J Korean Neurosurg Soc.
2024 Aug;67(5):531-540. 10.3340/jkns.2023.0224.
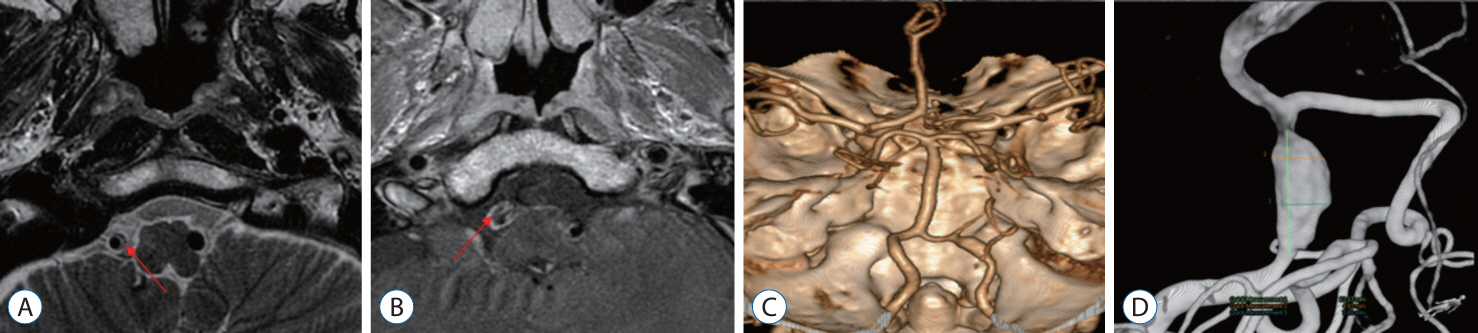
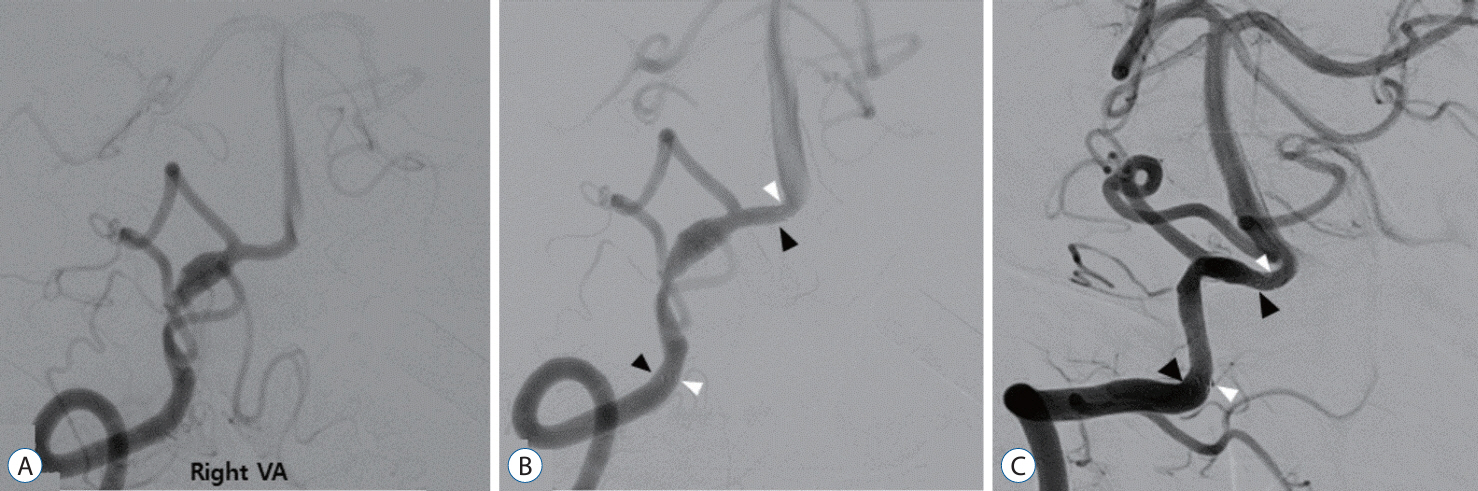
Clinical and Angiographic Outcomes of Endovascular Treatment for Acute Intracranial Vertebral Artery Dissecting Aneurysms Using Double-Overlapping Stents : Low-Profile Visualized Intraluminal Support within Enterprise Stents
- Affiliations
-
- 1Department of Neurosurgery, Ajou University School of Medicine, Suwon, Korea
- KMID: 2558678
- DOI: http://doi.org/10.3340/jkns.2023.0224
Abstract
Objective
: The use of reconstructive treatment with a double-overlapping stents has proven to be effective and safe in the current treatment of intracranial vertebral artery dissecting aneurysms (VADAs). We employed a combination of overlapping stents, using low-profile visualized intraluminal support (LVIS) within the Enterprise stent. This combination was chosen to minimize the outward bulging of the inner LVIS by overlapping it with the Enterprise stent while maintaining flow diversion and stability. This study aimed to evaluate the clinical and angiographic outcomes following the use of double-overlapping stents with LVIS within the Enterprise stent for the treatment of VADAs.
Methods
: From March 2016 to January 2022, total 28 patients with unruptured VADAs were treated with the double-overlapping stent technique using LVIS within an Enterprise stent in our institute. The Enterprise stent was deployed first, followed by the LVIS stent. Patient clinical and angiographic characteristics, procedural complications, and follow-up outcomes were retrospectively reviewed.
Results
: All 28 patients (18 males and 10 females) were successfully treated with double-overlapping stent deployment. There were no procedural complications or new neurological deficits in any patient. Of the 28 patients, four VADAs had posterior inferior cerebellar artery involvement. Procedure-related parent artery occlusion did not occur during the angiographic follow-up conducted 6 to 12 months after the procedure. Out of 28 patients, 24 showed complete healing, three had focal residual stenosis or dilatation with residual sac and only one had a residual dissecting flap with aneurysm. All patients, including the four patients, did not require any additional procedures. The postoperative modified Rankin scale scores were 0–1 for all patients.
Conclusion
: A double-overlapping stent, with a flow-diversion effect, is a safe and effective treatment for patients with VADAs. In particular, when using the LVIS stent within an Enterprise stent, it minimizes the bulging of the inner LVIS stent while maintaining flow diversion and stability. Therefore, both can be effectively utilized as overlapping stents.
Figure
Reference
-
References
1. Ahn JY, Han IB, Kim TG, Yoon PH, Lee YJ, Lee BH, et al. Endovascular treatment of intracranial vertebral artery dissections with stent placement or stent-assisted coiling. AJNR Am J Neuroradiol. 27:1514–1520. 2006.2. Asai K, Nakamura H, Nishida T, Morris S, Sakaki T. Overlapping stent-assisted coil embolization for a ruptured intracranial vertebral artery dissection. J Surg Case Rep. 2017:rjx105. 2017.
Article3. Benndorf G, Herbon U, Sollmann WP, Campi A. Treatment of a ruptured dissecting vertebral artery aneurysm with double stent placement: case report. AJNR Am J Neuroradiol. 22:1844–1848. 2001.4. Bhogal P, Brouwer PA, Söderqvist ÅK, Ohlsson M, Andersson T, Holmin S, et al. Patients with subarachnoid haemorrhage from vertebrobasilar dissection: treatment with stent-in-stent technique. Neuroradiology. 57:605–614. 2015.5. Cerejo R, Bain M, Moore N, Hardman J, Bauer A, Hussain MS, et al. Flow diverter treatment of intracranial vertebral artery dissecting pseudoaneurysms. J Neurointerv Surg. 9:1064–1068. 2017.
Article6. Cho DY, Choi JH, Kim BS, Shin YS. Comparison of clinical and radiologic outcomes of diverse endovascular treatments in vertebral artery dissecting aneurysm involving the origin of PICA. World Neurosurg. 121:e22–e31. 2019.
Article7. Choi HH, Cho YD, Yoo DH, Kang HS, Han MH. LVIS-within-enterprise double-stent procedure without coiling beneficial as treatment of unruptured vertebral artery dissecting aneurysms. Interv Neuroradiol. 28:136–141. 2022.
Article8. Chung Y, Lee SH, Choi SK, Kim BJ, Lee KM, Kim EJ. Triple stent therapy for the treatment of vertebral dissecting aneurysms: efficacy and safety. World Neurosurg. 99:79–88. 2017.
Article9. Cohen JE, Gomori JM, Rajz G, Rosenthal G, El Hassan HA, Moscovici S, et al. Vertebral artery pseudoaneurysms secondary to blunt trauma: endovascular management by means of neurostents and flow diverters. J Clin Neurosci. 32:77–82. 2016.10. Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 14:640–654. 2015.
Article11. Guerrero WR, Ortega-Gutierrez S, Hayakawa M, Derdeyn CP, Rossen JD, Hasan D, et al. Endovascular treatment of ruptured vertebrobasilar dissecting aneurysms using flow diversion embolization devices: single-institution experience. World Neurosurg. 109:e164–e169. 2018.
Article12. Hernández-Durán S, Ogilvy CS. Clinical outcomes of patients with vertebral artery dissection treated endovascularly: a meta-analysis. Neurosurg Rev. 37:569–577. 2014.
Article13. Kim CH, Lee CH, Kim YH, Sung SK, Son DW, Lee SW, et al. Flow diverter devices for the treatment of unruptured vertebral artery dissecting aneurysm. J Korean Neurosurg Soc. 64:891–900. 2021.
Article14. Kim MJ, Chung J, Kim SL, Roh HG, Kwon BJ, Kim BS, et al. Stenting from the vertebral artery to the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 33:348–352. 2012.15. Kim S, Yang H, Hong I, Oh JH, Kim YB. Computational study of hemodynamic changes induced by overlapping and compacting of stents and flow diverter in cerebral aneurysms. Front Neurol. 12:705841. 2021.
Article16. Lim YC, Shin YS, Chung J. Flow diversion via LVIS blue stent within enterprise stent in patients with vertebral artery dissecting aneurysm. World Neurosurg. 117:203–207. 2018.
Article17. Liu P, Li Z, Hu L, Liu Y, Li P, Zhu W, et al. Clinical characteristics, endovascular choices, and surgical outcomes of intracranial vertebral artery dissecting aneurysms: a consecutive series of 196 patients. J Neurosurg. 138:215–222. 2022.
Article18. Liu Q, Qi C, Zhang Y, Deng L, Li G, Su W. Low-profile visualized intraluminal support stent-only technique for intracranial aneurysms-a report of 12 cases with midterm follow-up. World Neurosurg. 129:e40–e47. 2019.
Article19. Liu XL, Wang B, Zhao LB, Jia ZY, Shi HB, Liu S. Overlapping stents-assisted coiling for vertebral artery dissecting aneurysm : LVIS stent within neuroform EZ stent. J Korean Neurosurg Soc. 65:523–530. 2022.20. Lv N, Cao W, Larrabide I, Karmonik C, Zhu D, Liu J, et al. Hemodynamic changes caused by multiple stenting in vertebral artery fusiform aneurysms: a patient-specific computational fluid dynamics study. AJNR Am J Neuroradiol. 39:118–122. 2018.
Article21. Lylyk P, Ceratto R, Hurvitz D, Basso A. Treatment of a vertebral dissecting aneurysm with stents and coils: technical case report. Neurosurgery. 43:385–388. 1998.
Article22. Park SI, Kim BM, Kim DI, Shin YS, Suh SH, Chung EC, et al. Clinical and angiographic follow-up of stent-only therapy for acute intracranial vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 30:1351–1356. 2009.
Article23. Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 344:898–906. 2001.
Article24. Sekhon LH, Morgan MK, Sorby W, Grinnell V. Combined endovascular stent implantation and endosaccular coil placement for the treatment of a wide-necked vertebral artery aneurysm: technical case report. Neurosurgery. 43:380–383. discussion 384. 1998.
Article25. Suzuki T, Hasegawa H, Ando K, Shibuya K, Takahashi H, Saito S, et al. Possibility of worsening flow diversion effect due to morphological changes of a stented artery with multiple overlapping stents for partially thrombosed vertebral artery aneurysms. Front Neurol. 11:611124. 2020.26. Wang C, Tian Z, Liu J, Jing L, Paliwal N, Wang S, et al. Flow diverter effect of LVIS stent on cerebral aneurysm hemodynamics: a comparison with Enterprise stents and the Pipeline device. J Transl Med. 14:199. 2016.
Article27. Wang CC, Fang YB, Zhang P, Zhu X, Hong B, Xu Y, et al. Reconstructive endovascular treatment of vertebral artery dissecting aneurysms with the Low-profile Visualized Intraluminal Support (LVIS) device. PLoS One. 12:e0180079. 2017.
Article28. Zhao KJ, Fang YB, Huang QH, Xu Y, Hong B, Li Q, et al. Reconstructive treatment of ruptured intracranial spontaneous vertebral artery dissection aneurysms: long-term results and predictors of unfavorable outcomes. PLoS One. 8:e67169. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple telescopic stenting versus single flow diverter for the treatment of vertebral artery dissecting aneurysm
- Endovascular Treatment by using Double Stent Method for Ruptured Vertebral Artery Dissecting Aneurysms
- Overlapping Stents-Assisted Coiling for Vertebral Artery Dissecting Aneurysm : LVIS Stent within Neuroform EZ Stent
- Flow diversion via telescoping stent with Low-profile Visualized Intraluminal Support Junior for treatment of ruptured dissecting aneurysm located at proximal posterior inferior cerebellar artery
- Endovascular Surgery of Vertebral Artery Dissecting Aneurysm