Acute Crit Care.
2021 Nov;36(4):322-331. 10.4266/acc.2021.00276.
Bleeding complications associated with the molecular adsorbent recirculating system: a retrospective study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea
- 2Research Institute of Clinical Medicine of Jeonbuk National University-Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea
- 3Humidifier Disinfectant Health Center, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea
- 4Division of Respiratory and Critical Care Medicine, Department of Internal Medicine, Research Center for Pulmonary Disorders, Jeonbuk National University Hospital, Jeonbuk National University Medical School, Jeonju, Korea
- KMID: 2524315
- DOI: http://doi.org/10.4266/acc.2021.00276
Abstract
- Background
The molecular adsorbent recirculating system (MARS) is a hepatic replacement system that supports excretory liver function in patients with liver failure. However, since MARS has been employed in our hospital, bleeding complications have occurred in many patients during or after MARS. The objective of this study was to determine how MARS affects coagulopathy and identify specific factors associated with bleeding complications.
Methods
We retrospectively analyzed data from 17 patients undergoing a total of 41 MARS sessions. Complete blood count, coagulation profiles, and blood chemistry values were compared before and after MARS. To identify pre-MARS factors associated with increased bleeding after MARS, we divided patients into bleeder and non-bleeder groups and compared their pre-MARS laboratory values.
Results
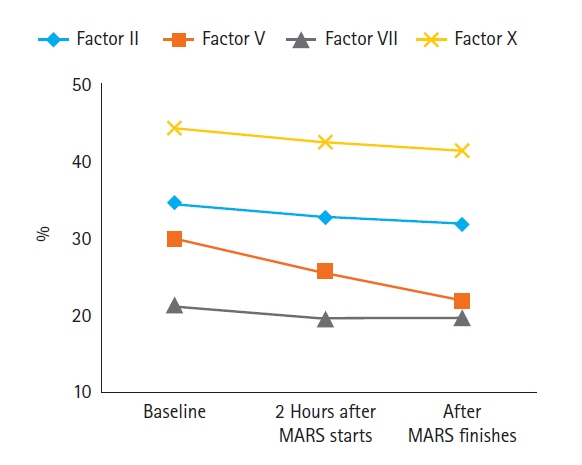
MARS significantly reduced bilirubin and creatinine levels. MARS also increased prothrombin time and reduced platelet and fibrinogen, thus negatively impacting coagulation. Pre-MARS hemoglobin was significantly lower in the bleeder group than in the non-bleeder group (P=0.015). When comparing the upper and lower 33% of MARS sessions based on the hemoglobin reduction rate, hemoglobin reduction was significantly greater in MARS sessions involving patients with low pre-MARS international normalized ratio of prothrombin time (PT-INR) and factor V (P=0.038 and P=0.023, respectively).
Conclusions
MARS could appears to alter coagulation-related factors such as factor V and increase the risk of bleeding complications particularly in patient with low hemoglobin. However, individual differences among patients were large, and various factors, such as low hemoglobin, PT-INR, and factor V levels, appear to be involved.
Keyword
Figure
Reference
-
1. Nanchal R, Subramanian R, Karvellas CJ, Hollenberg SM, Peppard WJ, Singbartl K, et al. Guidelines for the management of adult acute and acute-on-chronic liver failure in the ICU: cardiovascular, endocrine, hematologic, pulmonary and renal considerations: executive summary. Crit Care Med. 2020; 48:415–9.2. Lim YS. Acute liver failure in Korea: etiology, prognosis and treatment. Korean J Hepatol. 2010; 16:5–18.
Article3. Gerth HU, Pohlen M, Thölking G, Pavenstädt H, Brand M, Hüsing-Kabar A, et al. Molecular adsorbent recirculating system can reduce short-term mortality among patients with acute-on-chronic liver failure-a retrospective analysis. Crit Care Med. 2017; 45:1616–24.
Article4. Choi JW, Yoon KT, Park JY, Kim JK, Ahn SH, Paik YH, et al. Usefulness and safety of extracorporeal liver support therapy using MARSR for patients with liver failure: a preliminary report. Korean J Gastroenterol. 2009; 54:28–35.5. Vaid A, Chweich H, Balk EM, Jaber BL. Molecular adsorbent recirculating system as artificial support therapy for liver failure: a meta-analysis. ASAIO J. 2012; 58:51–9.6. Saliba F. The Molecular Adsorbent Recirculating System (MARS) in the intensive care unit: a rescue therapy for patients with hepatic failure. Crit Care. 2006; 10:118.7. Bañares R, Ibáñez-Samaniego L, Torner JM, Pavesi M, Olmedo C, Catalina MV, et al. Meta-analysis of individual patient data of albumin dialysis in acute-on-chronic liver failure: focus on treatment intensity. Therap Adv Gastroenterol. 2019; 12:1756284819879565.
Article8. He GL, Feng L, Duan CY, Hu X, Zhou CJ, Cheng Y, et al. Meta-analysis of survival with the molecular adsorbent recirculating system for liver failure. Int J Clin Exp Med. 2015; 8:17046–54.9. Khuroo MS, Khuroo MS, Farahat KL. Molecular adsorbent recirculating system for acute and acute-on-chronic liver failure: a meta-analysis. Liver Transpl. 2004; 10:1099–106.
Article10. Stravitz RT, Ellerbe C, Durkalski V, Schilsky M, Fontana RJ, Peterseim C, et al. Bleeding complications in acute liver failure. Hepatology. 2018; 67:1931–42.
Article11. Boyle M, Kurtovic J, Bihari D, Riordan S, Steiner C. Equipment review: the molecular adsorbents recirculating system (MARS). Crit Care. 2004; 8:280–6.12. Jalan R, Sen S, Williams R. Prospects for extracorporeal liver support. Gut. 2004; 53:890–8.
Article13. Duga S, Asselta R, Tenchini ML. Coagulation factor V. Int J Biochem Cell Biol. 2004; 36:1393–9.
Article14. Izumi S, Langley PG, Wendon J, Ellis AJ, Pernambuco RB, Hughes RD, et al. Coagulation factor V levels as a prognostic indicator in fulminant hepatic failure. Hepatology. 1996; 23:1507–11.
Article15. Bernuau J, Goudeau A, Poynard T, Dubois F, Lesage G, Yvonnet B, et al. Multivariate analysis of prognostic factors in fulminant hepatitis B. Hepatology. 1986; 6:648–51.
Article16. Ichai P, Laurent-Bellue A, Saliba F, Moreau D, Besch C, Francoz C, et al. Acute liver failure/injury related to drug reaction with eosinophilia and systemic symptoms: outcomes and prognostic factors. Transplantation. 2017; 101:1830–7.17. Zulian MC, Chedid MF, Chedid AD, Grezzana Filho TJ, Leipnitz I, de Araujo A, et al. Low serum factor V level: early predictor of allograft failure and death following liver transplantation. Langenbecks Arch Surg. 2015; 400:589–97.
Article18. Elinav E, Ben-Dov I, Hai-Am E, Ackerman Z, Ofran Y. The predictive value of admission and follow up factor V and VII levels in patients with acute hepatitis and coagulopathy. J Hepatol. 2005; 42:82–6.
Article19. Alshamsi F, Alshammari K, Belley-Cote E, Dionne J, Albrahim T, Albudoor B, et al. Extracorporeal liver support in patients with liver failure: a systematic review and meta-analysis of randomized trials. Intensive Care Med. 2020; 46:1–16.
Article20. Kim Y, Kim CK, Jung S, Ko SB. Brain oxygen monitoring via jugular venous oxygen saturation in a patient with fulminant hepatic failure. Korean J Crit Care Med. 2016; 31:251–5.
Article21. Ha SJ, Hwang YJ, Lim DG. Hemodynamic changes during isolated liver hemoperfusion of hepatoma. Korean J Crit Care Med. 2004; 19:115–20.22. Faybik P, Bacher A, Kozek-Langenecker SA, Steltzer H, Krenn CG, Unger S, et al. Molecular adsorbent recirculating system and hemostasis in patients at high risk of bleeding: an observational study. Crit Care. 2006; 10:R24.23. Doria C, Mandalà L, Smith JD, Caruana G, Scott VL, Gruttadauria S, et al. Thromboelastography used to assess coagulation during treatment with molecular adsorbent recirculating system. Clin Transplant. 2004; 18:365–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of the Molecular Adsorbent Recirculating System in Acute Fatty Liver of Pregnancy: a Case Report
- Two adolescent cases of early use of Molecular Adsorbent Recirculating System® for drug-induced fulminant hepatic failure
- Usefulness and Safety of Extracorporeal Liver Support Therapy Using MARS(R) for Patients with Liver Failure: A Preliminary Report
- A Case of Acute Hepatic Failure due to Acetaminophen Overdose Treated with Molecular Adsorbents Recirculating System(R)
- Albumin for End-Stage Liver Disease