Neurointervention.
2021 Jul;16(2):122-131. 10.5469/neuroint.2021.00199.
Endovascular Treatment of Intracranial Aneurysms Using the Novel Low Profile Visualized Intraluminal Support EVO Stent: Multicenter Early Feasibility Experience
- Affiliations
-
- 1Interventional Neuroradiology Service, Department of Radiology, Austin Health, Heidelberg, VIC, Australia
- 2Interventional Neuroradiology Service, Department of Radiology, Monash Health, Clayton, VIC, Australia
- 3School of Medicine, Deakin University, Waurn Ponds, VIC, Australia
- 4Interventional Neuroradiology Service, Department of Radiology, St Vincent’s Hospital Melbourne, Fitzroy, VIC, Australia
- 5Department of Imaging, Monash University, Clayton, VIC, Australia
- 6Faculty of Medicine and Health Sciences, Macquarie University, Macquarie Park, NSW, Australia
- 7Faculty of Medicine, Dentistry and Health Sciences, The University of Melbourne, Melbourne, VIC, Australia
- 8Neurosurgery Department, Austin Health, Heidelberg, VIC, Australia
- 9Interventional Radiology Service, Department of Radiology, Northern Health, Epping, VIC, Australia
- 10Florey Institute of Neurosciences and Mental Health, The University of Melbourne, Parkville, VIC, Australia
- KMID: 2517737
- DOI: http://doi.org/10.5469/neuroint.2021.00199
Abstract
- Purpose
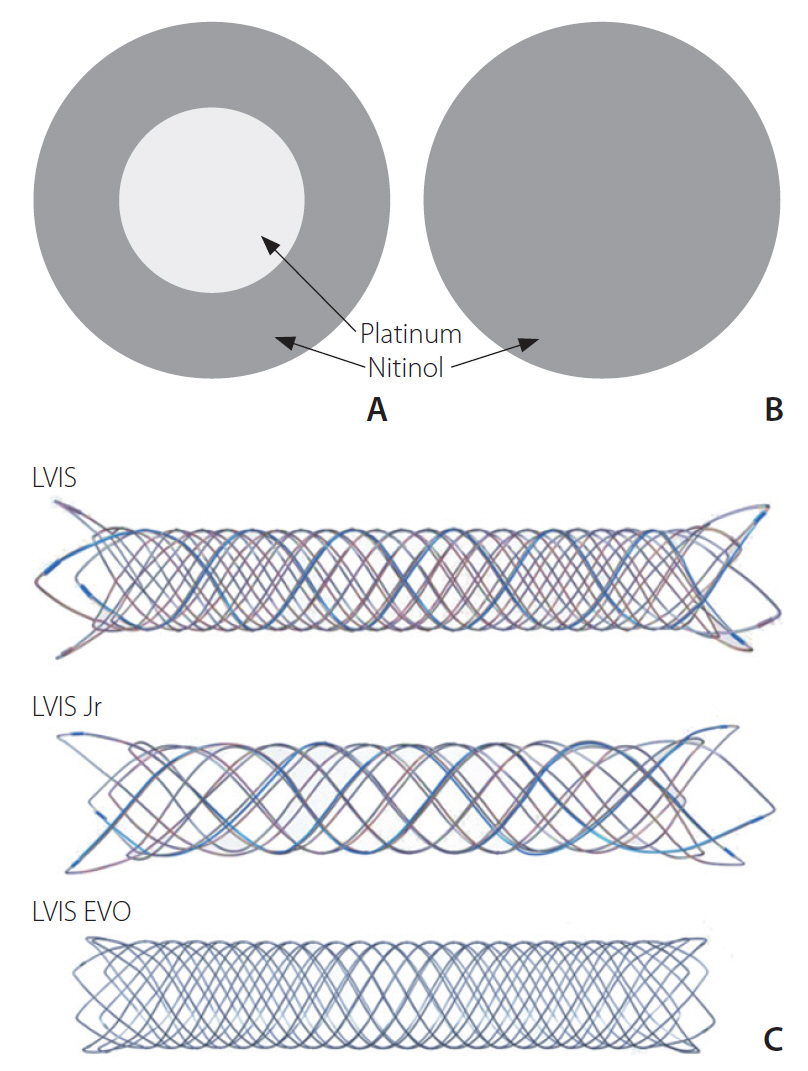
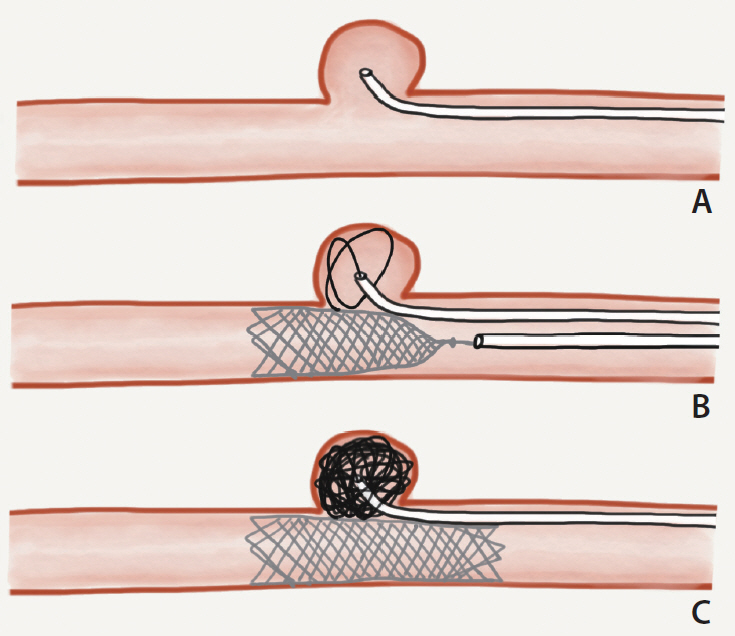
Low-profile, self-expandable stents have broadened therapeutic options available for definitive treatment of intracranial aneurysms. The novel Low-Profile Visualized Intraluminal Support (LVIS) EVO stent extends upon the success of its predecessor, the LVIS Jr stent, aiming to enable higher visibility and greater opening ability within a self-expandable and fully retrievable microstent system. In this study, we aim to report the early safety and feasibility experience with the LVIS EVO stent.
Materials and Methods
A multicenter, retrospective, observational study was conducted on patients who had intracranial aneurysms treated with the LVIS EVO stent across 3 Australian neurovascular centers between February 2020 and September 2020. Short-term technical and clinical outcomes were evaluated.
Results
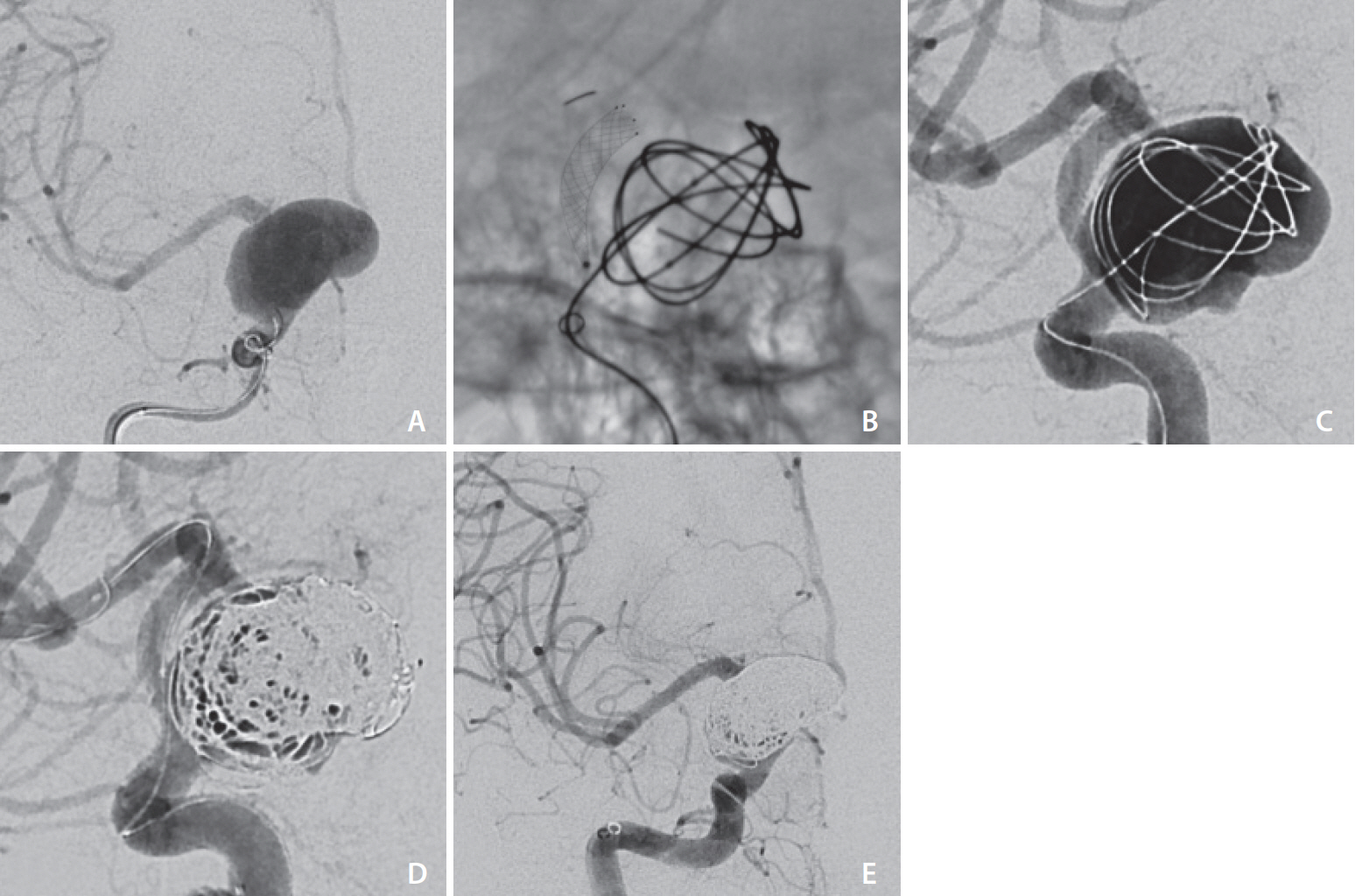
A total of 22 LVIS EVO stents were successfully implanted to treat 15 aneurysms (3 ruptured, 12 unruptured) in 15 patients. Aneurysms ranged from 2 mm to 35 mm in dome height. The LVIS EVO stent was used for stent-assisted coiling in 11 patients and flow diversion in 4 patients. There were no device-related procedural complications. There were 2 cases of peri-procedural symptomatic thromboembolic complications and no procedure-related mortality. At early radiological follow up, 10 patients had complete occlusion, 4 patients had small neck remnants, and 1 patient who was managed with flow diversion had a residual aneurysm.
Conclusion
Early experience with the LVIS EVO stent demonstrated safety and feasibility for stent-assisted coiling as well as flow diversion for intracranial aneurysms. In this heterogeneous cohort, including ruptured, complex, and large aneurysms, all cases were technically successful.
Keyword
Figure
Reference
-
1. Phan K, Huo YR, Jia F, Phan S, Rao PJ, Mobbs RJ, et al. Meta-analysis of stent-assisted coiling versus coiling-only for the treatment of intracranial aneurysms. J Clin Neurosci. 2016; 31:15–22.
Article2. Aydin K, Arat A, Sencer S, Barburoglu M, Men S. Stent-assisted coiling of wide-neck intracranial aneurysms using low-profile LEO baby stents: initial and midterm results. AJNR Am J Neuroradiol. 2015; 36:1934–1941.
Article3. Fiorella D, Boulos A, Turk AS, Siddiqui AH, Arthur AS, Diaz O, LVIS investigators, et al. The safety and effectiveness of the LVIS stent system for the treatment of wide-necked cerebral aneurysms: final results of the pivotal US LVIS trial. J Neurointerv Surg. 2019; 11:357–361.
Article4. Wang C, Tian Z, Liu J, Jing L, Paliwal N, Wang S, et al. Flow diverter effect of LVIS stent on cerebral aneurysm hemodynamics: a comparison with Enterprise stents and the Pipeline device. J Transl Med. 2016; 14:199.
Article5. Cagnazzo F, Cappucci M, Dargazanli C, Lefevre PH, Gascou G, Riquelme C, et al. Flow-diversion effect of LEO stents: aneurysm occlusion and flow remodeling of covered side branches and perforators. AJNR Am J Neuroradiol. 2018; 39:2057–2063.
Article6. Wang K, Huang Q, Hong B, Li Z, Fang X, Liu J. Correlation of aneurysm occlusion with actual metal coverage at neck after implantation of flow-diverting stent in rabbit models. Neuroradiology. 2012; 54:607–613.
Article7. Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH, et al. An update to the Raymond-Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg. 2015; 7:496–502.
Article8. O’kelly CJ, Krings T, Fiorella D, Marotta TR. A novel grading scale for the angiographic assessment of intracranial aneurysms treated using flow diverting stents. Interv Neuroradiol. 2010; 16:133–137.
Article9. Hendricks BK, Yoon JS, Yaeger K, Kellner CP, Mocco J, De Leacy RA, et al. Wide-neck aneurysms: systematic review of the neurosurgical literature with a focus on definition and clinical implications. [published online ahead of print Jun 14, 2019]. J Neurosurg. 2019.
Article10. Regelsberger J, Matschke J, Grzyska U, Ries T, Fiehler J, Köppen J, et al. Blister-like aneurysms--a diagnostic and therapeutic challenge. Neurosurg Rev. 2011; 34:409–416.
Article11. Sirakov A, Bhogal P, Möhlenbruch M, Sirakov S. Endovascular treatment of patients with intracranial aneurysms: feasibility and successful employment of a new low profile visible intraluminal support (LVIS) EVO stent. Neuroradiol J. 2020; 33:377–385.
Article12. Poncyljusz W, Kubiak K. Initial experience with LVIS EVO stents for the treatment of intracranial aneurysms. J Clin Med. 2020; 9:3966.
Article13. Pandey AS, Koebbe C, Rosenwasser RH, Veznedaroglu E. Endovascular coil embolization of ruptured and unruptured posterior circulation aneurysms: review of a 10-year experience. Neurosurgery. 2007; 60:626–636. discussion 636-637.14. Ferns SP, Sprengers ME, van Rooij WJ, Rinkel GJ, van Rijn JC, Bipat S, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke. 2009; 40:e523–e529.15. Vollherbst DF, Berlis A, Maurer C, Behrens L, Sirakov S, Sirakov A, et al. Periprocedural safety and feasibility of the new LVIS EVO device for stent-assisted coiling of intracranial aneurysms: an observational multicenter study. AJNR Am J Neuroradiol. 2021; 42:319–326.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Angiographic Outcomes of Endovascular Treatment for Acute Intracranial Vertebral Artery Dissecting Aneurysms Using Double-Overlapping Stents : Low-Profile Visualized Intraluminal Support within Enterprise Stents
- Endovascular treatment of intracranial aneurysms: Past and present
- Flow diversion via telescoping stent with Low-profile Visualized Intraluminal Support Junior for treatment of ruptured dissecting aneurysm located at proximal posterior inferior cerebellar artery
- Preliminary Experience of Lvis Blue in the Internal Carotid Artery for The Treatment Of Wide-Necked Intracranial Aneurysms
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms