Anat Cell Biol.
2021 Jun;54(2):165-177. 10.5115/acb.20.290.
Blood-brain barrier dysfunction in ischemic stroke and diabetes: the underlying link, mechanisms and future possible therapeutic targets
- Affiliations
-
- 1Department of Anatomy, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 2Department of Anatomy, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia
- 3Excellence in Osteology Research and Training Center (ORTC), Chiang Mai University, Chiang Mai, Thailand
- KMID: 2516900
- DOI: http://doi.org/10.5115/acb.20.290
Abstract
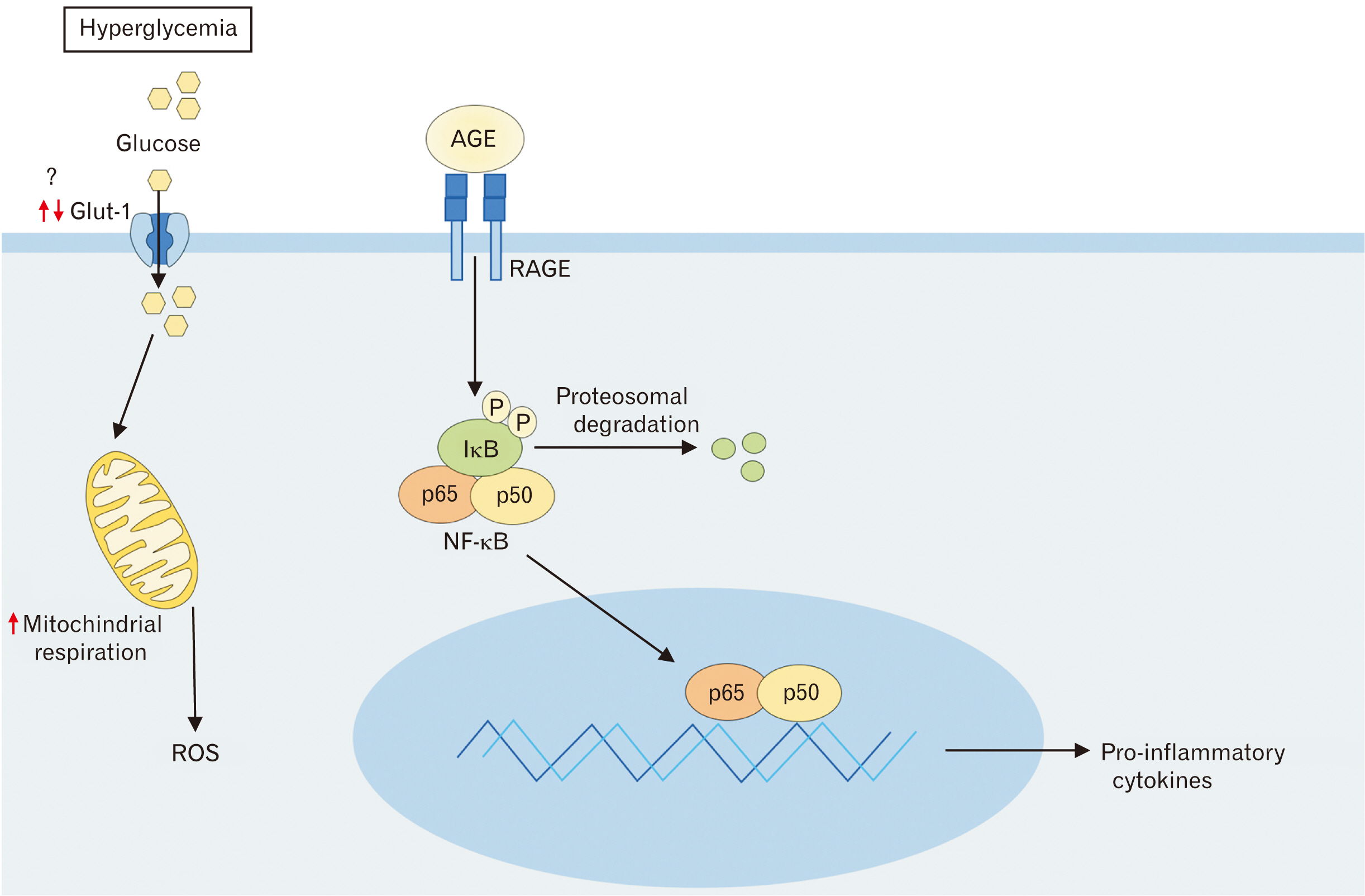
- Ischemic stroke caused by occlusion of cerebral artery is responsible for the majority of stroke that increases the morbidity and mortality worldwide. Diabetes mellitus (DM) is a crucial risk factor for ischemic stroke. Prolonged DM causes various microvascular and macrovascular changes, and blood-brain barrier (BBB) permeability that facilitates inflammatory response following stroke. In the acute phase following stroke, BBB disruption has been considered the initial step that induces neurological deficit and functional disabilities. Stroke outcomes are significantly worse among DM. In this article, we review stroke with diabetes-induce BBB damage, as well as underlying mechanism and possible therapeutic targets for stroke with diabetes.
Figure
Cited by 1 articles
-
The
in vitro analysis of migration and polarity of blastema cells in the extracellular matrix derived from bovine mesenteric in the presence of fibronectin
Kamelia Kohannezhad, Soroush Norouzi, Maryam Tafazoli, Safoura Soleymani, Nasser Mahdavi Shahri, Amin Tavassoli
Anat Cell Biol. 2022;55(2):229-238. doi: 10.5115/acb.21.233.
Reference
-
References
1. Goldstein LB, Adams R, Becker K, Furberg CD, Gorelick PB, Hademenos G, Hill M, Howard G, Howard VJ, Jacobs B, Levine SR, Mosca L, Sacco RL, Sherman DG, Wolf PA, del Zoppo GJ. 2001; Primary prevention of ischemic stroke: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Stroke. 32:280–99. DOI: 10.1161/01.STR.32.1.280. PMID: 11136952.2. Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. 2001; Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 32:2426–32. DOI: 10.1161/hs1001.096194. PMID: 11588337.3. Mankovsky BN, Ziegler D. 2004; Stroke in patients with diabetes mellitus. Diabetes Metab Res Rev. 20:268–87. DOI: 10.1002/dmrr.490. PMID: 15250030.
Article4. Megherbi SE, Milan C, Minier D, Couvreur G, Osseby GV, Tilling K, Di Carlo A, Inzitari D, Wolfe CD, Moreau T, Giroud M. European BIOMED Study of Stroke Care Group. 2003; Association between diabetes and stroke subtype on survival and functional outcome 3 months after stroke: data from the European BIOMED Stroke Project. Stroke. 34:688–94. DOI: 10.1161/01.STR.0000057975.15221.40. PMID: 12624292.
Article5. Yong M, Kaste M. 2008; Dynamic of hyperglycemia as a predictor of stroke outcome in the ECASS-II trial. Stroke. 39:2749–55. DOI: 10.1161/STROKEAHA.108.514307. PMID: 18703813.
Article6. Hawkins BT, Lundeen TF, Norwood KM, Brooks HL, Egleton RD. 2007; Increased blood-brain barrier permeability and altered tight junctions in experimental diabetes in the rat: contribution of hyperglycaemia and matrix metalloproteinases. Diabetologia. 50:202–11. DOI: 10.1007/s00125-006-0485-z. PMID: 17143608.
Article7. Horani MH, Mooradian AD. 2003; Effect of diabetes on the blood brain barrier. Curr Pharm Des. 9:833–40. DOI: 10.2174/1381612033455314. PMID: 12678883.
Article8. Serlin Y, Levy J, Shalev H. 2011; Vascular pathology and blood-brain barrier disruption in cognitive and psychiatric complications of type 2 diabetes mellitus. Cardiovasc Psychiatry Neurol. 2011:609202. DOI: 10.1155/2011/609202. PMID: 21350721. PMCID: PMC3042607.
Article9. Simpson IA, Appel NM, Hokari M, Oki J, Holman GD, Maher F, Koehler-Stec EM, Vannucci SJ, Smith QR. 1999; Blood-brain barrier glucose transporter: effects of hypo- and hyperglycemia revisited. J Neurochem. 72:238–47. DOI: 10.1046/j.1471-4159.1999.0720238.x. PMID: 9886075.10. Abdullahi W, Tripathi D, Ronaldson PT. 2018; Blood-brain barrier dysfunction in ischemic stroke: targeting tight junctions and transporters for vascular protection. Am J Physiol Cell Physiol. 315:C343–56. DOI: 10.1152/ajpcell.00095.2018. PMID: 29949404. PMCID: PMC6171039.
Article11. Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. 2010; Structure and function of the blood-brain barrier. Neurobiol Dis. 37:13–25. DOI: 10.1016/j.nbd.2009.07.030. PMID: 19664713.
Article12. Keaney J, Campbell M. 2015; The dynamic blood-brain barrier. FEBS J. 282:4067–79. DOI: 10.1111/febs.13412. PMID: 26277326.
Article13. Li AC, Thompson RP. 2003; Basement membrane components. J Clin Pathol. 56:885–7. DOI: 10.1136/jcp.56.12.885. PMID: 14645343. PMCID: PMC1770144.
Article14. Huber JD, Egleton RD, Davis TP. 2001; Molecular physiology and pathophysiology of tight junctions in the blood-brain barrier. Trends Neurosci. 24:719–25. DOI: 10.1016/S0166-2236(00)02004-X. PMID: 11718877.
Article15. Obermeier B, Verma A, Ransohoff RM. 2016; The blood-brain barrier. Handb Clin Neurol. 133:39–59. DOI: 10.1016/B978-0-444-63432-0.00003-7. PMID: 27112670.
Article16. Piccio L, Rossi B, Scarpini E, Laudanna C, Giagulli C, Issekutz AC, Vestweber D, Butcher EC, Constantin G. 2002; Molecular mechanisms involved in lymphocyte recruitment in inflamed brain microvessels: critical roles for P-selectin glycoprotein ligand-1 and heterotrimeric G(i)-linked receptors. J Immunol. 168:1940–9. DOI: 10.4049/jimmunol.168.4.1940. PMID: 11823530.
Article17. Gee JR, Keller JN. 2005; Astrocytes: regulation of brain homeostasis via apolipoprotein E. Int J Biochem Cell Biol. 37:1145–50. DOI: 10.1016/j.biocel.2004.10.004. PMID: 15778078.
Article18. Armulik A, Genové G, Mäe M, Nisancioglu MH, Wallgard E, Niaudet C, He L, Norlin J, Lindblom P, Strittmatter K, Johansson BR, Betsholtz C. 2010; Pericytes regulate the blood-brain barrier. Nature. 468:557–61. DOI: 10.1038/nature09522. PMID: 20944627.
Article19. Daneman R, Zhou L, Kebede AA, Barres BA. 2010; Pericytes are required for blood-brain barrier integrity during embryogenesis. Nature. 468:562–6. DOI: 10.1038/nature09513. PMID: 20944625. PMCID: PMC3241506.
Article20. Daneman R, Prat A. 2015; The blood-brain barrier. Cold Spring Harb Perspect Biol. 7:a020412. DOI: 10.1101/cshperspect.a020412. PMID: 25561720. PMCID: PMC4292164.
Article21. Nitta T, Hata M, Gotoh S, Seo Y, Sasaki H, Hashimoto N, Furuse M, Tsukita S. 2003; Size-selective loosening of the blood-brain barrier in claudin-5-deficient mice. J Cell Biol. 161:653–60. DOI: 10.1083/jcb.200302070. PMID: 12743111. PMCID: PMC2172943.
Article22. Liebner S, Corada M, Bangsow T, Babbage J, Taddei A, Czupalla CJ, Reis M, Felici A, Wolburg H, Fruttiger M, Taketo MM, von Melchner H, Plate KH, Gerhardt H, Dejana E. 2008; Wnt/beta-catenin signaling controls development of the blood-brain barrier. J Cell Biol. 183:409–17. DOI: 10.1083/jcb.200806024. PMID: 18955553. PMCID: PMC2575783.23. Saitou M, Furuse M, Sasaki H, Schulzke JD, Fromm M, Takano H, Noda T, Tsukita S. 2000; Complex phenotype of mice lacking occludin, a component of tight junction strands. Mol Biol Cell. 11:4131–42. DOI: 10.1091/mbc.11.12.4131. PMID: 11102513. PMCID: PMC15062.
Article24. Van Itallie CM, Anderson JM. 2013; Claudin interactions in and out of the tight junction. Tissue Barriers. 1:e25247. DOI: 10.4161/tisb.25247. PMID: 24665401. PMCID: PMC3875638.
Article25. Löscher W, Potschka H. 2005; Blood-brain barrier active efflux transporters: ATP-binding cassette gene family. NeuroRx. 2:86–98. DOI: 10.1602/neurorx.2.1.86. PMID: 15717060. PMCID: PMC539326.
Article26. Erdő F, Krajcsi P. 2019; Age-related functional and expressional changes in efflux pathways at the blood-brain barrier. Front Aging Neurosci. 11:196. DOI: 10.3389/fnagi.2019.00196. PMID: 31417399. PMCID: PMC6682691.
Article27. Shah K, Desilva S, Abbruscato T. 2012; The role of glucose transporters in brain disease: diabetes and Alzheimer's disease. Int J Mol Sci. 13:12629–55. DOI: 10.3390/ijms131012629. PMID: 23202918. PMCID: PMC3497292.
Article28. Luchsinger JA, Tang MX, Stern Y, Shea S, Mayeux R. 2001; Diabetes mellitus and risk of Alzheimer's disease and dementia with stroke in a multiethnic cohort. Am J Epidemiol. 154:635–41. DOI: 10.1093/aje/154.7.635. PMID: 11581097.
Article29. Prasad S, Sajja RK, Naik P, Cucullo L. 2014; Diabetes mellitus and blood-brain barrier dysfunction: an overview. J Pharmacovigil. 2:125. DOI: 10.4172/2329-6887.1000125. PMID: 25632404. PMCID: PMC4306190.30. Chen M, Zheng H, Xu M, Zhao L, Zhang Q, Song J, Zhao Z, Lu S, Weng Q, Wu X, Yang W, Fan X, Gao H, Ji J. 2019; Changes in hepatic metabolic profile during the evolution of STZ-induced diabetic rats via an 1H NMR-based metabonomic investigation. Biosci Rep. 39:BSR20181379. DOI: 10.1042/BSR20181379. PMID: 30918104. PMCID: PMC6481239.
Article31. Jurysta C, Nicaise C, Giroix MH, Cetik S, Malaisse WJ, Sener A. 2013; Comparison of GLUT1, GLUT2, GLUT4 and SGLT1 mRNA expression in the salivary glands and six other organs of control, streptozotocin-induced and Goto-Kakizaki diabetic rats. Cell Physiol Biochem. 31:37–43. DOI: 10.1159/000343347. PMID: 23343648.
Article32. Younessi P, Yoonessi A. 2011; Advanced glycation end-products and their receptor-mediated roles: inflammation and oxidative stress. Iran J Med Sci. 36:154–66. PMID: 23358382. PMCID: PMC3556769.33. Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. 2004; Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Diabetes. 53:2079–86. DOI: 10.2337/diabetes.53.8.2079. PMID: 15277389.
Article34. Volpe CMO, Villar-Delfino PH, Dos Anjos PMF, Nogueira-Machado JA. 2018; Cellular death, reactive oxygen species (ROS) and diabetic complications. Cell Death Dis. 9:119. DOI: 10.1038/s41419-017-0135-z. PMID: 29371661. PMCID: PMC5833737.
Article35. World Health Organization (WHO). 2008. The Global burden of disease: 2004 update. World Health Organization;Geneva:36. Tun NN, Arunagirinathan G, Munshi SK, Pappachan JM. 2017; Diabetes mellitus and stroke: a clinical update. World J Diabetes. 8:235–48. DOI: 10.4239/wjd.v8.i6.235. PMID: 28694925. PMCID: PMC5483423.
Article37. Fujimura M, Gasche Y, Morita-Fujimura Y, Massengale J, Kawase M, Chan PH. 1999; Early appearance of activated matrix metalloproteinase-9 and blood-brain barrier disruption in mice after focal cerebral ischemia and reperfusion. Brain Res. 842:92–100. DOI: 10.1016/S0006-8993(99)01843-0. PMID: 10526099.
Article38. Fukuda AM, Badaut J. 2012; Aquaporin 4: a player in cerebral edema and neuroinflammation. J Neuroinflammation. 9:279. DOI: 10.1186/1742-2094-9-279. PMID: 23270503. PMCID: PMC3552817.
Article39. Candelario-Jalil E, Yang Y, Rosenberg GA. 2009; Diverse roles of matrix metalloproteinases and tissue inhibitors of metalloproteinases in neuroinflammation and cerebral ischemia. Neuroscience. 158:983–94. DOI: 10.1016/j.neuroscience.2008.06.025. PMID: 18621108. PMCID: PMC3584171.
Article40. Chodobski A, Zink BJ, Szmydynger-Chodobska J. 2011; Blood-brain barrier pathophysiology in traumatic brain injury. Transl Stroke Res. 2:492–516. DOI: 10.1007/s12975-011-0125-x. PMID: 22299022. PMCID: PMC3268209.
Article41. Uyttenboogaart M, Koch MW, Stewart RE, Vroomen PC, Luijckx GJ, De Keyser J. 2007; Moderate hyperglycaemia is associated with favourable outcome in acute lacunar stroke. Brain. 130(Pt 6):1626–30. DOI: 10.1093/brain/awm087. PMID: 17525141.
Article42. Ramasamy R, Yan SF, Schmidt AM. 2011; Receptor for AGE (RAGE): signaling mechanisms in the pathogenesis of diabetes and its complications. Ann N Y Acad Sci. 1243:88–102. DOI: 10.1111/j.1749-6632.2011.06320.x. PMID: 22211895. PMCID: PMC4501013.
Article43. Song EC, Chu K, Jeong SW, Jung KH, Kim SH, Kim M, Yoon BW. 2003; Hyperglycemia exacerbates brain edema and perihematomal cell death after intracerebral hemorrhage. Stroke. 34:2215–20. DOI: 10.1161/01.STR.0000088060.83709.2C. PMID: 12907821.
Article44. Bruno A, Levine SR, Frankel MR, Brott TG, Lin Y, Tilley BC, Lyden PD, Broderick JP, Kwiatkowski TG, Fineberg SE. NINDS rt-PA Stroke Study Group. 2002; Admission glucose level and clinical outcomes in the NINDS rt-PA Stroke Trial. Neurology. 59:669–74. DOI: 10.1212/WNL.59.5.669. PMID: 12221155.
Article45. Barreras A, Gurk-Turner C. 2003; Angiotensin II receptor blockers. Proc (Bayl Univ Med Cent). 16:123–6. DOI: 10.1080/08998280.2003.11927893. PMID: 16278727. PMCID: PMC1200815.
Article46. O'Keefe JH, Wetzel M, Moe RR, Bronsnahan K, Lavie CJ. 2001; Should an angiotensin-converting enzyme inhibitor be standard therapy for patients with atherosclerotic disease? J Am Coll Cardiol. 37:1–8. DOI: 10.1016/S0735-1097(00)01044-5. PMID: 11153722.47. Schiffrin EL, Park JB, Intengan HD, Touyz RM. 2000; Correction of arterial structure and endothelial dysfunction in human essential hypertension by the angiotensin receptor antagonist losartan. Circulation. 101:1653–9. DOI: 10.1161/01.CIR.101.14.1653. PMID: 10758046.
Article48. Ido A, Hasebe N, Takeuchi T, Kikuchi K. 2003; Effects of temocapril and olmesartan on myocardial sympathetic nervous activity and fatty acid metabolism in rats with chronic beta-adrenergic stimulation. J Cardiovasc Pharmacol. 41 Suppl 1:S133–7. PMID: 12688410.49. Yamaguchi K, Ura N, Murakami H, Togashi N, Hyakukoku M, Higashiura K, Shimamoto K. 2005; Olmesartan ameliorates insulin sensitivity by modulating tumor necrosis factor-alpha and cyclic AMP in skeletal muscle. Hypertens Res. 28:773–8. DOI: 10.1291/hypres.28.773. PMID: 16419651.
Article50. Matsumura T, Kinoshita H, Ishii N, Fukuda K, Motoshima H, Senokuchi T, Taketa K, Kawasaki S, Nishimaki-Mogami T, Kawada T, Nishikawa T, Araki E. 2011; Telmisartan exerts antiatherosclerotic effects by activating peroxisome proliferator-activated receptor-γ in macrophages. Arterioscler Thromb Vasc Biol. 31:1268–75. DOI: 10.1161/ATVBAHA.110.222067. PMID: 21474824.
Article51. Tan XY, Hu JB. 2016; ACEIs/ARBs for the prevention of type 2 diabetes in patients with cardiovascular diseases: a systematic review and meta-analysis. Int J Clin Exp Med. 9:7624–37.52. Kuwashiro T, Kamouchi M, Ago T, Hata J, Sugimori H, Kitazono T. 2012; The factors associated with a functional outcome after ischemic stroke in diabetic patients: the Fukuoka Stroke Registry. J Neurol Sci. 313:110–4. DOI: 10.1016/j.jns.2011.09.012. PMID: 21992812.
Article53. Baird TA, Parsons MW, Phan T, Butcher KS, Desmond PM, Tress BM, Colman PG, Chambers BR, Davis SM. 2003; Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke. 34:2208–14. DOI: 10.1161/01.STR.0000085087.41330.FF. PMID: 12893952.
Article54. Fuentes B, Castillo J, San José B, Leira R, Serena J, Vivancos J, Dávalos A, Nuñez AG, Egido J, Díez-Tejedor E. Stroke Project of the Cerebrovascular Diseases Study Group, Spanish Society of Neurology. 2009; The prognostic value of capillary glucose levels in acute stroke: the GLycemia in acute stroke (GLIAS) study. Stroke. 40:562–8. DOI: 10.1161/STROKEAHA.108.519926. PMID: 19095970.55. Boussageon R, Bejan-Angoulvant T, Saadatian-Elahi M, Lafont S, Bergeonneau C, Kassaï B, Erpeldinger S, Wright JM, Gueyffier F, Cornu C. 2011; Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ. 343:d4169. DOI: 10.1136/bmj.d4169. PMID: 21791495. PMCID: PMC3144314.
Article56. Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, Zieve FJ, Marks J, Davis SN, Hayward R, Warren SR, Goldman S, McCarren M, Vitek ME, Henderson WG, Huang GD. 2009; Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 360:129–39. DOI: 10.1056/NEJMoa0808431. PMID: 19092145.
Article57. Gerstein HC, Miller ME, Genuth S, Ismail-Beigi F, Buse JB, Goff DC Jr, Probstfield JL, Cushman WC, Ginsberg HN, Bigger JT, Grimm RH Jr, Byington RP, Rosenberg YD, Friedewald WT. 2011; Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 364:818–28. DOI: 10.1056/NEJMoa1006524. PMID: 21366473. PMCID: PMC4083508.
Article58. Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal TP, Hemmingsen C, Wetterslev J. 2013; Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database Syst Rev. (11):CD008143. DOI: 10.1002/14651858.CD008143.pub3. PMID: 26222248.
Article59. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. 2008; Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 358:2560–72. DOI: 10.1056/NEJMoa0802987. PMID: 18539916.60. Bonnet F, Scheen AJ. 2017; Impact of glucose-lowering therapies on risk of stroke in type 2 diabetes. Diabetes Metab. 43:299–313. DOI: 10.1016/j.diabet.2017.04.004. PMID: 28522196.
Article61. Castilla-Guerra L, Fernandez-Moreno MDC, Leon-Jimenez D, Carmona-Nimo E. 2018; Antidiabetic drugs and stroke risk. Current evidence. Eur J Intern Med. 48:1–5. DOI: 10.1016/j.ejim.2017.09.019. PMID: 28939005.
Article62. Lee JC, Won MH. 2014; Neuroprotection of antioxidant enzymes against transient global cerebral ischemia in gerbils. Anat Cell Biol. 47:149–56. DOI: 10.5115/acb.2014.47.3.149. PMID: 25276473. PMCID: PMC4178189.
Article63. Li H, Luo Y, Yang P, Liu J. 2019; Hydrogen as a complementary therapy against ischemic stroke: a review of the evidence. J Neurol Sci. 396:240–6. DOI: 10.1016/j.jns.2018.11.004. PMID: 30529801.
Article64. Shinohara Y, Saito I, Kobayashi S, Uchiyama S. 2009; Edaravone (radical scavenger) versus sodium ozagrel (antiplatelet agent) in acute noncardioembolic ischemic stroke (EDO trial). Cerebrovasc Dis. 27:485–92. DOI: 10.1159/000210190. PMID: 19321945.
Article65. Hu Q, Manaenko A, Bian H, Guo Z, Huang JL, Guo ZN, Yang P, Tang J, Zhang JH. 2017; Hyperbaric oxygen reduces infarction volume and hemorrhagic transformation through ATP/NAD+/Sirt1 pathway in hyperglycemic middle cerebral artery occlusion rats. Stroke. 48:1655–64. DOI: 10.1161/STROKEAHA.116.015753. PMID: 28495827. PMCID: PMC5489129.66. Ning R, Venkat P, Chopp M, Zacharek A, Yan T, Cui X, Seyfried D, Chen J. 2017; D-4F increases microRNA-124a and reduces neuroinflammation in diabetic stroke rats. Oncotarget. 8:95481–94. DOI: 10.18632/oncotarget.20751. PMID: 29221142. PMCID: PMC5707036.
Article67. Iwasawa E, Ichijo M, Ishibashi S, Yokota T. 2016; Acute development of collateral circulation and therapeutic prospects in ischemic stroke. Neural Regen Res. 11:368–71. DOI: 10.4103/1673-5374.179033. PMID: 27127459. PMCID: PMC4828985.
Article68. Wang J, Hu W, Li L, Huang X, Liu Y, Wang D, Teng L. 2017; Antidiabetic activities of polysaccharides separated from Inonotus obliquus via the modulation of oxidative stress in mice with streptozotocin-induced diabetes. PLoS One. 12:e0180476. DOI: 10.1371/journal.pone.0180476. PMID: 28662169. PMCID: PMC5491251.
Article69. Hong P, Gu RN, Li FX, Xiong XX, Liang WB, You ZJ, Zhang HF. 2019; NLRP3 inflammasome as a potential treatment in ischemic stroke concomitant with diabetes. J Neuroinflammation. 16:121. DOI: 10.1186/s12974-019-1498-0. PMID: 31174550. PMCID: PMC6554993.
Article70. Hu J, Liu B, Zhao Q, Jin P, Hua F, Zhang Z, Liu Y, Zan K, Cui G, Ye X. 2016; Bone marrow stromal cells inhibits HMGB1-mediated inflammation after stroke in type 2 diabetic rats. Neuroscience. 324:11–9. DOI: 10.1016/j.neuroscience.2016.02.058. PMID: 26946264.
Article71. Xiang J, Hu J, Shen T, Liu B, Hua F, Zan K, Zu J, Cui G, Ye X. 2017; Bone marrow mesenchymal stem cells-conditioned medium enhances vascular remodeling after stroke in type 2 diabetic rats. Neurosci Lett. 644:62–6. DOI: 10.1016/j.neulet.2017.02.040. PMID: 28219791.
Article72. Venkat P, Yan T, Chopp M, Zacharek A, Ning R, Van Slyke P, Dumont D, Landschoot-Ward J, Liang L, Chen J. 2018; Angiopoietin-1 mimetic peptide promotes neuroprotection after stroke in type 1 diabetic rats. Cell Transplant. 27:1744–52. DOI: 10.1177/0963689718791568. PMID: 30124060. PMCID: PMC6300775.
Article73. Nakagawa S, Aruga J. 2020; Sphingosine 1-phosphate signaling is involved in impaired blood-brain barrier function in ischemia-reperfusion injury. Mol Neurobiol. 57:1594–606. DOI: 10.1007/s12035-019-01844-x. PMID: 31802363.
Article74. Sanchez T. 2016; Sphingosine-1-phosphate signaling in endothelial disorders. Curr Atheroscler Rep. 18:31. DOI: 10.1007/s11883-016-0586-1. PMID: 27115142.
Article75. Li YJ, Shi SX, Liu Q, Shi FD, Gonzales RJ. 2020; Targeted role for sphingosine-1-phosphate receptor 1 in cerebrovascular integrity and inflammation during acute ischemic stroke. Neurosci Lett. 735:135160. DOI: 10.1016/j.neulet.2020.135160. PMID: 32561451.
Article76. Kurano M, Tsukamoto K, Shimizu T, Kassai H, Nakao K, Aiba A, Hara M, Yatomi Y. 2020; Protection against insulin resistance by apolipoprotein M/sphingosine-1-phosphate. Diabetes. 69:867–81. DOI: 10.2337/db19-0811. PMID: 31915150.
Article77. Li S, Wang N, Guo X, Li J, Zhang T, Ren G, Li D. 2018; Fibroblast growth factor 21 regulates glucose metabolism in part by reducing renal glucose reabsorption. Biomed Pharmacother. 108:355–66. DOI: 10.1016/j.biopha.2018.09.078. PMID: 30227329.
Article78. Tezze C, Romanello V, Sandri M. 2019; FGF21 as modulator of metabolism in health and disease. Front Physiol. 10:419. DOI: 10.3389/fphys.2019.00419. PMID: 31057418. PMCID: PMC6478891.
Article79. Woo YC, Xu A, Wang Y, Lam KS. 2013; Fibroblast growth factor 21 as an emerging metabolic regulator: clinical perspectives. Clin Endocrinol (Oxf). 78:489–96. DOI: 10.1111/cen.12095. PMID: 23134073.
Article80. Wang D, Liu F, Zhu L, Lin P, Han F, Wang X, Tan X, Lin L, Xiong Y. 2020; FGF21 alleviates neuroinflammation following ischemic stroke by modulating the temporal and spatial dynamics of microglia/macrophages. J Neuroinflammation. 17:257. DOI: 10.1186/s12974-020-01921-2. PMID: 32867781. PMCID: PMC7457364.
Article81. Jiang Y, Lin L, Liu N, Wang Q, Yuan J, Li Y, Chung KK, Guo S, Yu Z, Wang X. 2020; FGF21 protects against aggravated blood-brain barrier disruption after ischemic focal stroke in diabetic db/db male mice via cerebrovascular PPARγ activation. Int J Mol Sci. 21:824. DOI: 10.3390/ijms21030824. PMID: 32012810. PMCID: PMC7037567.
Article82. Zhong C, Yang J, Xu T, Xu T, Peng Y, Wang A, Wang J, Peng H, Li Q, Ju Z, Geng D, Zhang Y, He J. 2017; Serum matrix metalloproteinase-9 levels and prognosis of acute ischemic stroke. Neurology. 89:805–12. DOI: 10.1212/WNL.0000000000004257. PMID: 28747453. PMCID: PMC5580861.
Article83. Darsalia V, Hua S, Larsson M, Mallard C, Nathanson D, Nyström T, Sjöholm Å, Johansson ME, Patrone C. 2014; Exendin-4 reduces ischemic brain injury in normal and aged type 2 diabetic mice and promotes microglial M2 polarization. PLoS One. 9:e103114. DOI: 10.1371/journal.pone.0103114. PMID: 25101679. PMCID: PMC4125154.
Article84. Chen X, Jiang H. 2019; Tau as a potential therapeutic target for ischemic stroke. Aging (Albany NY). 11:12827–43. DOI: 10.18632/aging.102547. PMID: 31841442. PMCID: PMC6949092.
Article85. Tuo QZ, Lei P, Jackman KA, Li XL, Xiong H, Li XL, Liuyang ZY, Roisman L, Zhang ST, Ayton S, Wang Q, Crouch PJ, Ganio K, Wang XC, Pei L, Adlard PA, Lu YM, Cappai R, Wang JZ, Liu R, Bush AI. 2017; Tau-mediated iron export prevents ferroptotic damage after ischemic stroke. Mol Psychiatry. 22:1520–30. DOI: 10.1038/mp.2017.171. PMID: 28886009.
Article86. Bi M, Gladbach A, van Eersel J, Ittner A, Przybyla M, van Hummel A, Chua SW, van der Hoven J, Lee WS, Müller J, Parmar J, Jonquieres GV, Stefen H, Guccione E, Fath T, Housley GD, Klugmann M, Ke YD, Ittner LM. 2017; Tau exacerbates excitotoxic brain damage in an animal model of stroke. Nat Commun. 8:473. DOI: 10.1038/s41467-017-00618-0. PMID: 28883427. PMCID: PMC5589746.
Article87. Raz L, Bhaskar K, Weaver J, Marini S, Zhang Q, Thompson JF, Espinoza C, Iqbal S, Maphis NM, Weston L, Sillerud LO, Caprihan A, Pesko JC, Erhardt EB, Rosenberg GA. 2019; Hypoxia promotes tau hyperphosphorylation with associated neuropathology in vascular dysfunction. Neurobiol Dis. 126:124–36. DOI: 10.1016/j.nbd.2018.07.009. PMID: 30010004. PMCID: PMC6347559.
Article88. Zhang T, Pan BS, Sun GC, Sun X, Sun FY. 2010; Diabetes synergistically exacerbates poststroke dementia and tau abnormality in brain. Neurochem Int. 56:955–61. DOI: 10.1016/j.neuint.2010.04.003. PMID: 20398714.
Article89. Hesse C, Rosengren L, Andreasen N, Davidsson P, Vanderstichele H, Vanmechelen E, Blennow K. 2001; Transient increase in total tau but not phospho-tau in human cerebrospinal fluid after acute stroke. Neurosci Lett. 297:187–90. DOI: 10.1016/S0304-3940(00)01697-9.
Article90. De Vos A, Bjerke M, Brouns R, De Roeck N, Jacobs D, Van den Abbeele L, Guldolf K, Zetterberg H, Blennow K, Engelborghs S, Vanmechelen E. 2017; Neurogranin and tau in cerebrospinal fluid and plasma of patients with acute ischemic stroke. BMC Neurol. 17:170. DOI: 10.1186/s12883-017-0945-8. PMID: 28854881. PMCID: PMC5577791.
Article91. Xia M, Ye Z, Shi Y, Zhou L, Hua Y. 2018; Curcumin improves diabetes mellitus-associated cerebral infarction by increasing the expression of GLUT1 and GLUT3. Mol Med Rep. 17:1963–9. DOI: 10.3892/mmr.2017.8085.
Article92. Kuhad A, Chopra K. 2008; Effect of sesamol on diabetes-associated cognitive decline in rats. Exp Brain Res. 185:411–20. DOI: 10.1007/s00221-007-1166-y. PMID: 17955223.
Article93. Zhang L, Kan ZC, Zhang XL, Fang H, Jiang WL. 2014; 8-O-acetyl shanzhiside methylester attenuates cerebral ischaemia/reperfusion injury through an anti-inflammatory mechanism in diabetic rats. Basic Clin Pharmacol Toxicol. 115:481–7. DOI: 10.1111/bcpt.12266. PMID: 24823762.
Article94. Luan H, Kan Z, Xu Y, Lv C, Jiang W. 2013; Rosmarinic acid protects against experimental diabetes with cerebral ischemia: relation to inflammation response. J Neuroinflammation. 10:28. DOI: 10.1186/1742-2094-10-28. PMID: 23414442. PMCID: PMC3614882.
Article95. Kim JH, Lee NS, Jeong YG, Lee JH, Kim EJ, Han SY. 2012; Protective efficacy of an Ecklonia cava extract used to treat transient focal ischemia of the rat brain. Anat Cell Biol. 45:103–13. DOI: 10.5115/acb.2012.45.2.103. PMID: 22822465. PMCID: PMC3398172.96. Yoon JY, Choi H, Jun HS. 2017; The effect of phloroglucinol, a component of Ecklonia cava extract, on hepatic glucose production. Mar Drugs. 15:106. DOI: 10.3390/md15040106. PMID: 28379184. PMCID: PMC5408252.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Loss of Integrity: Impairment of the Blood-brain Barrier in Heavy Metal-associated Ischemic Stroke
- Glial and Vascular Cell Regulation of the Blood-Brain Barrier in Diabetes
- tPA Helpers in the Treatment of Acute Ischemic Stroke: Are They Ready for Clinical Use?
- The Migraine-Stroke Connection
- Brain Abscess Developed on the Lesion Site of Previous Ischemic Stroke