J Korean Assoc Oral Maxillofac Surg.
2021 Apr;47(2):120-127. 10.5125/jkaoms.2021.47.2.120.
Sequential treatment from mandibulectomy to reconstruction on mandibular oral cancer – Case review I: mandibular ramus and angle lesion of primary intraosseous squamous cell carcinoma
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry, Pusan National University, Yangsan, Korea
- KMID: 2515310
- DOI: http://doi.org/10.5125/jkaoms.2021.47.2.120
Abstract
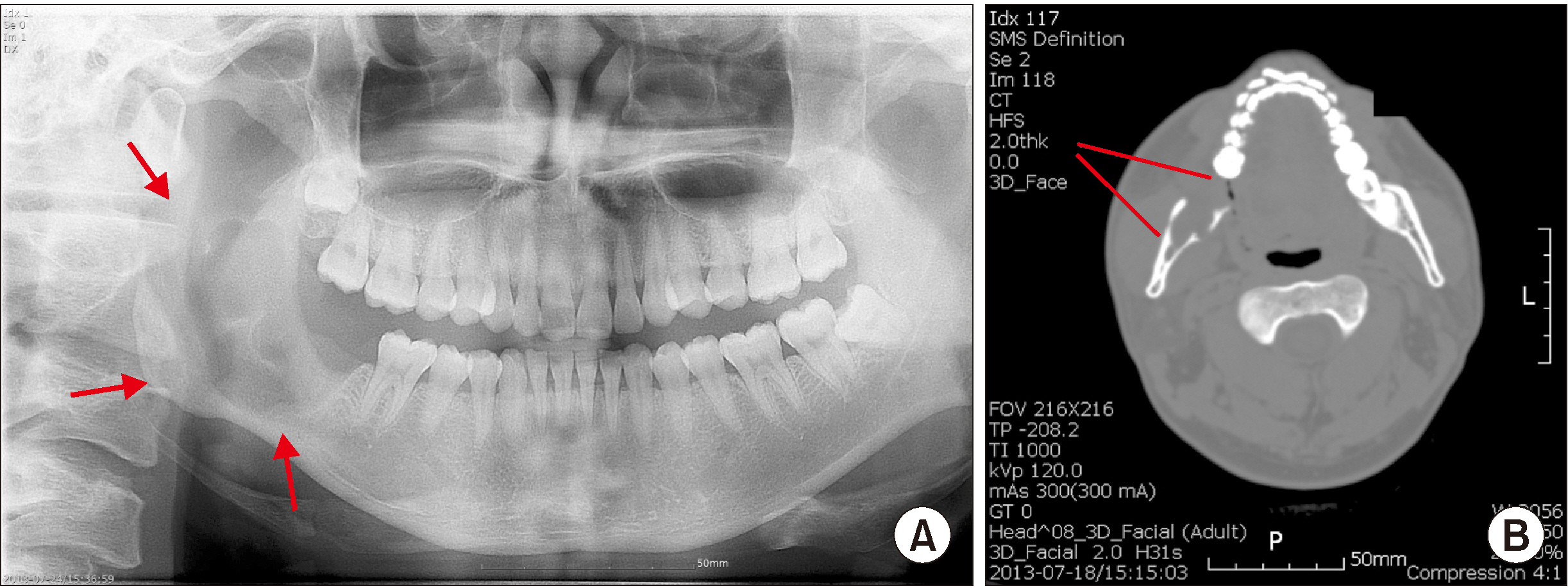
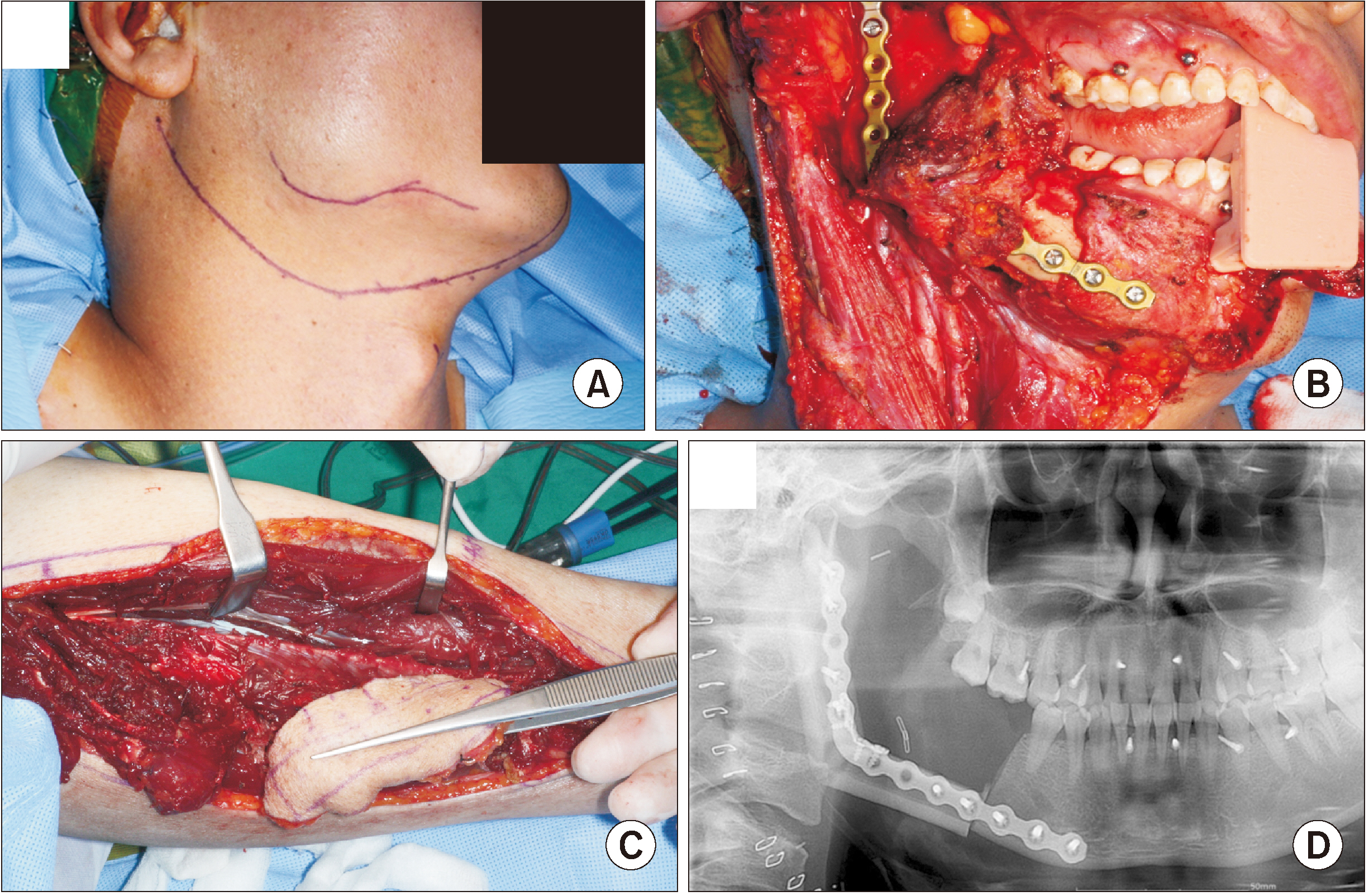
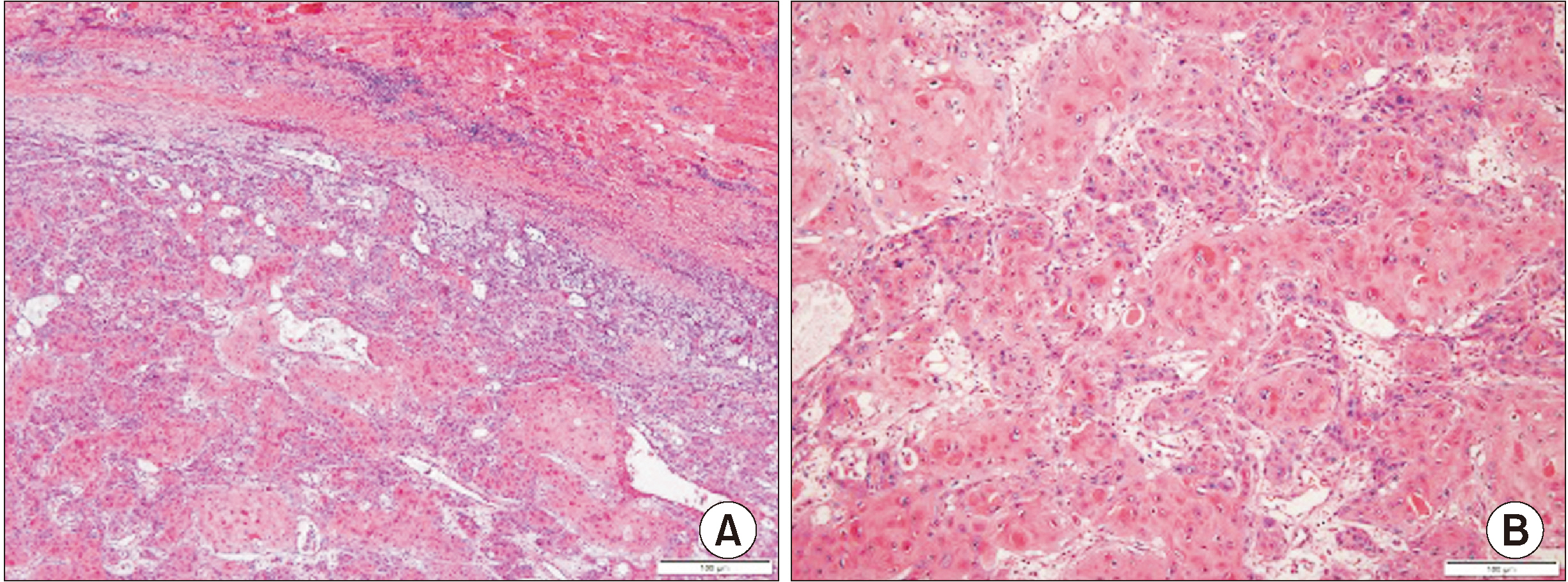
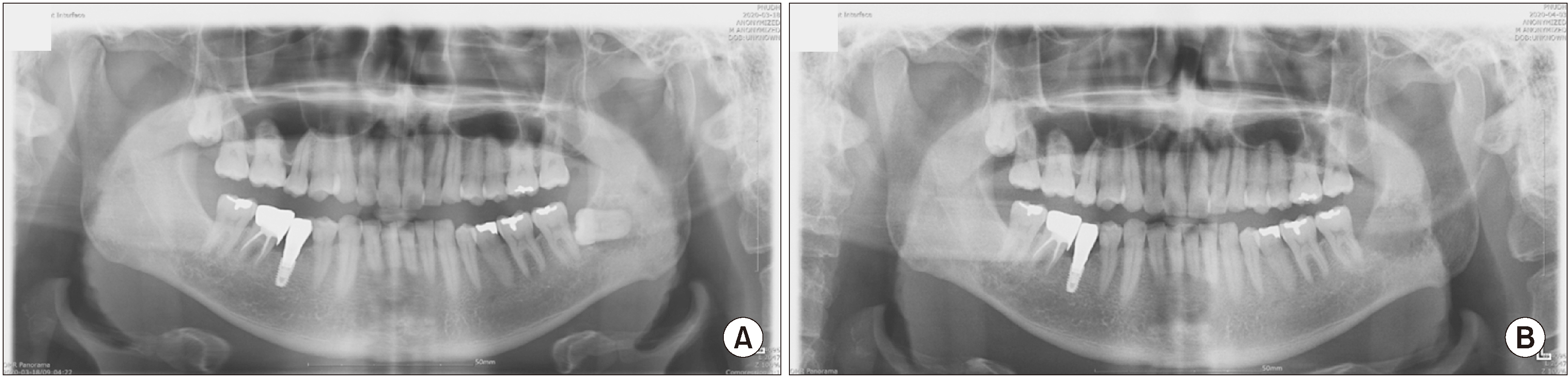
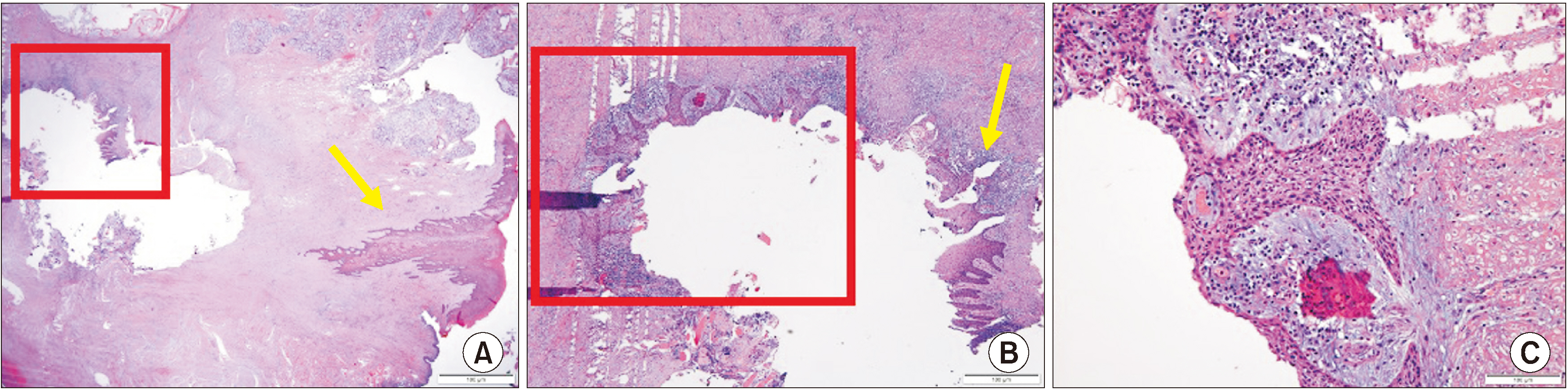
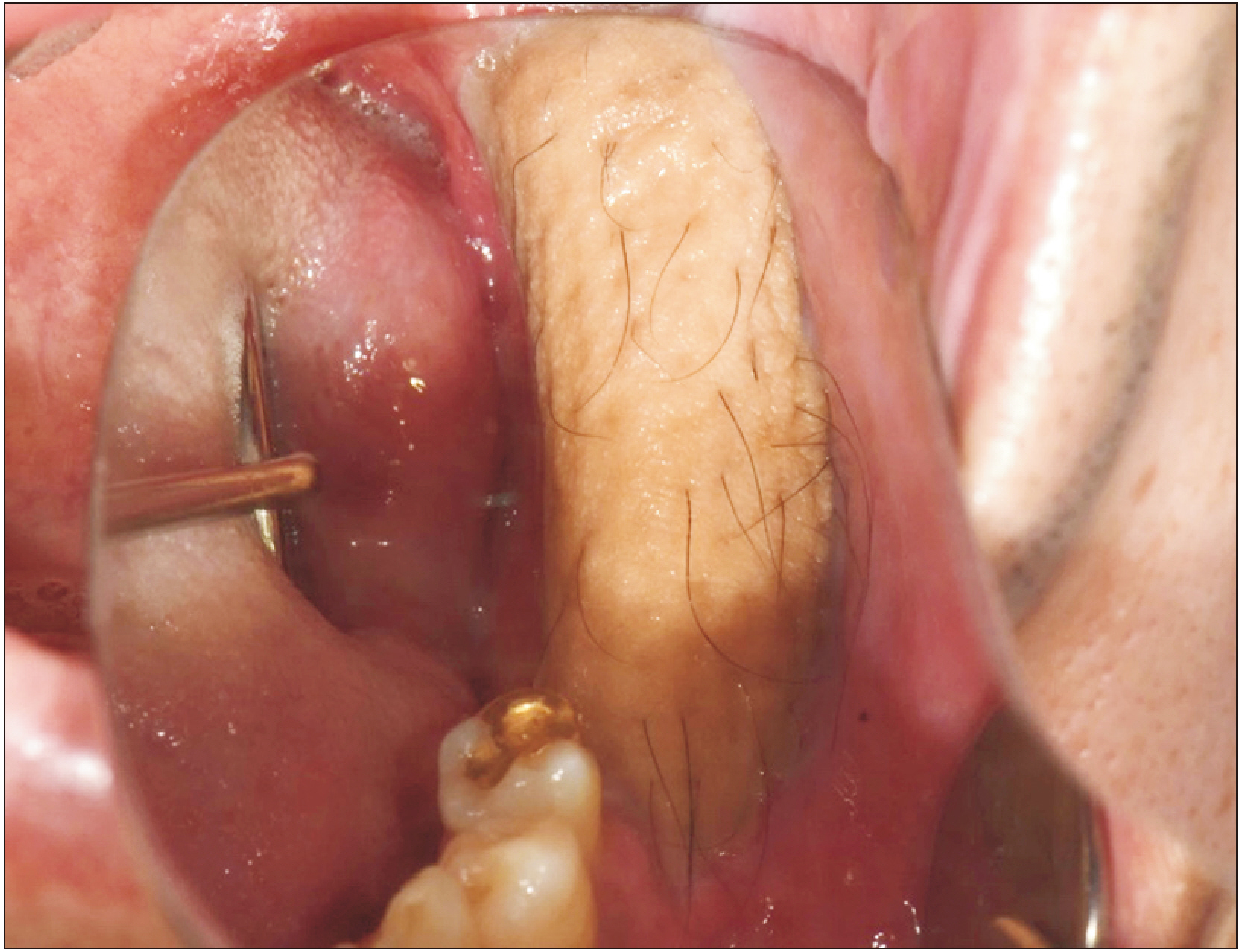
- Primary intraosseous squamous cell carcinoma (PIOSCC) is very rare type of squamous cell carcinoma (SCC) that occurs within the jaw and arises from remnants of odontogenic epithelium with no connection to the oral mucosa. This study reports two cases of PIOSCC of the mandible. Reported in this article are two cases of PIOSCC of the mandible that were treated with resection and reconstruction using a fibular free flap. The first case was a 36-year-old male patient who complained of right mandibular pain. Computed tomography (CT) and panoramic radiograph revealed a large radiolucency in the mandibular ramus area. At first, an odontogenic keratocyst was tentatively diagnosed, and an excision procedure was carried out at another clinic. A final biopsy after cyst enucleation revealed well-differentiated SCC, so we proceeded with segmental mandibulectomy and reconstruction using a fibular free flap. The second case was a 48-year-old male patient with left mandibular pain. CT and panoramic radiograph revealed irregular radiolucency in the mandibular angle area near tooth #38. At first, osteomyelitis was tentatively diagnosed, and a curettage was carried out. A later biopsy revealed well-differentiated SCC, so segmental mandibulectomy and reconstruction with a fibular free flap were secondarily performed. Our two cases have had no recurrence. The facial appearance of both patients is satisfactory, and the neo-mandibular body created using a fibular bone transfer displays adequate bony volume.
Figure
Reference
-
References
1. Bodner L, Manor E, Shear M, van der Waal I. 2011; Primary intraosseous squamous cell carcinoma arising in an odontogenic cyst: a clinicopathologic analysis of 116 reported cases. J Oral Pathol Med. 40:733–8. https://doi.org/10.1111/j.1600-0714.2011.01058.x . DOI: 10.1111/j.1600-0714.2011.01058.x. PMID: 21689161.
Article2. Shear M. 1969; Primary intra-alveolar epidermoid carcinoma of the jaw. J Pathol. 97:645–51. https://doi.org/10.1002/path.1710970409 . DOI: 10.1002/path.1710970409. PMID: 5354042.
Article3. Chaisuparat R, Coletti D, Kolokythas A, Ord RA, Nikitakis NG. 2006; Primary intraosseous odontogenic carcinoma arising in an odontogenic cyst or de novo: a clinicopathologic study of six new cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 101:194–200. https://doi.org/10.1016/j.tripleo.2005.03.037 . DOI: 10.1016/j.tripleo.2005.03.037. PMID: 16448921.
Article4. McGowan RH. 1980; Primary intra-alveolar carcinoma. A difficult diagnosis. Br J Oral Surg. 18:259–65. https://doi.org/10.1016/0007-117x(80)90071-2 . DOI: 10.1016/0007-117x(80)90071-2. PMID: 6934823.
Article5. Thomas G, Pandey M, Mathew A, Abraham EK, Francis A, Somanathan T, et al. 2001; Primary intraosseous carcinoma of the jaw: pooled analysis of world literature and report of two new cases. Int J Oral Maxillofac Surg. 30:349–55. https://doi.org/10.1054/ijom.2001.0069 . DOI: 10.1054/ijom.2001.0069. PMID: 11518362.
Article6. Huang JW, Luo HY, Li Q, Li TJ. 2009; Primary intraosseous squamous cell carcinoma of the jaws. Clinicopathologic presentation and prognostic factors. Arch Pathol Lab Med. 133:1834–40. https://doi.org/10.1043/1543-2165-133.11.1834 . DOI: 10.1043/1543-2165-133.11.1834. PMID: 19886720.
Article7. Williams MD. 2017; Update from the 4th edition of the World Health Organization Classification of Head and Neck Tumours: mucosal melanomas. Head Neck Pathol. 11:110–7. https://doi.org/10.1007/s12105-017-0789-y . DOI: 10.1007/s12105-017-0789-y. PMID: 28247222. PMCID: PMC5340730.
Article8. Sharma M, Wakure A, Thankappan K, Mathew J, Jairaj D, Dudipala RR, et al. 2015; Anatomic basis for an algorithmic approach for free fibula flap donor side selection in composite oro-mandibular defects. Indian J Plast Surg. 48:43–7. https://doi.org/10.4103/0970-0358.155268 . DOI: 10.4103/0970-0358.155268. PMID: 25991885. PMCID: PMC4413489.
Article9. Thakur A, Tupkari JV, Joy T, Gogri AA. 2017; Primary intraosseous squamous cell carcinoma - a rare odontogenic malignancy. J Oral Maxillofac Pathol. 21:320. https://doi.org/10.4103/jomfp.JOMFP_25_16 . DOI: 10.4103/jomfp.JOMFP_25_16. PMID: 28932052. PMCID: PMC5596693.
Article10. Suei Y, Taguchi A, Tanimoto K. 2004; Recommendation of modified classification for odontogenic carcinomas. Med Hypotheses. 62:382–6. https://doi.org/10.1016/j.mehy.2003.11.010 . DOI: 10.1016/j.mehy.2003.11.010. PMID: 14975508.
Article11. Elzay RP. 1982; Primary intraosseous carcinoma of the jaws. Review and update of odontogenic carcinomas. Oral Surg Oral Med Oral Pathol. 54:299–303. https://doi.org/10.1016/0030-4220(82)90099-8 . DOI: 10.1016/0030-4220(82)90099-8. PMID: 6957827.
Article12. Dai YL, King AD. 2018; State of the art MRI in head and neck cancer. Clin Radiol. 73:45–59. https://doi.org/10.1016/j.crad.2017.05.020 . DOI: 10.1016/j.crad.2017.05.020. PMID: 28655406.
Article13. Wenguang X, Hao S, Xiaofeng Q, Zhiyong W, Yufeng W, Qingang H, et al. 2016; Prognostic factors of primary intraosseous squamous cell carcinoma (PIOSCC): a retrospective review. PLoS One. 11:e0153646. https://doi.org/10.1371/journal.pone.0153646 . DOI: 10.1371/journal.pone.0153646. PMID: 27074366. PMCID: PMC4830592.
Article14. de Morais EF, Carlan LM, de Farias Morais HG, Pinheiro JC, Martins HDD, Barboza CAG, et al. 2020; Primary intraosseous squamous cell carcinoma involving the jaw bones: a systematic review and update. Head Neck Pathol. https://doi.org/10.1007/s12105-020-01234-z [Epub ahead of print]. DOI: 10.1007/s12105-020-01234-z. PMID: 33044723.
Article15. Dimitrakopoulos I, Psomaderis K, Asimaki A, Papaemanouel S, Karakasis D. 2005; Primary de novo intraosseous carcinoma: report of two cases. J Oral Maxillofac Surg. 63:1227–30. https://doi.org/10.1016/j.joms.2005.04.009 . DOI: 10.1016/j.joms.2005.04.009. PMID: 16094596.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sequential treatment from mandibulectomy to reconstruction on mandibular oral cancer – Case review II: mandibular anterior and the floor of the mouth lesion of basaloid squamous cell carcinoma and clear cell odontogenic carcinoma
- Mandibular intraosseous squamous cell carcinoma lesion associated with odontogenic keratocyst: a case report
- Primary intraosseous carcinoma(PIOC) on mandible: Case Report
- Delayed diagnosis of a primary intraosseous squamous cell carcinoma: A case report
- Reconstruction of extensive mandibular defects using deep circumflex iliac artery flap surgery and 3D-printed guides: a case report