J Neurocrit Care.
2021 Dec;14(2):103-108. 10.18700/jnc.210028.
Successful treatment with rituximab in a patient with lupus cerebritis and posterior reversible encephalopathy syndrome: a case report
- Affiliations
-
- 1Department of Neurology, Hanyang University Hospital, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2523720
- DOI: http://doi.org/10.18700/jnc.210028
Abstract
- Background
Neuropsychiatric systemic lupus erythematosus (NPSLE) has a diverse and broad spectrum of severity and prognosis, with some devastating manifestations. However, its diagnosis and treatment remain unclear and controversial.
Case Report
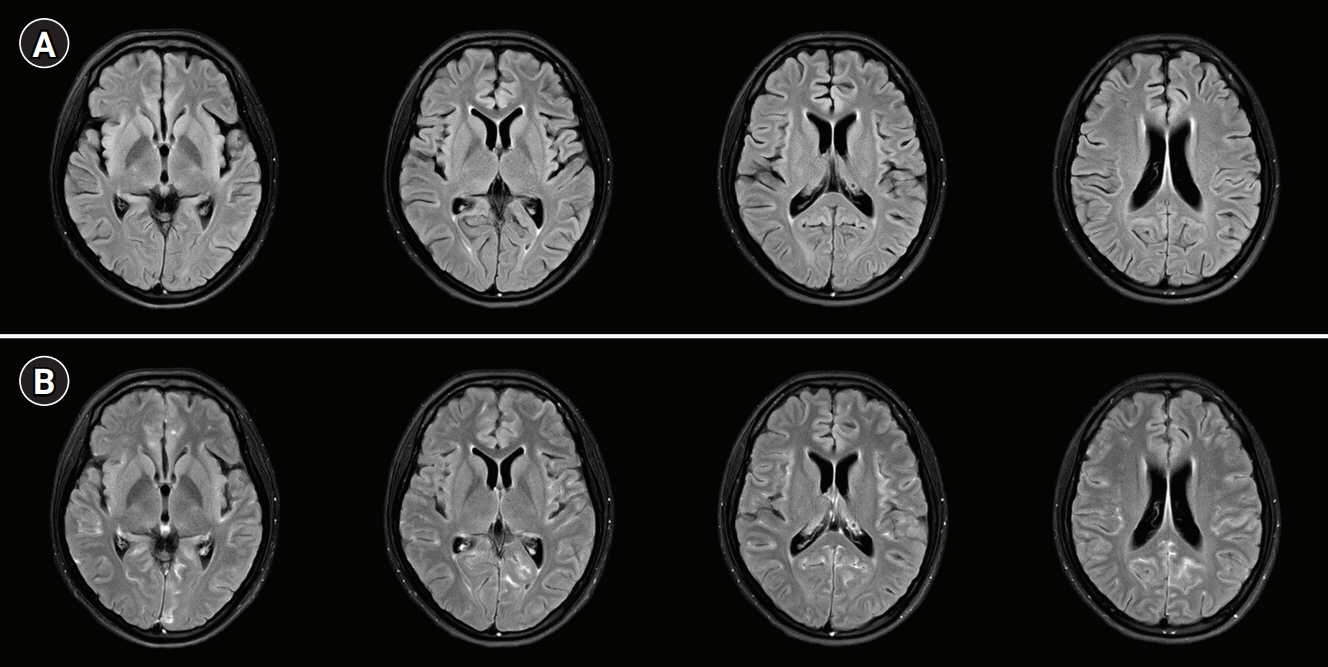
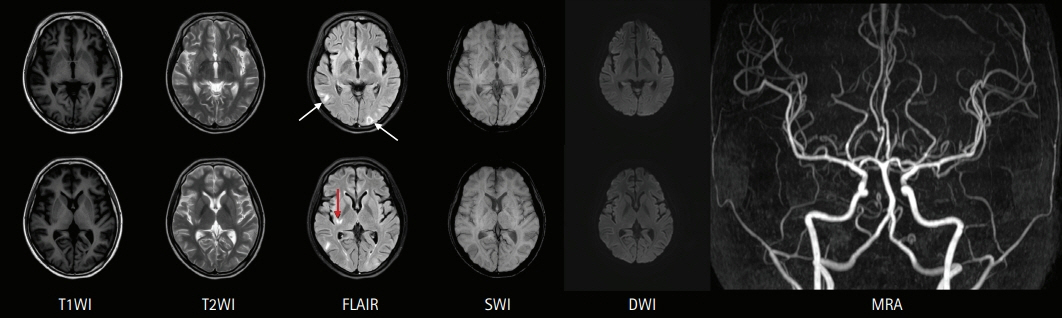
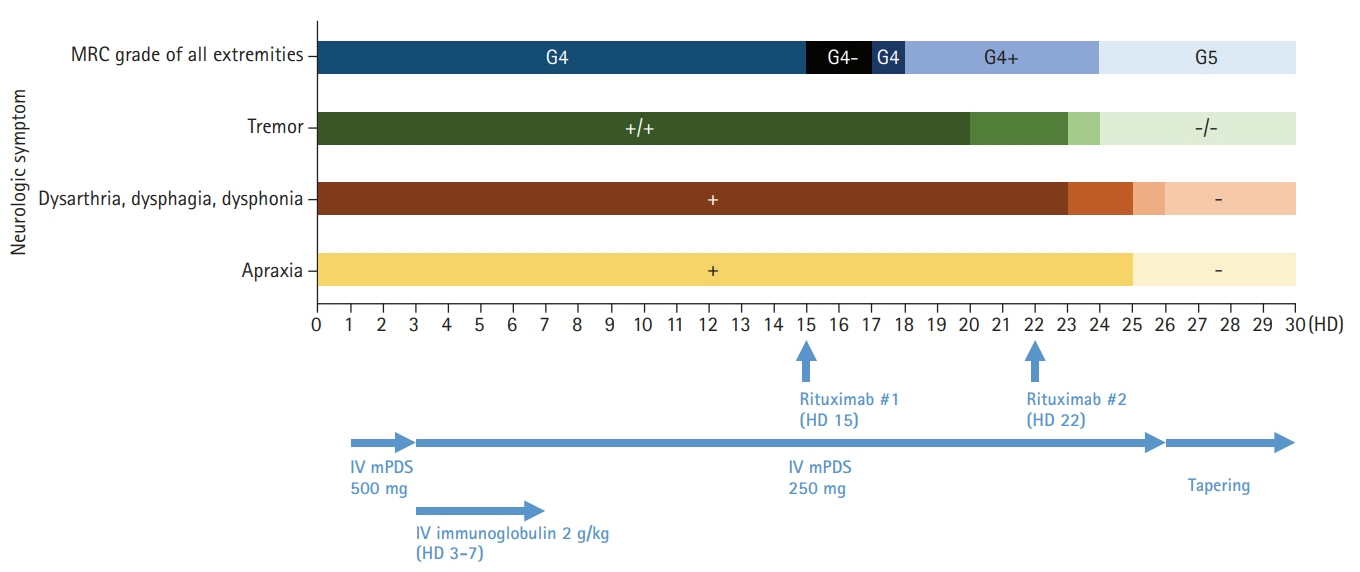
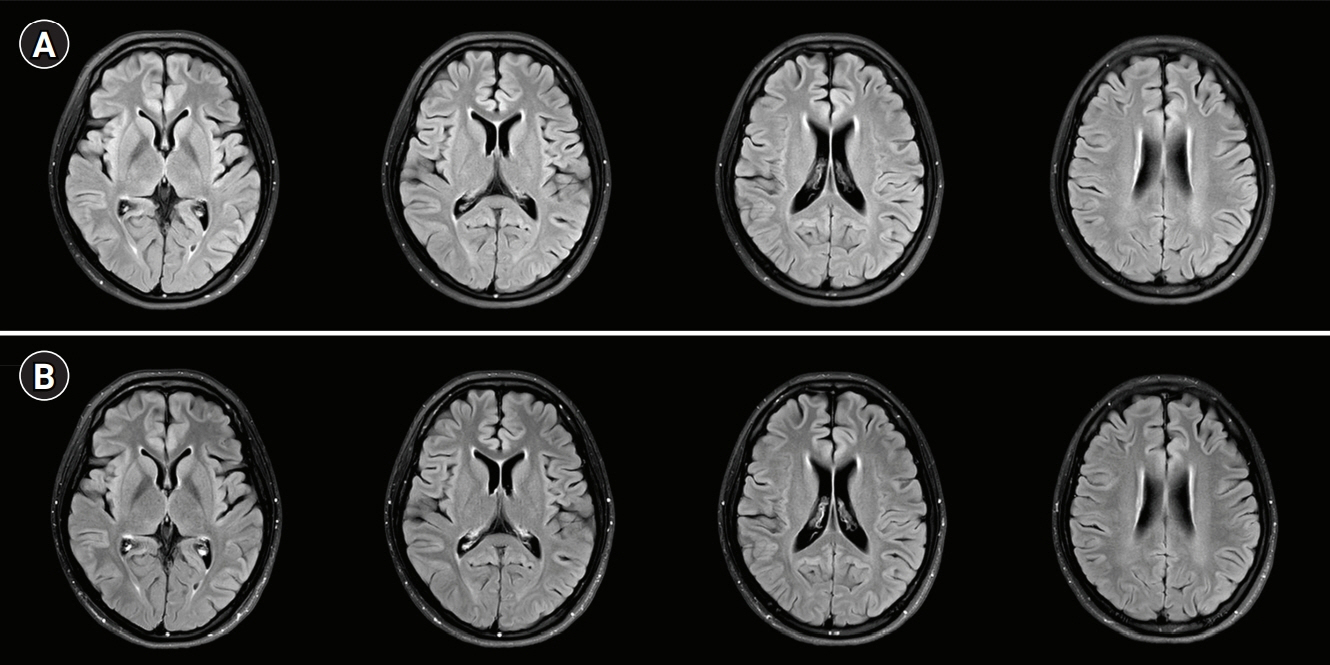
A 19-year-old woman with SLE presented with fever, headache, quadriparesis, and tremor. Brain magnetic resonance imaging (MRI) showed sulcal enhancement in the cortical sulcus, and intravenous methylprednisolone (500 mg/day) and immunoglobulin (2 g/kg for 5 days) were started under the suspicion of aseptic lupus meningitis. However, the patient’s neurologic symptoms worsened; brain MRI showed a newly developed brain parenchymal lesion, suggesting lupus cerebritis and posterior reversible encephalopathy syndrome. Two cycles of rituximab (850 mg/day, 1-week interval) were administered for the treatment of refractory NPSLE. Her neurologic symptoms gradually improved after the second cycle, and she was discharged with minimal neurologic symptoms.
Conclusion
Rituximab may be a therapeutic option for refractory lupus cerebritis. Further research is needed to accurately determine its efficacy.
Keyword
Figure
Reference
-
1. Govoni M, Bortoluzzi A, Padovan M, Silvagni E, Borrelli M, Donelli F, et al. The diagnosis and clinical management of the neuropsychiatric manifestations of lupus. J Autoimmun. 2016; 74:41–72.
Article2. The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999; 42:599–608.3. Schwartz N, Stock AD, Putterman C. Neuropsychiatric lupus: new mechanistic insights and future treatment directions. Nat Rev Rheumatol. 2019; 15:137–52.
Article4. Carrión-Barberà I, Salman-Monte TC, Vílchez-Oya F, Monfort J. Neuropsychiatric involvement in systemic lupus erythematosus: a review. Autoimmun Rev. 2021; 20:102780.
Article5. Muhammad O, Jindal H, Sharath M, Khan AM, Choi S. Systemic lupus erythematosus with multi-organ involvement in a young female: lymphadenopathy, lupus cerebritis, lupus nephritis, and cardiac manifestations. Cureus. 2021; 13:e15517.
Article6. Bertsias GK, Tektonidou M, Amoura Z, Aringer M, Bajema I, Berden JH, et al. Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis. 2012; 71:1771–82.
Article7. Hanly JG. Diagnosis and management of neuropsychiatric SLE. Nat Rev Rheumatol. 2014; 10:338–47.
Article8. Bertsias GK, Boumpas DT. Pathogenesis, diagnosis and management of neuropsychiatric SLE manifestations. Nat Rev Rheumatol. 2010; 6:358–67.
Article9. Ahn GY, Kim D, Won S, Song ST, Jeong HJ, Sohn IW, et al. Prevalence, risk factors, and impact on mortality of neuropsychiatric lupus: a prospective, single-center study. Lupus. 2018; 27:1338–47.
Article10. Kwon HS, Kim YS, Lee JM, Koh SH, Kim HY, Kim C, et al. Causes, risk factors, and clinical outcomes of stroke in Korean young adults: systemic lupus erythematosus is associated with unfavorable outcomes. J Clin Neurol. 2020; 16:605–11.
Article11. Bortoluzzi A, Scirè CA, Bombardieri S, Caniatti L, Conti F, De Vita S, et al. Development and validation of a new algorithm for attribution of neuropsychiatric events in systemic lupus erythematosus. Rheumatology (Oxford). 2015; 54:891–8.
Article12. Magro-Checa C, Zirkzee EJ, Huizinga TW, Steup-Beekman GM. Management of neuropsychiatric systemic lupus erythematosus: current approaches and future perspectives. Drugs. 2016; 76:459–83.
Article13. Nikolopoulos D, Fanouriakis A, Bertsias G. Treatment of neuropsychiatric systemic lupus erythematosus: clinical challenges and future perspectives. Expert Rev Clin Immunol. 2021; 17:317–30.
Article14. Barile-Fabris L, Ariza-Andraca R, Olguín-Ortega L, Jara LJ, Fraga-Mouret A, Miranda-Limón JM, et al. Controlled clinical trial of IV cyclophosphamide versus IV methylprednisolone in severe neurological manifestations in systemic lupus erythematosus. Ann Rheum Dis. 2005; 64:620–5.
Article15. Tokunaga M, Saito K, Kawabata D, Imura Y, Fujii T, Nakayamada S, et al. Efficacy of rituximab (anti-CD20) for refractory systemic lupus erythematosus involving the central nervous system. Ann Rheum Dis. 2007; 66:470–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Reversible Encephalopathy Syndrome in a Patient with Lupus Nephritis
- Posterior Reversible Encephalopathy Syndrome in a Patient with Systemic Lupus Erythematosus and Systemic Sclerosis Overlap Syndrome
- Posterior Reversible Encephalopathy Syndrome in a Patient with Intoxication of Arisaema amurense
- Irreversible Hemorrhagic Complication of Recurrent Posterior Reversible Encephalopathy Syndrome in a Patient with Systemic Lupus Erythematosus
- Cyclophosphamide-induced Posterior Reversible Encephalopathy Syndrome in a Patient with Lupus Nephritis