J Cerebrovasc Endovasc Neurosurg.
2023 Sep;25(3):245-252. 10.7461/jcen.2023.E2022.10.005.
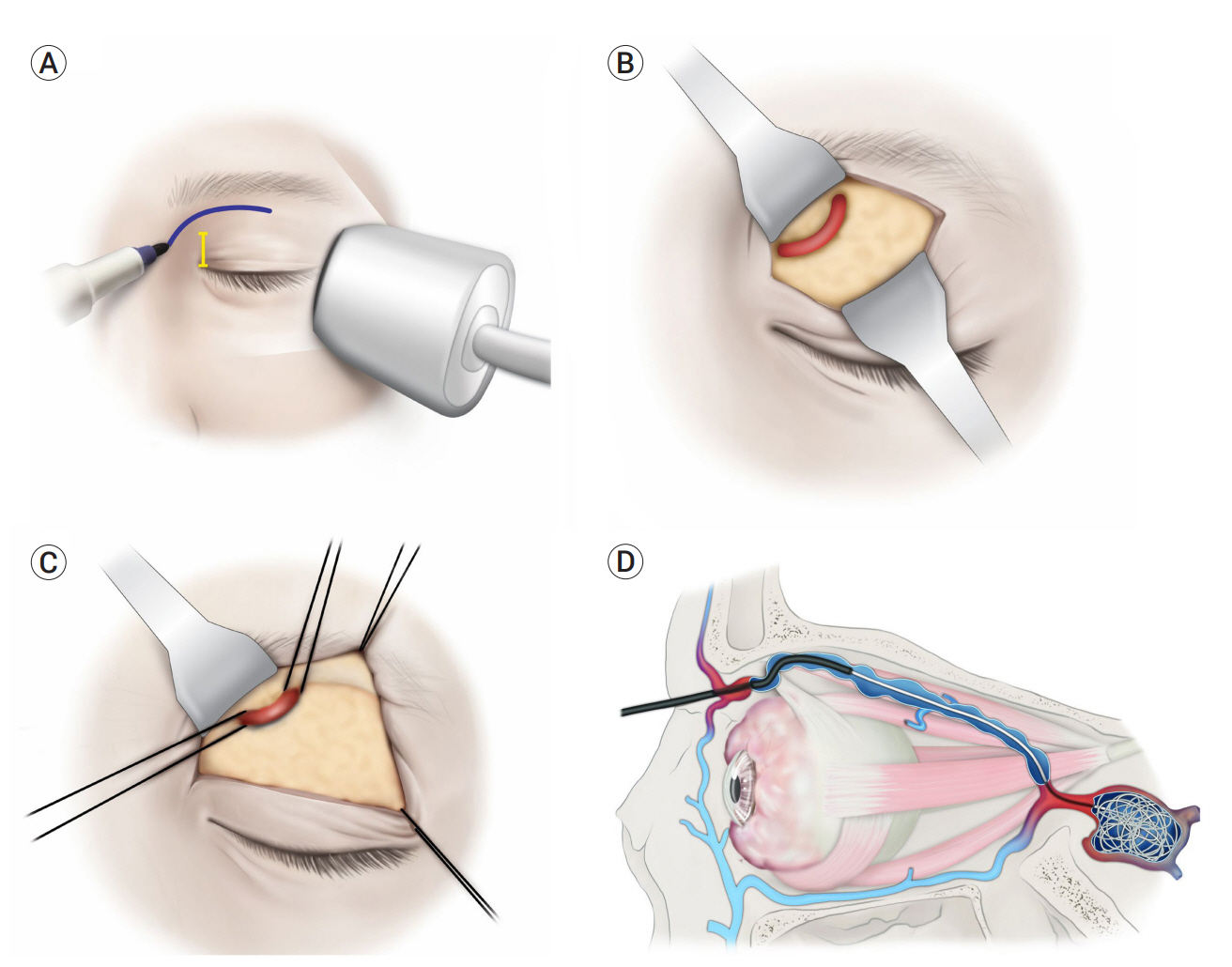
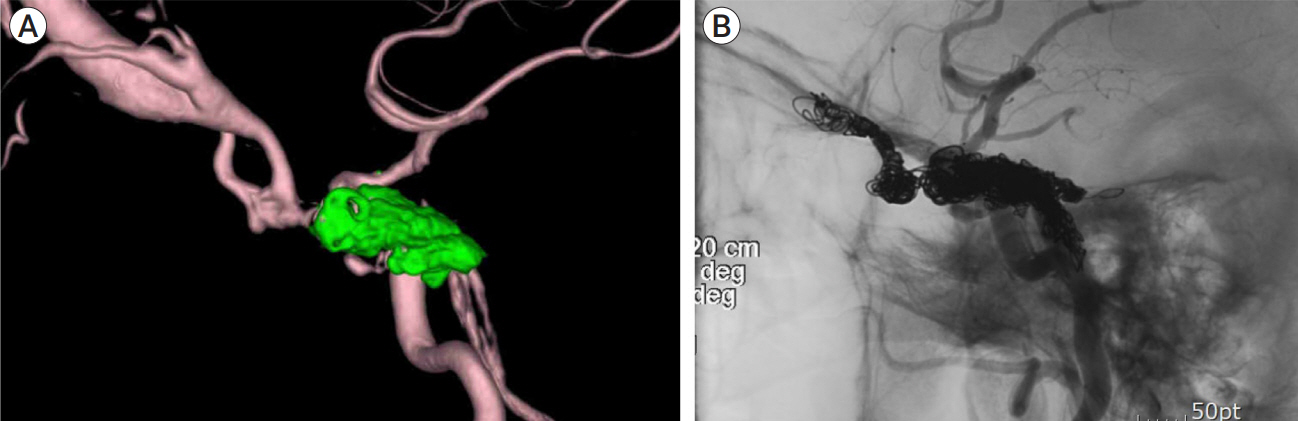
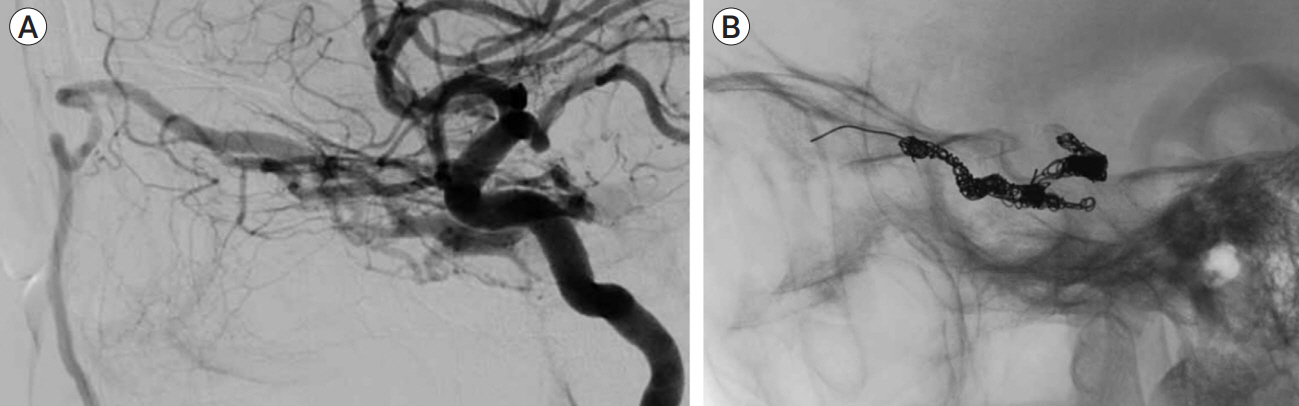
Superior ophthalmic approach in carotid-cavernous fistula: current concepts in indications, surgical techniques, and case reviews
- Affiliations
-
- 1Department of Ophthalmology, School of Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2546160
- DOI: http://doi.org/10.7461/jcen.2023.E2022.10.005
Abstract
- Carotid-cavernous fistulas, characterized by abnormal arteriovenous communication within the cavernous sinus (CS), can be classified as direct or indirect. Direct fistulas are defined as a direct connection between the internal carotid artery (ICA) and CS, whereas indirect fistulas result from an abnormal connection between the CS and dural arterial branches. The first-line treatment for both types of fistulas is endovascular intervention, most commonly accomplished through the transarterial and transvenous approaches of the conventional pathway, including the ICA, inferior and superior petrosal sinuses, or basilar plexus. Nonetheless, a retrograde approach through the superior ophthalmic vein may be necessary for individuals in whom conventional endovascular treatment fails. Herein, the current principles of surgical indication and technique are presented, along with case studies.
Figure
Reference
-
1. Adam CR, Shields CL, Gutman J, Kim HJ, Hayek B, Shore JW, et al. Dilated superior ophthalmic vein: clinical and radiographic features of 113 cases. Ophthalmic Plast Reconstr Surg. 2018; Jan-Feb. 34(1):68–73.2. Ageno W, Turpie A. Venous thromboembolism: pathophysiology and diagnosis. Therapeutic Strategies in Thrombosis Atlas Medical Publish;2006. p. 301–14.3. Andrade G, De Souza MLP, Marques R, Silva JL, Abath C, Azevedo-Filho HR. Endovascular treatment of traumatic carotid cavernous fistula with balloon-assisted sinus coiling: a technical description and initial results. Interv Neuroradiol. 2013; Dec. 19(4):445–54.4. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985; Feb. 62(2):248–56.5. Debrun GM. Angiographic workup of a carotid cavernous sinus fistula (CCF) or what information does the interventionalist need for treatment? Surg Neurol. 1995; 44(1):75–9.6. Debrun GM, Viñuela F, Fox AJ, Davis KR, Ahn HS. Indications for treatment and classification of 132 carotid-cavernous fistulas. Neurosurgery. 1988; Feb. 22(2):285–9.7. Fattahi TT, Brandt MT, Jenkins WS, Steinberg B. Traumatic carotid-cavernous fistula: pathophysiology and treatment. J Craniofac Surg. 2003; 14(2):240–6.8. Gemmete JJ, Ansari SA, Gandhi DM. Endovascular techniques for treatment of carotid-cavernous fistula. J Neuroophthalmol. 2009; 29(1):62–71.9. Gioulekas J, Mitchell P, Tress B, McNab AA. Embolization of carotid cavernous fistulas via the superior ophthalmic vein. Aust N Z J Ophthalmol. 1997; Feb. 25(1):47–53.10. Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye (Lond). 2018; Feb. 32(2):164–72.11. Jia ZY, Song YS, Sheen JJ, Kim JG, Lee DH, Suh DC. Cannulation of occluded inferior petrosal sinuses for the transvenous embolization of cavernous sinus dural arteriovenous fistulas: usefulness of a frontier-wire probing technique. AJNR Am J Neuroradiol. 2018; Dec. 39(12):2301–6.12. Jimenez DF, Gibbs SR. Carotid-cavernous sinus fistulae in craniofacial trauma: classification and treatment. J Craniomaxillofac Trauma. 1997; Fall. 3(3):7–15.13. Kirsch M, Henkes H, Liebig T, Weber W, Esser J, Golik S, et al. Endovascular management of dural carotid–cavernous sinus fistulas in 141 patients. Neuroradiology. 2006; Jul. 48(7):486–90.14. Klisch J, Huppertz HJ, Spetzger U, Hetzel A, Seeger W, Schumacher M. Transvenous treatment of carotid cavernous and dural arteriovenous fistulae: results for 31 patients and review of the literature. Neurosurgery. 2003; Oct. 53(4):836–56. discussion 856-7.15. Leibovitch I, Modjtahedi S, Duckwiler GR, Goldberg RA. Lessons learned from difficult or unsuccessful cannulations of the superior ophthalmic vein in the treatment of cavernous sinus dural fistulas. Ophthalmology. 2006; Jul. 113(7):1220–6.16. Massa RN, Minutello K, Mesfin FB. Neuroanatomy, Cavernous Sinus. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing;2021.17. Meyers PM, Halbach VV, Dowd CF, Lempert TE, Malek AM, Phatouros CC, et al. Dural carotid cavernous fistula: definitive endovascular management and long-term follow-up. Am J Ophthalmol. 2002; Jul. 134(1):85–92.18. Miller NR. Diagnosis and management of dural carotid–cavernous sinus fistulas. Neurosurg Focus. 2007; 23(5):e13.19. Miller NR, Monsein LH, Debrun GM, Tamargo RJ, Nauta HJ. Treatment of carotid-cavernous sinus fistulas using a superior ophthalmic vein approach. J Neurosurg. 1995; Nov. 83(5):838–42.20. Park J, Lee JI, Choi HY. Surgical tips for approaching to superior ophthalmic vein in patients with a carotid cavernous fistula. Korean J Ophthalmol. 2021; Aug. 35(4):325–7.21. Park J, Lee JI, Jeon H, Choi HY. Direct approach to thrombosed superior ophthalmic vein of recalcitrant indirect carotid cavernous fistula in thrombocythemia failed with multiple conventional embolization treatment. Int J Ophthalmol. 2020; Apr. 13(4):687–92.22. Satchi K, Mitchell PJ, McNab AA. Transorbital puncture of the cavernous sinus to treat a dural carotid-cavernous sinus fistula. Ophthalmic Plast Reconstruct Surg. 2009; JanFeb. 25(1):54–6.23. Shiu PC, Hanafee WN, Wilson GH, Rand RW. Cavernous sinus venography. Am J Roentgenol Radium Ther Nucl Med. 1968; Sep. 104(1):57–62.24. Srinivas H, Murthy S, Brown R. Is Valsalva manoeuvre useful in diagnosing dural caroticocavernous fistulas? Eye (Lond). 2005; Nov. 19(11):1226–7.25. Stiebel-Kalish H, Setton A, Nimii Y, Kalish Y, Hartman J, BarOn RH, et al. Cavernous sinus dural arteriovenous malformations: patterns of venous drainage are related to clinical signs and symptoms. Ophthalmology. 2002; Sep. 109(9):1685–91.26. Woolen S, Gemmete JJ, Pandey AS, Chaudhary N. Dural carotid-cavernous fistula presenting with confusion and expressive aphasia. J Clin Neurosci. 2015; Nov. 22(11):1844–6.27. Yilmaz SG, Yazici B, Çetinkaya A, Yagci A. Embolization of dural carotid-cavernous fistulas via the thrombosed superior ophthalmic vein. Ophthalmic Plast Reconstr Surg. 2013; Jul-Aug. 29(4):272–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coil Embolization Via a Superior Ophthalmic Vein Approach of Carotid Cavernous Sinus Fistula
- Treatment of a Carotid-Cavernous Sinus Fistula via the Superior Ophthalmic Vein Approach: A Case Report
- Intraoperative Embolization of Dural Carotid-Cavernous Fistula: Case Report
- Transvenous Embolization of Cavernous Sinus Dural Arteriovenous Fistula Using the Direct Superior Ophthalmic Vein Approach: A Case Report
- Transvenous Embolization of Dural Carotid Cavernous Fistula through the Supraorbital Vein