J Stroke.
2022 Jan;24(1):128-137. 10.5853/jos.2021.02082.
Bridging Thrombolysis versus Direct Mechanical Thrombectomy in Stroke Due to Basilar Artery Occlusion
- Affiliations
-
- 1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
- 2Division of Neurology, Department of Medicine, National University Health System, Singapore
- 3Bristol Medical School, University of Bristol, Bristol, UK
- 4Division of Interventional Radiology, Department of Diagnostic Imaging, National University Health System, Singapore
- 5Department of Interventional Neuroradiology, The Royal London Hospital, Barts NHS Trust, London, UK
- 6Stroke Department, The Royal London Hospital, Barts NHS Trust, London, UK
- 7Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 8Department of Diagnostic and Interventional Neuroradiology, Hospital Bremen-Mitte, Bremen, Germany
- 9First Department of Radiology, School of Medicine, National & Kapodistrian University of Athens, Athens, Greece
- 10Department of Neurology, Hospital Bremen-Mitte, Bremen, Germany
- 11Department of Neuroradiology, University Hospital Magdeburg, Magdeburg, Germany
- 12Institute of Diagnostic and Interventional Radiology, Neuroradiology and Nuclear Medicine, University Hospital Knappschaftskrankenhaus Bochum, Bochum, Germany
- 13Department of Neuroradiology, Karolinska University Hospital, Stockholm, Sweden
- 14Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
- 15Department of Medical Imaging, AZ Groeninge, Kortrijk, Belgium
- 16Department of Neurology, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
- KMID: 2525338
- DOI: http://doi.org/10.5853/jos.2021.02082
Abstract
- Background and Purpose
Mechanical thrombectomy (MT) is an effective treatment for patients with basilar artery occlusion (BAO) acute ischemic stroke. It remains unclear whether bridging intravenous thrombolysis (IVT) prior to MT confers any benefit. This study compared the outcomes of acute BAO patients who were treated with direct MT versus combined IVT plus MT.
Methods
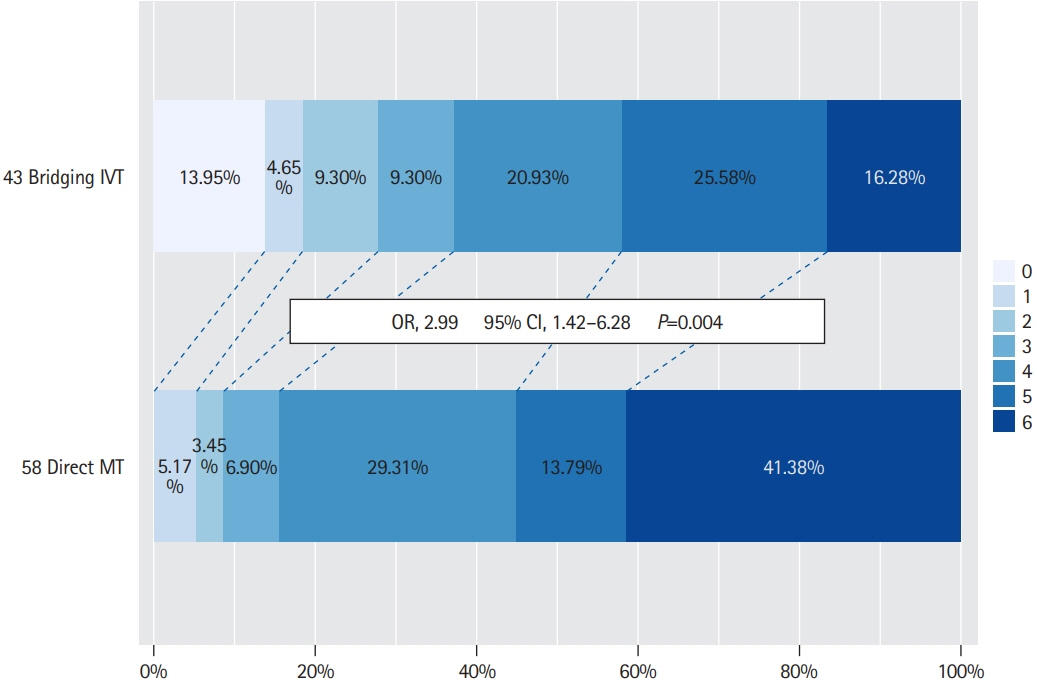
This multicenter retrospective cohort study included patients who were treated for acute BAO from eight comprehensive stroke centers between January 2015 and December 2019. Patients received direct MT or combined bridging IVT plus MT. Primary outcome was favorable functional outcome defined as modified Rankin Scale 0–3 measured at 90 days. Secondary outcome measures included mortality and symptomatic intracranial hemorrhage (sICH).
Results
Among 322 patients, 127 (39.4%) patients underwent bridging IVT followed by MT and 195 (60.6%) underwent direct MT. The mean±standard deviation age was 67.5±14.1 years, 64.0% were male and median National Institutes of Health Stroke Scale was 16 (interquartile range, 8 to 25). At 90-day, the rate of favorable functional outcome was similar between the bridging IVT and direct MT groups (39.4% vs. 34.4%, P=0.361). On multivariable analyses, bridging IVT was not asComorbidisociated with favorable functional outcome, mortality or sICH. In subgroup analyses, patients with underlying atherosclerosis treated with bridging IVT compared to direct MT had a higher rate of favorable functional outcome at 90 days (37.2% vs. 15.5%, P=0.013).
Conclusions
Functional outcomes were similar in BAO patients treated with bridging IVT versus direct MT. In the subgroup of patients with underlying large-artery atherosclerosis stroke mechanism, bridging IVT may potentially confer benefit and this warrants further investigation.
Figure
Reference
-
References
1. Lindsberg PJ, Mattle HP. Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke. 2006; 37:922–928.2. Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ. Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry. 2005; 76:1238–1241.
Article3. Baird TA, Muir KW, Bone I. Basilar artery occlusion. Neurocrit Care. 2004; 1:319–329.
Article4. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.5. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.
Article6. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.7. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article8. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article9. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.
Article10. Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring HP, Trenkler J, et al. Mechanical recanalization in basilar artery occlusion: the ENDOSTROKE study. Ann Neurol. 2015; 77:415–424.
Article11. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.12. Katsanos AH, Malhotra K, Goyal N, Arthur A, Schellinger PD, Köhrmann M, et al. Intravenous thrombolysis prior to mechanical thrombectomy in large vessel occlusions. Ann Neurol. 2019; 86:395–406.
Article13. Mazighi M, Meseguer E, Labreuche J, Amarenco P. Bridging therapy in acute ischemic stroke: a systematic review and meta-analysis. Stroke. 2012; 43:1302–1308.14. Mazighi M, Serfaty JM, Labreuche J, Laissy JP, Meseguer E, Lavallée PC, et al. Comparison of intravenous alteplase with a combined intravenous-endovascular approach in patients with stroke and confirmed arterial occlusion (RECANALISE study): a prospective cohort study. Lancet Neurol. 2009; 8:802–809.
Article15. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO)-European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischaemic stroke: endorsed by Stroke Alliance for Europe (SAFE). Eur Stroke J. 2019; 4:6–12.16. Desilles JP, Loyau S, Syvannarath V, Gonzalez-Valcarcel J, Cantier M, Louedec L, et al. Alteplase reduces downstream microvascular thrombosis and improves the benefit of large artery recanalization in stroke. Stroke. 2015; 46:3241–3248.
Article17. Seners P, Turc G, Maïer B, Mas JL, Oppenheim C, Baron JC. Incidence and predictors of early recanalization after intravenous thrombolysis: a systematic review and meta-analysis. Stroke. 2016; 47:2409–2412.18. Tsivgoulis G, Katsanos AH, Schellinger PD, Köhrmann M, Varelas P, Magoufis G, et al. Successful reperfusion with intravenous thrombolysis preceding mechanical thrombectomy in large-vessel occlusions. Stroke. 2018; 49:232–235.
Article19. Abilleira S, Ribera A, Cardona P, Rubiera M, López-Cancio E, Amaro S, et al. Outcomes after direct thrombectomy or combined intravenous and endovascular treatment are not different. Stroke. 2017; 48:375–378.
Article20. Bellwald S, Weber R, Dobrocky T, Nordmeyer H, Jung S, Hadisurya J, et al. Direct mechanical intervention versus bridging therapy in stroke patients eligible for intravenous thrombolysis: a pooled analysis of 2 registries. Stroke. 2017; 48:3282–3288.21. Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Clark W, Dávalos A, et al. Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the SWIFT and STAR studies. JAMA Neurol. 2017; 74:268–274.22. Kaesmacher J, Mordasini P, Arnold M, López-Cancio E, Cerdá N, Boeckh-Behrens T, et al. Direct mechanical thrombectomy in tPA-ineligible and -eligible patients versus the bridging approach: a meta-analysis. J Neurointerv Surg. 2019; 11:20–27.
Article23. Maingard J, Shvarts Y, Motyer R, Thijs V, Brennan P, O’Hare A, et al. Outcomes of endovascular thrombectomy with and without bridging thrombolysis for acute large vessel occlusion ischaemic stroke. Intern Med J. 2019; 49:345–351.
Article24. Seners P, Dargazanli C, Piotin M, Sablot D, Bracard S, Niclot P, et al. Intended bridging therapy or intravenous thrombolysis alone in minor stroke with basilar artery occlusion. Stroke. 2021; 52:699–702.
Article25. Mistry EA, Mistry AM, Nakawah MO, Chitale RV, James RF, Volpi JJ, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients: a meta-analysis. Stroke. 2017; 48:2450–2456.
Article26. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article27. Sparaco M. Basilar artery occlusion: clinical management and therapy. Clin Manag Issues. 2018; 12:67–76.
Article28. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial: TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article29. Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, et al. Modified thrombolysis in cerebral infarction 2C/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy: insights from the ASTER Trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization). Stroke. 2018; 49:1189–1196.30. Jansen IG, Mulder MJ, Goldhoorn RB; MR CLEAN Registry investigators. Endovascular treatment for acute ischaemic stroke in routine clinical practice: prospective, observational cohort study (MR CLEAN Registry). BMJ. 2018; 360:k949.
Article31. Wahlgren N, Ahmed N, Dávalos A, Hacke W, Millán M, Muir K, et al. Thrombolysis with alteplase 3-4.5 h after acute ischaemic stroke (SITS-ISTR): an observational study. Lancet. 2008; 372:1303–1309.
Article32. Schonewille W. A randomized acute stroke trial of endovascular therapy in acute basilar artery occlusion. European Stroke Organisation (ESO)-World Stroke Organization (WSO). 2020 Nov 7-9; Webinar. https://eso-wso-conference.org/eso-wso-may-webinar.33. Writing Group for the BASILAR Group, Zi W, Qiu Z, Wu D, Li F, Liu H, et al. Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry. JAMA Neurol. 2020; 77:561–573.34. Fischer U, Kaesmacher J, Mendes Pereira V, Chapot R, Siddiqui AH, Froehler MT, et al. Direct mechanical thrombectomy versus combined intravenous and mechanical thrombectomy in large-artery anterior circulation stroke: a topical review. Stroke. 2017; 48:2912–2918.35. Riedel CH, Zimmermann P, Jensen-Kondering U, Stingele R, Deuschl G, Jansen O. The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke. 2011; 42:1775–1777.36. Sun X, Tong X, Gao F, Lao H, Miao Z. Endovascular treatment for acute basilar artery occlusion: a single center retrospective observational study. BMC Neurol. 2019; 19:315.
Article37. Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. 2020; 382:1981–1993.
Article38. Suzuki K, Matsumaru Y, Takeuchi M, Morimoto M, Kanazawa R, Takayama Y, et al. Effect of mechanical thrombectomy without vs with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke: the SKIP randomized clinical trial. JAMA. 2021; 325:244–253.39. Zi W, Qiu Z, Li F, Sang H, Wu D, Luo W, et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: the DEVT randomized clinical trial. JAMA. 2021; 325:234–243.40. Treurniet KM, LeCouffe NE, Kappelhof M, Emmer BJ, van Es AC, Boiten J, et al. MR CLEAN-NO IV: intravenous treatment followed by endovascular treatment versus direct endovascular treatment for acute ischemic stroke caused by a proximal intracranial occlusion-study protocol for a randomized clinical trial. Trials. 2021; 22:141.
Article41. Bridging Thrombolysis Versus Direct Mechanical Thrombectomy in Acute Ischemic Stroke (SWIFT DIRECT). ClinicalTrials. gov. https://clinicaltrials.gov/ct2/show/NCT03192332. 2021. Accessed November 4, 2021.42. DIRECT-SAFE: A Randomized Controlled Trial of DIRECT Endovascular Clot Retrieval Versus Standard Bridging Thrombolysis With Endovascular Clot Retrieval. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03494920. 2021. Accessed November 4, 2021.43. Chalos V, LeCouffe NE, Uyttenboogaart M, Lingsma HF, Mulder MJHL, Venema E, et al. Endovascular treatment with or without prior intravenous alteplase for acute ischemic stroke. J Am Heart Assoc. 2019; 8:e011592.44. Malhotra K, Liebeskind DS. Collaterals in ischemic stroke. Brain Hemorrhages. 2020; 1:6–12.
Article45. Haussen DC, Bouslama M, Dehkharghanii S, Bowen M, Fag- gard J, Grossberg JA, et al. Enhanced collaterals in patients with large vessel stroke from intracranial atherosclerosis: an automated CT perfusion-based study. Stroke. 2017; 48(Suppl 1):AWMP23.
Article46. Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Turan TN, Cloft HJ, et al. Collaterals dramatically alter stroke risk in intracranial atherosclerosis. Ann Neurol. 2011; 69:963–974.
Article47. Maus V, Kalkan A, Kabbasch C, Abdullayev N, Stetefeld H, Barnikol UB, et al. Mechanical thrombectomy in basilar artery occlusion: presence of bilateral posterior communicating arteries is a predictor of favorable clinical outcome. Clin Neuroradiol. 2019; 29:153–160.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- DIRECT-SAFE: A Randomized Controlled Trial of DIRECT Endovascular Clot Retrieval versus Standard Bridging Therapy
- Dual Mechanical Thrombectomy for Recanalization of a Resistant Acute Posterior Circulation Stroke
- Mechanical Thrombectomy for Acute Ischemic Stroke with Middle Cerebral Artery Occlusion in 11-year-old Patient
- Endovascular Therapy for Acute Basilar Artery Occlusion: Comparison between Patients with and without Underlying Intracranial Atherosclerotic Stenosis
- The Limitations of Thrombectomy with Solitaire(TM) AB as First-line Treatment in Acute Ischemic Stroke: A Single Center Experience