Ann Hepatobiliary Pancreat Surg.
2022 Feb;26(1):69-75. 0000-0002-9045-2531.
Liver transplantation in pediatric patients with progressive familial intrahepatic cholestasis: Single center experience of seven cases
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2526834
- DOI: http://doi.org/0000-0002-9045-2531
Abstract
- Backgrounds/Aims
Progressive familial intrahepatic cholestasis (PFIC) is an autosomal recessive inherited disease requiring liver transplantation (LT). The objective of this study was to investigate the clinicopathological features and posttransplant courses of seven LT recipients with PFIC.
Methods
This was a retrospective single-center study of patients with PFIC who underwent LT from January 2013 to June 2020.
Results
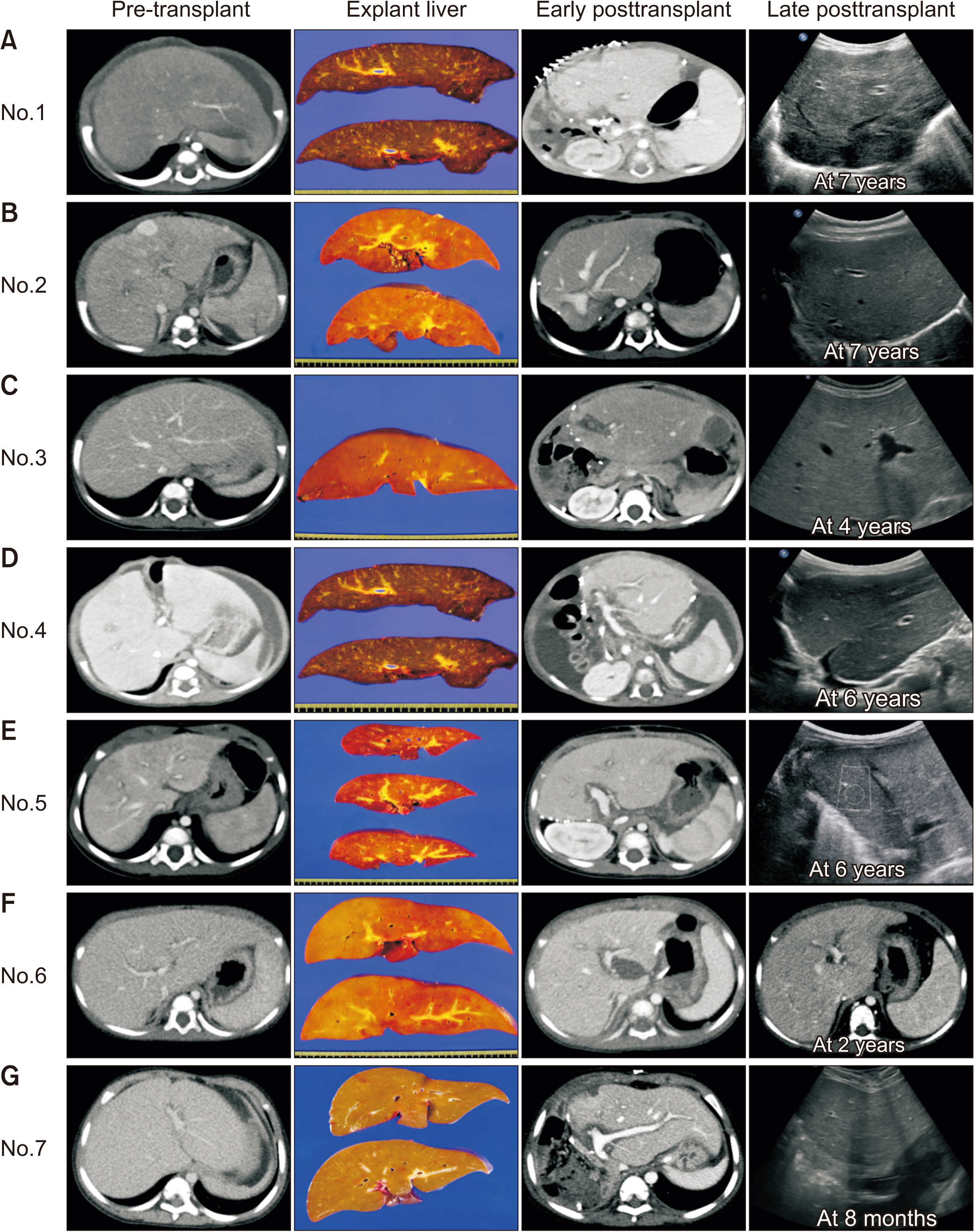
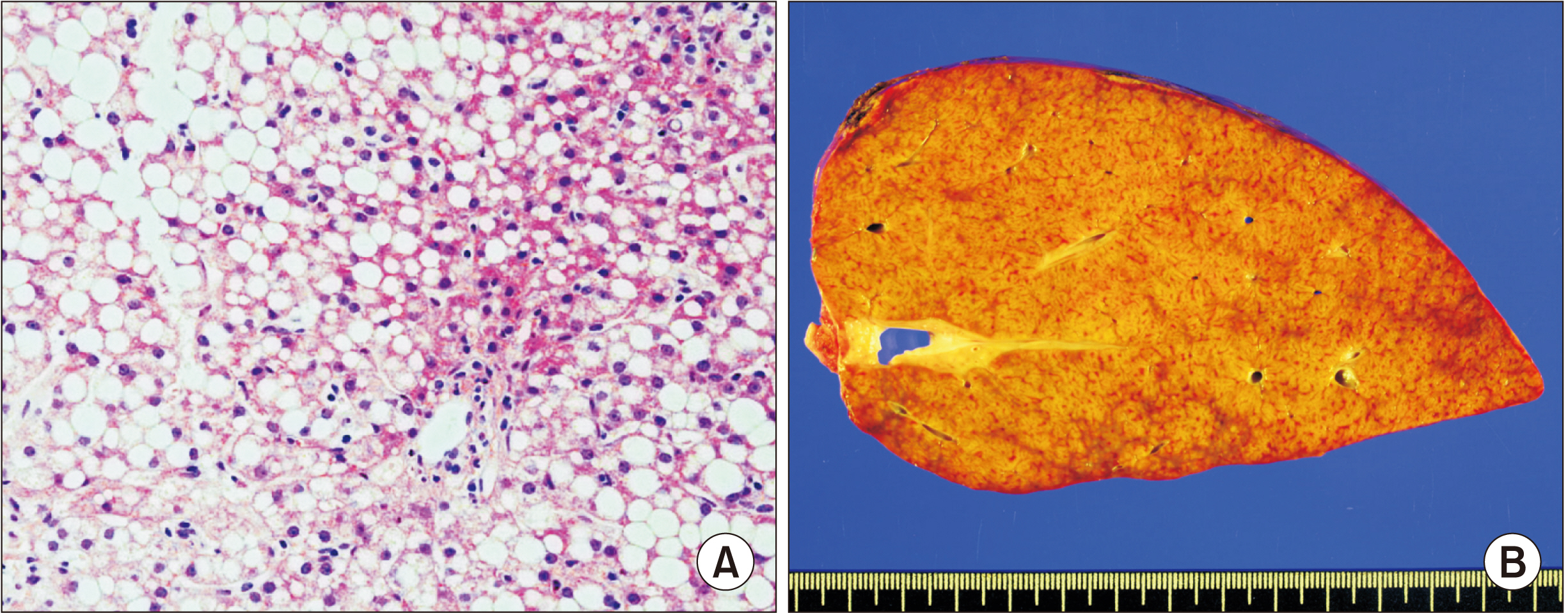
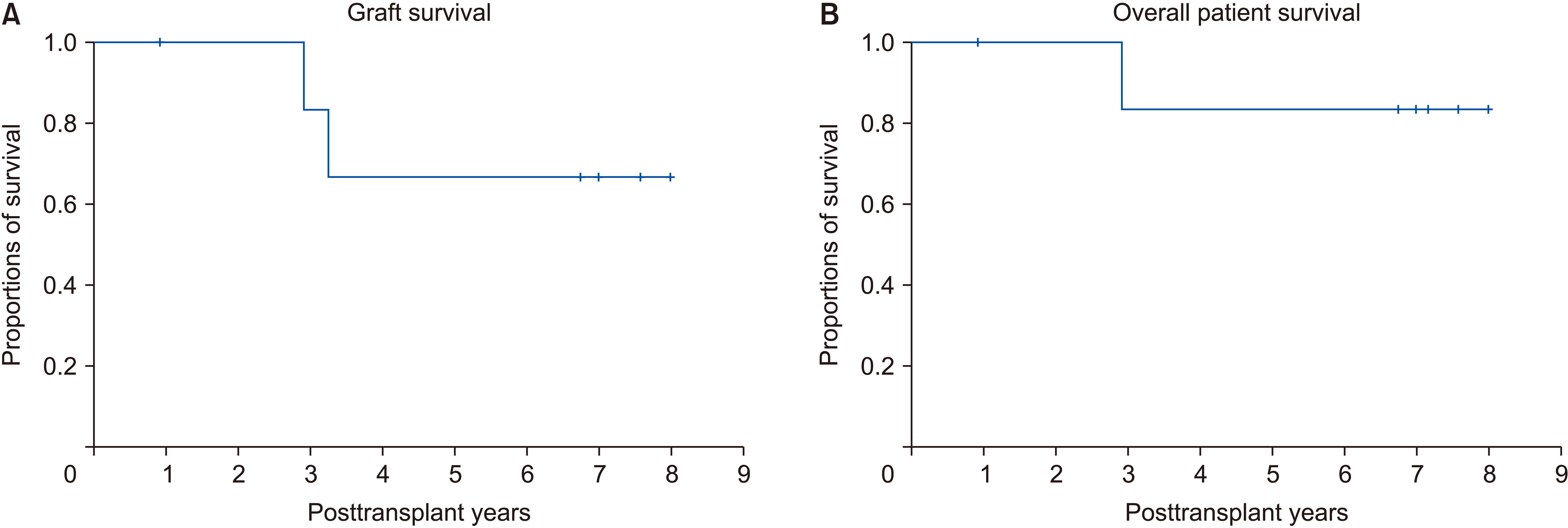
Two and five patients were diagnosed with PFIC type 1 and type 2, respectively. For all seven patients, age of PFIC onset was at birth. Jaundice was present in all cases. Mean pretransplant total and direct bilirubin levels were 16.1 ± 8.1 mg/dL and 12.4 ± 6.2 mg/dL, respectively. Median patient age and body weight at LT were 10 months and 7 kg, respectively. Types of donors were mothers of patients in four and deceased donors in three. All five patients with PFIC type 2 recovered uneventfully. One patient each with PFIC type 1 underwent retransplantation due to graft failure or died due to multi-organ failure. Overall graft and patient survival rates at five years were 66.7% and 83.3%, respectively. Bile salt export pump immunohistochemical staining showed normal canalicular expression in two patients with PFIC type 1, focal loss in two patients with PFIC type 2, and total loss in three patients with PFIC type 2.
Conclusions
LT is currently the only effective treatment for PFIC-associated end-stage liver diseases. It is mandatory to perform regular follow-up due to the risk of complications including steatohepatitis, especially for patients with PFIC type 1.
Figure
Reference
-
1. Nakanishi Y, Saxena R. 2015; Pathophysiology and diseases of the proximal pathways of the biliary system. Arch Pathol Lab Med. 139:858–866. DOI: 10.5858/arpa.2014-0229-RA. PMID: 26125426.
Article2. van Mil SW, Klomp LW, Bull LN, Houwen RH. 2001; FIC1 disease: a spectrum of intrahepatic cholestatic disorders. Semin Liver Dis. 21:535–544. DOI: 10.1055/s-2001-19034. PMID: 11745041.
Article3. de Vree JM, Jacquemin E, Sturm E, Cresteil D, Bosma PJ, Aten J, et al. 1998; Mutations in the MDR3 gene cause progressive familial intrahepatic cholestasis. Proc Natl Acad Sci U S A. 95:282–287. DOI: 10.1073/pnas.95.1.282. PMID: 9419367. PMCID: PMC18201.
Article4. Clayton RJ, Iber FL, Ruebner BH, McKusick VA. 1969; Byler disease. Fatal familial intrahepatic cholestasis in an Amish kindred. Am J Dis Child. 117:112–124. DOI: 10.1001/archpedi.1969.02100030114014. PMID: 5762004.5. Mehl A, Bohorquez H, Serrano MS, Galliano G, Reichman TW. 2016; Liver transplantation and the management of progressive familial intrahepatic cholestasis in children. World J Transplant. 6:278–290. DOI: 10.5500/wjt.v6.i2.278. PMID: 27358773. PMCID: PMC4919732.
Article6. Jacquemin E. 2012; Progressive familial intrahepatic cholestasis. Clin Res Hepatol Gastroenterol. 36 Suppl 1:S26–S35. DOI: 10.1016/S2210-7401(12)70018-9. PMID: 30236549.
Article7. Kang HJ, Hong SA, Oh SH, Kim KM, Yoo HW, Kim GH, et al. 2019; Progressive familial intrahepatic cholestasis in Korea: a clinicopathological study of five patients. J Pathol Transl Med. 53:253–260. DOI: 10.4132/jptm.2019.05.03. PMID: 31091858. PMCID: PMC6639708.
Article8. Namgoong JM, Hwang S, Song GW, Kim DY, Ha TY, Jung DH, et al. 2020; Pediatric liver transplantation with hyperreduced left lateral segment graft. Ann Hepatobiliary Pancreat Surg. 24:503–512. DOI: 10.14701/ahbps.2020.24.4.503. PMID: 33234754. PMCID: PMC7691208.
Article9. Namgoong JM, Hwang S, Ahn CS, Jung DH, Park GC. 2020; Side-to-side portal vein reconstruction for infant-to-infant deceased donor whole liver transplantation: report of 2 cases with video. Ann Hepatobiliary Pancreat Surg. 24:301–304. DOI: 10.14701/ahbps.2020.24.3.301. PMID: 32843595. PMCID: PMC7452795.
Article10. Rhee ES, Kim YB, Lee S, Oh SH, Lee BH, Kim KM, et al. 2019; Novel ATP8B1 gene mutations in a child with progressive familial intrahepatic cholestasis type 1. Pediatr Gastroenterol Hepatol Nutr. 22:479–486. DOI: 10.5223/pghn.2019.22.5.479. PMID: 31555573. PMCID: PMC6751104.
Article11. Aydogdu S, Cakir M, Arikan C, Tumgor G, Yuksekkaya HA, Yilmaz F, et al. 2007; Liver transplantation for progressive familial intrahepatic cholestasis: clinical and histopathological findings, outcome and impact on growth. Pediatr Transplant. 11:634–640. DOI: 10.1111/j.1399-3046.2007.00722.x. PMID: 17663686.
Article12. Liu Y, Sun LY, Zhu ZJ, Wei L, Qu W, Zeng ZG. 2018; Liver transplantation for progressive familial intrahepatic cholestasis. Ann Transplant. 23:666–673. DOI: 10.12659/AOT.909941. PMID: 30250015. PMCID: PMC6248029.
Article13. Davit-Spraul A, Gonzales E, Baussan C, Jacquemin E. 2009; Progressive familial intrahepatic cholestasis. Orphanet J Rare Dis. 4:1. DOI: 10.1186/1750-1172-4-1. PMID: 19133130. PMCID: PMC2647530.
Article14. Nemesánszky E, Lott JA. 1985; Gamma-glutamyltransferase and its isoenzymes: progress and problems. Clin Chem. 31:797–803. DOI: 10.1093/clinchem/31.6.797. PMID: 2859933.
Article15. Oude Elferink RP, Paulusma CC, Groen AK. 2006; Hepatocanalicular transport defects: pathophysiologic mechanisms of rare diseases. Gastroenterology. 130:908–925. DOI: 10.1053/j.gastro.2005.08.052. PMID: 16530529.
Article16. Klomp LW, Vargas JC, van Mil SW, Pawlikowska L, Strautnieks SS, van Eijk MJ, et al. 2004; Characterization of mutations in ATP8B1 associated with hereditary cholestasis. Hepatology. 40:27–38. DOI: 10.1002/hep.20285. PMID: 15239083.
Article17. Alissa FT, Jaffe R, Shneider BL. 2008; Update on progressive familial intrahepatic cholestasis. J Pediatr Gastroenterol Nutr. 46:241–252. DOI: 10.1097/MPG.0b013e3181596060. PMID: 18376240.
Article18. Liu LY, Wang XH, Wang ZL, Zhu QR, Wang JS. 2010; Characterization of ATP8B1 gene mutations and a hot-linked mutation found in Chinese children with progressive intrahepatic cholestasis and low GGT. J Pediatr Gastroenterol Nutr. 50:179–183. DOI: 10.1097/MPG.0b013e3181c1b368. PMID: 20038848.
Article19. Gonzales E, Spraul A, Jacquemin E. 2014; Clinical utility gene card for: progressive familial intrahepatic cholestasis type 2. Eur J Hum Genet. 22:572. DOI: 10.1038/ejhg.2013.187. PMID: 23982689. PMCID: PMC3953913.
Article20. Jacquemin E, Hermans D, Myara A, Habes D, Debray D, Hadchouel M, et al. 1997; Ursodeoxycholic acid therapy in pediatric patients with progressive familial intrahepatic cholestasis. Hepatology. 25:519–523. DOI: 10.1002/hep.510250303. PMID: 9049190.
Article21. Amer S, Hajira A. 2014; A comprehensive review of progressive familial intrahepatic cholestasis (PFIC): genetic disorders of hepatocanalicular transporters. Gastroenterology Res. 7:39–43. DOI: 10.14740/gr609e. PMID: 27785268. PMCID: PMC5051073.
Article22. Hori T, Egawa H, Miyagawa-Hayashino A, Yorifuji T, Yonekawa Y, Nguyen JH, et al. 2011; Living-donor liver transplantation for progressive familial intrahepatic cholestasis. World J Surg. 35:393–402. DOI: 10.1007/s00268-010-0869-6. PMID: 21125272.
Article23. Hori T, Egawa H, Takada Y, Ueda M, Oike F, Ogura Y, et al. 2011; Progressive familial intrahepatic cholestasis: a single-center experience of living-donor liver transplantation during two decades in Japan. Clin Transplant. 25:776–785. DOI: 10.1111/j.1399-0012.2010.01368.x. PMID: 21158920.
Article24. Englert C, Grabhorn E, Richter A, Rogiers X, Burdelski M, Ganschow R. 2007; Liver transplantation in children with progressive familial intrahepatic cholestasis. Transplantation. 84:1361–1363. DOI: 10.1097/01.tp.0000282869.94152.4f. PMID: 18049123.
Article25. Maggiore G, Gonzales E, Sciveres M, Redon MJ, Grosse B, Stieger B, et al. 2010; Relapsing features of bile salt export pump deficiency after liver transplantation in two patients with progressive familial intrahepatic cholestasis type 2. J Hepatol. 53:981–986. DOI: 10.1016/j.jhep.2010.05.025. PMID: 20800306.
Article26. Sindhi R, Rohan V, Bukowinski A, Tadros S, de Ville de Goyet J, Rapkin L, et al. 2020; Liver transplantation for pediatric liver cancer. Cancers (Basel). 12:720. DOI: 10.3390/cancers12030720. PMID: 32204368. PMCID: PMC7140094.
Article27. Namgoong JM, Hwang S, Kim DY, Ahn CS, Kwon H, Ha S, et al. Living donor liver transplantation in an infant patient with progressive familial intrahepatic cholestasis along with hepatocellular carcinoma: a case report. Korean J Transpl. https://doi.org/10.4285/kjt.21.0007 [in press]. DOI: 10.4285/kjt.21.0007. 2021.
Article28. Esquivel CO, Gutiérrez C, Cox KL, Garcia-Kennedy R, Berquist W, Concepcion W. 1994; Hepatocellular carcinoma and liver cell dysplasia in children with chronic liver disease. J Pediatr Surg. 29:1465–1469. DOI: 10.1016/0022-3468(94)90145-7. PMID: 7844722.
Article29. Brunati A, Feruzi Z, Sokal E, Smets F, Fervaille C, Gosseye S, et al. 2007; Early occurrence of hepatocellular carcinoma in biliary atresia treated by liver transplantation. Pediatr Transplant. 11:117–119. DOI: 10.1111/j.1399-3046.2006.00623.x. PMID: 17239135.
Article30. Iida T, Zendejas IR, Kayler LK, Magliocca JF, Kim RD, Hemming AW, et al. 2009; Hepatocellular carcinoma in a 10-month-old biliary atresia child. Pediatr Transplant. 13:1048–1049. DOI: 10.1111/j.1399-3046.2008.01094.x. PMID: 19032418.
Article31. Kim JM, Lee SK, Kwon CH, Joh JW, Choe YH, Park CK. 2012; Hepatocellular carcinoma in an infant with biliary atresia younger than 1 year. J Pediatr Surg. 47:819–821. DOI: 10.1016/j.jpedsurg.2012.01.020. PMID: 22498405.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Novel ATP8B1 Gene Mutations in a Child with Progressive Familial Intrahepatic Cholestasis Type 1
- Successful Use of Bortezomib for Recurrent Progressive Familial Intrahepatic Cholestasis Type II After Liver Transplantation: A Pediatric Case with a 9-Year Follow-Up
- Hepatocellular carcinoma associated with progressive intrahepatic familial cholestasis type 2: a case report
- Liver transplantation in pediatric patients with progressive familial intrahepatic cholestasis: single center experience of seven cases
- Early Diagnosis of ABCB11 Spectrum Liver Disorders by Next Generation Sequencing