in patients with unresectable pancreatic cancer. Int J Radiat Oncol Biol Phys. 2016; 94:571–9.
Article12. Cézé N, Thibault G, Goujon G, Viguier J, Watier H, Dorval E, et al. Pre-treatment lymphopenia as a prognostic biomarker in colorectal cancer patients receiving chemotherapy. Cancer Chemother Pharmacol. 2011; 68:1305–13.
Article13. Kitayama J, Yasuda K, Kawai K, Sunami E, Nagawa H. Circulating lymphocyte number has a positive association with tumor response in neoadjuvant chemoradiotherapy for advanced rectal cancer. Radiat Oncol. 2010; 5:47.
Article14. Schueneman AJ, Sugar EA, Uram J, Bigelow E, Herman JM, Edil BH, et al. Low total lymphocyte count is associated with poor survival in patients with resected pancreatic adenocarcinoma receiving a GM-CSF secreting pancreatic tumor vaccine. Ann Surg Oncol. 2013; 20(Suppl 3):S725–30.
Article15. Davuluri R, Jiang W, Fang P, Xu C, Komaki R, Gomez DR, et al. lymphocyte nadir and esophageal cancer survival outcomes after chemoradiation therapy. Int J Radiat Oncol Biol Phys. 2017; 99:128–35.
Article16. Cho O, Oh YT, Chun M, Noh OK, Hoe JS, Kim H. Minimum absolute lymphocyte count during radiotherapy as a new prognostic factor for nasopharyngeal cancer. Head Neck. 2016; 38(Suppl 1):E1061–7.
Article17. Campian JL, Ye X, Brock M, Grossman SA. Treatment-related lymphopenia in patients with stage III non-small-cell lung cancer. Cancer Invest. 2013; 31:183–8.
Article18. Groopman JE, Itri LM. Chemotherapy-induced anemia in adults: incidence and treatment. J Natl Cancer Inst. 1999; 91:1616–34.
Article19. Knight K, Wade S, Balducci L. Prevalence and outcomes of anemia in cancer: a systematic review of the literature. Am J Med. 2004; 116:Suppl 7A. 11S–26S.
Article20. Dunst J, Kuhnt T, Strauss HG, Krause U, Pelz T, Koelbl H, et al. Anemia in cervical cancers: impact on survival, patterns of relapse, and association with hypoxia and angiogenesis. Int J Radiat Oncol Biol Phys. 2003; 56:778–87.
Article21. Lim S, Lee CM, Park JM, Jung SY, Lee KB. An association between preoperative anemia and poor prognostic factors and decreased survival in early stage cervical cancer patients. Obstet Gynecol Sci. 2014; 57:471–7.
Article22. Rades D, Schild SE. Challenges of anemia correction during radiotherapy and chemoradiation. Eur Med Oncol. 2012; 5:35–8.
Article23. Koulis TA, Kornaga EN, Banerjee R, Phan T, Ghatage P, Magliocco AM, et al. Anemia, leukocytosis and thrombocytosis as prognostic factors in patients with cervical cancer treated with radical chemoradiotherapy: a retrospective cohort study. Clin Transl Radiat Oncol. 2017; 4:51–56.
Article24. Bishop AJ, Allen PK, Klopp AH, Meyer LA, Eifel PJ. Relationship between low hemoglobin levels and outcomes after treatment with radiation or chemoradiation in patients with cervical cancer: has the impact of anemia been overstated? Int J Radiat Oncol Biol Phys. 2015; 91:196–205.
Article25. Cho O, Chun M, Chang SJ, Oh YT, Noh OK. Prognostic Value of Severe Lymphopenia During Pelvic Concurrent Chemoradiotherapy in Cervical Cancer. Anticancer Res. 2016; 36:3541–7.26. Bogani G, Sabatucci I, Maltese G, Lecce F, Signorelli M, Martinelli F, et al. Chemotherapy-related leukopenia as a biomarker predicting survival outcomes in locally advanced cervical cancer. Eur J Obstet Gynecol Reprod Biol. 2017; 208:41–5.
Article27. Ray-Coquard I, Cropet C, Van Glabbeke M, Sebban C, Le Cesne A, Judson I, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 2009; 69:5383–91.
Article28. Fyles A, Keane TJ, Barton M, Simm J. The effect of treatment duration in the local control of cervix cancer. Radiother Oncol. 1992; 25:273–9.
Article29. Girinsky T, Rey A, Roche B, Haie C, Gerbaulet A, Randrianarivello H, et al. Overall treatment time in advanced cervical carcinomas: a critical parameter in treatment outcome. Int J Radiat Oncol Biol Phys. 1993; 27:1051–6.
Article30. Biewenga P, van der Velden J, Mol BW, Stalpers LJ, Schilthuis MS, van der Steeg JW, et al. Prognostic model for survival in patients with early stage cervical cancer. Cancer. 2011; 117:768–76.
Article31. Onal C, Yildirim BA, Guler OC, Mertsoylu H. The utility of pretreatment and posttreatment lymphopenia in cervical squamous cell carcinoma patients treated with definitive chemoradiotherapy. Int J Gynecol Cancer. 2018; 28:1553–59.
Article32. Taguchi A, Furusawa A, Ito K, Nakajima Y, Shimizuguchi T, Hara K, et al. Postradiotherapy persistent lymphopenia as a poor prognostic factor in patients with cervical cancer receiving radiotherapy: a single-center, retrospective study. Int J Clin Oncol. 2020; 25:955–62.
Article33. Azab B, Camacho-Rivera M, Taioli E. Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLoS One. 2014; 9:e112361.
Article34. Warnke C, Dehmel T, Ramanujam R, Holmen C, Nordin N, Wolfram K, et al. Initial lymphocyte count and low BMI may affect fingolimod-induced lymphopenia. Neurology. 2014; 83:2153–7.
Article35. Borges TC, Gomes TL, Pichard C, Laviano A, Pimentel GD. High neutrophil to lymphocytes ratio is associated with sarcopenia risk in hospitalized cancer patients. Clin Nutr. 2021; 40:202–6.
Article36. Lee AY, Golden DW, Bazan JG, Kopec M, Pelizzari CA, Aggarwal S, et al. Hematologic nadirs during chemoradiation for anal cancer: temporal characterization and dosimetric predictors. Int J Radiat Oncol Biol Phys. 2017; 97:306–12.
Article37. Sini C, Fiorino C, Perna L, Noris Chiorda B, Deantoni CL, Bianchi M, et al. Dose-volume effects for pelvic bone marrow in predicting hematological toxicity in prostate cancer radiotherapy with pelvic node irradiation. Radiother Oncol. 2016; 118:79–84.
Article38. Mell LK, Kochanski JD, Roeske JC, Haslam JJ, Mehta N, Yamada SD, et al. Dosimetric predictors of acute hematologic toxicity in cervical cancer patients treated with concurrent cisplatin and intensity-modulated pelvic radiotherapy. Int J Radiat Oncol Biol Phys. 2006; 66:1356–65.
Article39. Dyer BA, Zamarin D, Eskandar RN, Mayadev JM. Role of immunotherapy in the management of locally advanced and recurrent/metastatic cervical cancer. J Natl Compr Canc Netw. 2019; 17:91–7.
Article40. Ouh YT, Cho HW, Kim SM, Min KJ, Lee SH, Song JY, et al. Risk factors for type-specific persistence of high-risk human papillomavirus and residual/recurrent cervical intraepithelial neoplasia after surgical treatment. Obstet Gynecol Sci. 2020; 63:631–42.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Phase II Study of Consolidation Chemotherapy after Adjuvant or Primary Concurrent Chemoradiation Using Paclitaxel and Carboplatin to Treat High-Risk Early-Stage or Locally Advanced Cervical Cancer
- Concurrent chemotherapy and radiotherapy in invasive cervical cancer patients with high risk factors
- A case of primary retroperitoneal undifferentiated endometrial stromal sarcoma after concurrent chemoradiation therapy for cervical cancer
- Concurrent chemoradiation therapy in cervical cancer with para-aortic lymph node involvement
- Treatment of Cervical Cancer