Anesth Pain Med.
2022 Jan;17(1):35-43. 10.17085/apm.21055.
Comparison of bolus administration effects of lidocaine on preventing tourniquet-induced hypertension in patients undergoing general anesthesia: a randomized controlled trial
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kosin University College of Medicine, Busan, Korea
- 2Department of Anesthesiology and Pain Medicine, Ulsan University Hospital, Ulsan, Korea
- KMID: 2526525
- DOI: http://doi.org/10.17085/apm.21055
Abstract
- Background
This study assessed the effect of a single bolus administration of lidocaine on the prevention of tourniquet-induced hypertension (TIH) and compared the effect of lidocaine to that of ketamine in patients undergoing general anesthesia.
Methods
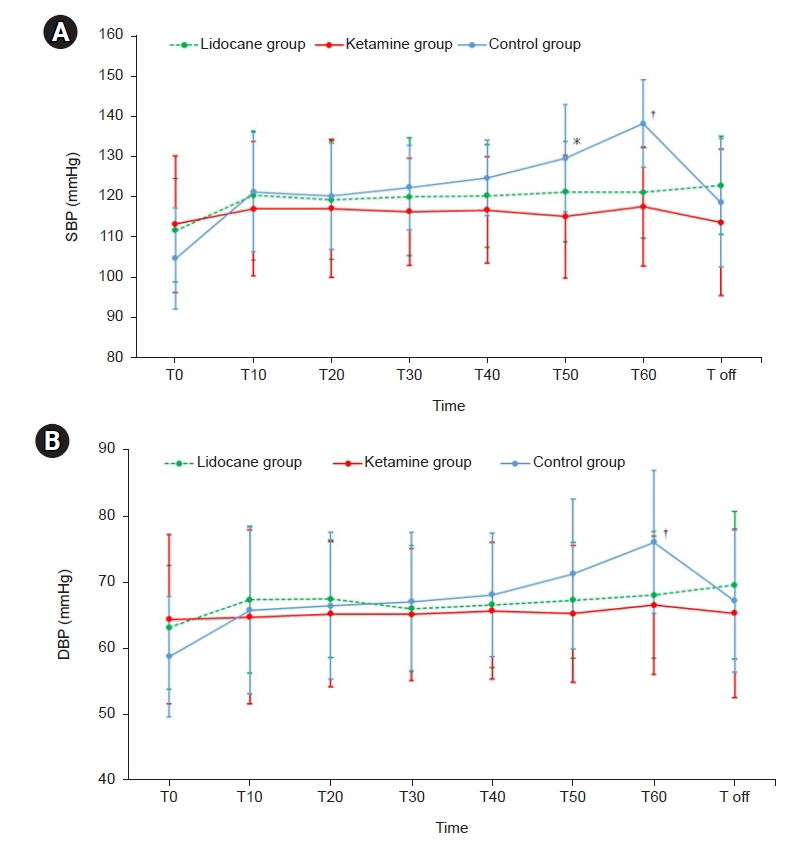
This randomized, controlled, double-blind study included 75 patients who underwent lower limb surgery using a tourniquet. The patients were administered lidocaine (1.5 mg/kg, n = 25), ketamine (0.2 mg/kg, n = 25) or placebo (n = 25). The study drugs were administered intravenously 10 min before tourniquet inflation. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were measured before tourniquet inflation, after tourniquet inflation for 60 min at 10 min intervals, and immediately after tourniquet deflation. The incidence of TIH, defined as an increase of 30% or more in SBP or DBP during tourniquet inflation, was also recorded.
Results
SBP, DBP, and HR increased significantly over time in the control group compared to those in the lidocaine and ketamine groups for 60 min after tourniquet inflation (P < 0.001, P < 0.001, and P = 0.007, respectively). The incidence of TIH was significantly lower in the lidocaine (n = 4, 16%) and ketamine (n = 3, 12%) group than in the control group (n = 14, 56%) (P = 0.001).
Conclusion
Single-bolus lidocaine effectively attenuated blood pressure increase due to tourniquet inflation, with an effect comparable to that of bolus ketamine.
Keyword
Figure
Reference
-
1. Kumar K, Railton C, Tawfic Q. Tourniquet application during anesthesia: "what we need to know?". J Anaesthesiol Clin Pharmacol. 2016; 32:424–30.2. Kam PC, Kavanagh R, Yoong FF. The arterial tourniquet: pathophysiological consequences and anaesthetic implications. Anaesthesia. 2001; 56:534–45.3. Kaufman RD, Walts LF. Tourniquet-induced hypertension. Br J Anaesth. 1982; 54:333–6.4. Valli H, Rosenberg PH, Kyttä J, Nurminen M. Arterial hypertension associated with the use of a tourniquet with either general or regional anaesthesia. Acta Anaesthesiol Scand. 1987; 31:279–83.5. Girardis M, Milesi S, Donato S, Raffaelli M, Spasiano A, Antonutto G, et al. The hemodynamic and metabolic effects of tourniquet application during knee surgery. Anesth Analg. 2000; 91:727–31.6. Chabel C, Russell LC, Lee R. Tourniquet-induced limb ischemia: a neurophysiologic animal model. Anesthesiology. 1990; 72:1038–44.7. MacIver MB, Tanelian DL. Activation of C fibers by metabolic perturbations associated with tourniquet ischemia. Anesthesiology. 1992; 76:617–23.8. Woolf CJ, Thompson SWN. The induction and maintenance of central sensitization is dependent on N-methyl-D-aspartic acid receptor activation; implications for the treatment of post-injury pain hypersensitivity states. Pain. 1991; 44:293–9.9. Tetzlaff JE, O'Hara J Jr, Yoon HJ, Schubert A. Tourniquet-induced hypertension correlates with autonomic nervous system changes detected by power spectral heart rate analysis. J Clin Anesth. 1997; 9:138–42.10. El-Sayed W, Hasanein R. Intraoperative lidocaine infusion attenuates tourniquet induced hypertension in patients undergoing anterior cruciate ligament reconstruction under general anesthesia. Egypt J Anaesth. 2016; 32:345–50.11. Zaidi R, Ahmed A. Comparison of ketorolac and low-dose ketamine in preventing tourniquet-induced increase in arterial pressure. Indian J Anaesth. 2015; 59:428–32.12. Shinoda T, Murakami W, Takamichi Y, Iizuka H, Tanaka M, Kuwasako Y. Effect of remifentanil infusion rate on stress response in orthopedic surgery using a tourniquet application. BMC Anesthesiol. 2013; 13:14.13. Li YH, Wang YQ, Zhang YJ, Zheng DY, Hu L, Tian ML. Influence of Dexmedetomidine on the tourniquet related responses in hypertension patients receiving unilateral knee arthroplasty under general anesthesia. J Arthroplasty. 2015; 30:1359–63.14. Satsumae T, Yamaguchi H, Sakaguchi M, Yasunaga T, Yamashita S, Yamamoto S, et al. Preoperative small-dose ketamine prevented tourniquet-induced arterial pressure increase in orthopedic patients under general anesthesia. Anesth Analg. 2001; 92:1286–9.15. Park JW, Jung YH, Baek CW, Kang H, Cha SM. Effects of low dose ketamine on tourniquet-induced haemodynamic responses during general anaesthesia. J Int Med Res. 2007; 35:600–8.16. Hermanns H, Hollmann MW, Stevens MF, Lirk P, Brandenburger T, Piegeler T, et al. Molecular mechanisms of action of systemic lidocaine in acute and chronic pain: a narrative review. Br J Anaesth. 2019; 123:335–49.17. Gholipour Baradari A, Firouzian A, Hasanzadeh Kiabi F, Emami Zeydi A, Khademloo M, Nazari Z, et al. Bolus administration of intravenous lidocaine reduces pain after an elective caesarean section: findings from a randomised, double-blind, placebo-controlled trial. J Obstet Gynaecol. 2017; 37:566–70.18. Koppert W, Weigand M, Neumann F, Sittl R, Schuettler J, Schmelz M, et al. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004; 98:1050–5.19. Takada M, Fukusaki M, Terao Y, Kanaide M, Yamashita K, Matsumoto S, et al. Preadministration of low-dose ketamine reduces tourniquet pain in healthy volunteers. J Anesth. 2005; 19:180–2.20. Yardeni IZ, Beilin B, Mayburd E, Levinson Y, Bessler H. The effect of perioperative intravenous lidocaine on postoperative pain and immune function. Anesth Analg. 2009; 109:1464–9.21. Fiorelli A, Mazzella A, Passavanti B, Sansone P, Chiodini P, Iannotti M, et al. Is pre-emptive administration of ketamine a significant adjunction to intravenous morphine analgesia for controlling postoperative pain? A randomized, double-blind, placebo-controlled clinical trial. Interact Cardiovasc Thorac Surg. 2015; 21:284–90.22. Yang L, Zhang J, Zhang Z, Zhang C, Zhao D, Li J. Preemptive analgesia effects of ketamine in patients undergoing surgery. A meta-analysis. Acta Cir Bras. 2014; 29:819–25.23. Murthy Tk K, Kumar Pv V. Effect of perioperative intravenous lignocaine infusion on haemodynamic responses and postoperative analgesia in laparoscopic cholecystectomy surgeries. Anesth Pain Med. 2018; 8:e63490.24. Weale NK, Rogers CA, Cooper R, Nolan J, Wolf AR. Effect of remifentanil infusion rate on stress response to the pre-bypass phase of paediatric cardiac surgery. Br J Anaesth. 2004; 92:187–94.25. Scott LJ, Perry CM. Remifentanil: a review of its use during the induction and maintenance of general anaesthesia. Drugs. 2005; 65:1793–823.26. Jung JY, Han JH, Yi JW, Kang JM. Remifentanil prevents tourniquet-induced arterial pressure increase in elderly orthopedic patients under sevoflurane/N2O general anesthesia. Int J Med Sci. 2012; 9:311–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Intravenous Lidocaine on Cardiovascular Changes by the use of Tourniquet under Anesthesia
- The Effects of Lidocaine Infiltration in the Tourniquet Site on Blood Pressure and Heart Rate
- Effects of Four Anesthesia Methods and Tourniquet Durations on Tourniquet Induced Hypertension during Total Knee Arthroplasty
- Prevention of pain with the injection of microemulsion propofol: a comparison of a combination of lidocaine and ketamine with lidocaine or ketamine alone
- Wide-Awake Hand Surgery