Neurointervention.
2021 Nov;16(3):280-284. 10.5469/neuroint.2021.00367.
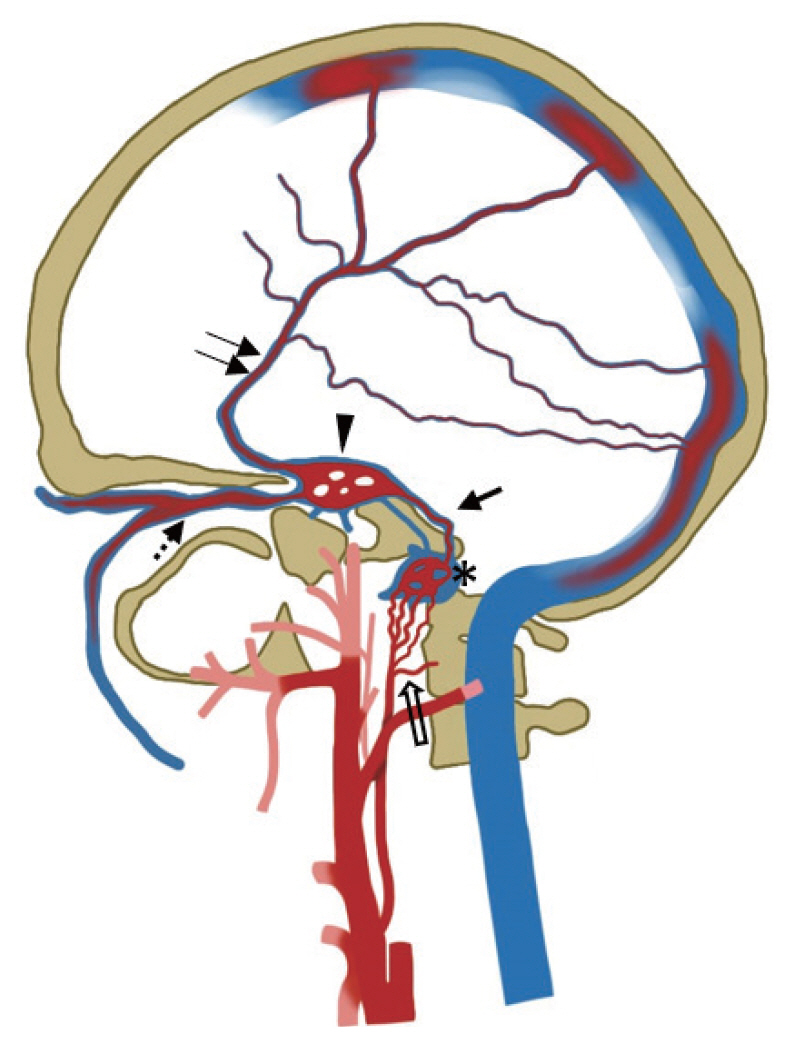
Direct Superior Ophthalmic Vein Approach to Treat Anterior Condylar Confluence Dural Arteriovenous Fistula
- Affiliations
-
- 1Department of Interventional Neuroradiology, G. Kuppuswamy Naidu Memorial Hospital, Coimbatore, India
- 2Department of Neurosurgery, G. Kuppuswamy Naidu Memorial Hospital, Coimbatore, India
- 3Division of Neuroradiology, Department of Radiology, Cerrahapasa Medical Faculty, Istanbul University, Istanbul, Turkey
- 4Department of Radiology, St John’s Medical College, Bengaluru, India
- KMID: 2522043
- DOI: http://doi.org/10.5469/neuroint.2021.00367
Abstract
- Dural arteriovenous fistulas (DAVFs) are acquired pathological arteriovenous connections involving vessels that usually supply the meninges. A DAVF in the region of the hypoglossal canal is a rare form of fistula that involves the anterior condylar confluence or anterior condylar vein. We report a case of hypoglossal canal DAVF that was successfully embolized transvenously through a superior ophthalmic vein (SOV) approach. After failed attempts through jugular access, our patient was treated by a unique percutaneous direct puncture approach through the SOV, achieving complete obliteration of the fistula. A step-by-step description of the endovascular technique was described. The clinical course was uneventful without any new neurologic deficit. The eye symptoms and third nerve palsy had completely resolved at the 3-month follow-up visit. Hypoglossal canal DAVFs are rare and may exhibit complex venous drainage patterns. Knowledge of the complex venous anatomy is essential for planning an alternative transvenous route if the standard approach is not feasible. Xper CT (Philips Healthcare, Best, The Netherlands) is an excellent tool for identifying the exact site of the fistula as well as for confirming a safe position of the catheter tip for successful occlusion of this complex dural AV fistula.
Figure
Reference
-
1. Choi JW, Kim BM, Kim DJ, Kim DI, Suh SH, Shin NY, et al. Hypoglossal canal dural arteriovenous fistula: incidence and the relationship between symptoms and drainage pattern. J Neurosurg. 2013; 119:955–960.
Article2. Ernst R, Bulas R, Tomsick T, van Loveren H, Aziz KA. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. AJNR Am J Neuroradiol. 1999; 20:2016–2020.3. Lv X, Jiang C, Zhang J, Li Y, Wu Z. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. AJNR Am J Neuroradiol. 2009; 30:462–468.
Article4. Spittau B, Millán DS, El-Sherifi S, Hader C, Singh TP, Motschall E, et al. Dural arteriovenous fistulas of the hypoglossal canal: systematic review on imaging anatomy, clinical findings, and endovascular management. J Neurosurg. 2015; 122:883–903.
Article5. Manabe H, Hasegawa S, Takemura A, Shafiqul IM, Ito C, Nagahata M. Contralateral inferior petrosal sinus approach for transvenous embolization of a dural arteriovenous fistula at isolated jugular bulb. Technical case report. Minim Invasive Neurosurg. 2003; 46:366–368.
Article6. Dye J, Duckwiler G, Gonzalez N, Kaneko N, Goldberg R, Rootman D, et al. Endovascular approaches to the cavernous sinus in the setting of dural arteriovenous fistula. Brain Sci. 2020; 10:554.
Article7. White JB, Layton KF, Evans AJ, Tong FC, Jensen ME, Kallmes DF, et al. Transorbital puncture for the treatment of cavernous sinus dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2007; 28:1415–1417.
Article8. Trivelato FP, Manzato LB, Filho PMM, Ulhôa AC, Vanzin JR, Abud DG, et al. Transorbital cavernous sinus direct puncture: alternative to treat dural arteriovenous fistula. Clin Neuroradiol. 2018; 28:55–61.9. Kurata A, Suzuki S, Iwamoto K, Miyazaki T, Inukai M, Abe K, et al. Direct-puncture approach to the extraconal portion of the superior ophthalmic vein for carotid cavernous fistulae. Neuroradiology. 2009; 51:755–759.
Article10. Shinoda N, Mori M, Tamura S, Korosue K, Kose S, Imai H, et al. A patient with a cavernous sinus dural arteriovenous fistula in whom direct puncture of the superior ophthalmic vein led to rapidly progressing thrombosis and postoperative non-arteritic ischemic optic neuropathy: pathogenesis with respect to a drainage route. JNET. 2019; 13:221–227.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Dural Arteriovenous Fistula of the Anterior Condylar Vein
- Transvenous Embolization of Dural Carotid Cavernous Fistula through the Supraorbital Vein
- Transvenous Embolization of Cavernous Sinus Dural Arteriovenous Fistula Using the Direct Superior Ophthalmic Vein Approach: A Case Report
- Superior ophthalmic approach in carotid-cavernous fistula: current concepts in indications, surgical techniques, and case reviews
- Transvenous Coil Embolization for Dural Arteriovenous Fistulas of the Ophthalmic Sheath: Report of Two Cases and Review of the Literature