Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):62-70. 10.14701/ahbps.2021.25.1.62.
Chronological analysis of surgical and oncological outcomes after the treatment of perihilar cholangiocarcinoma
- Affiliations
-
- 1Division of Hepato-Biliary and Pancreatic Surgery, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2513177
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.62
Abstract
- Backgrounds/Aims
Despite advances in surgical techniques and perioperative supportive care, radical resection of hilar cholangiocarcinoma is the only modality that can achieve long-term survival. We chronologically investigated surgical and oncological outcomes of hilar cholangiocarcinoma and analyzed the factors affecting overall survival.
Methods
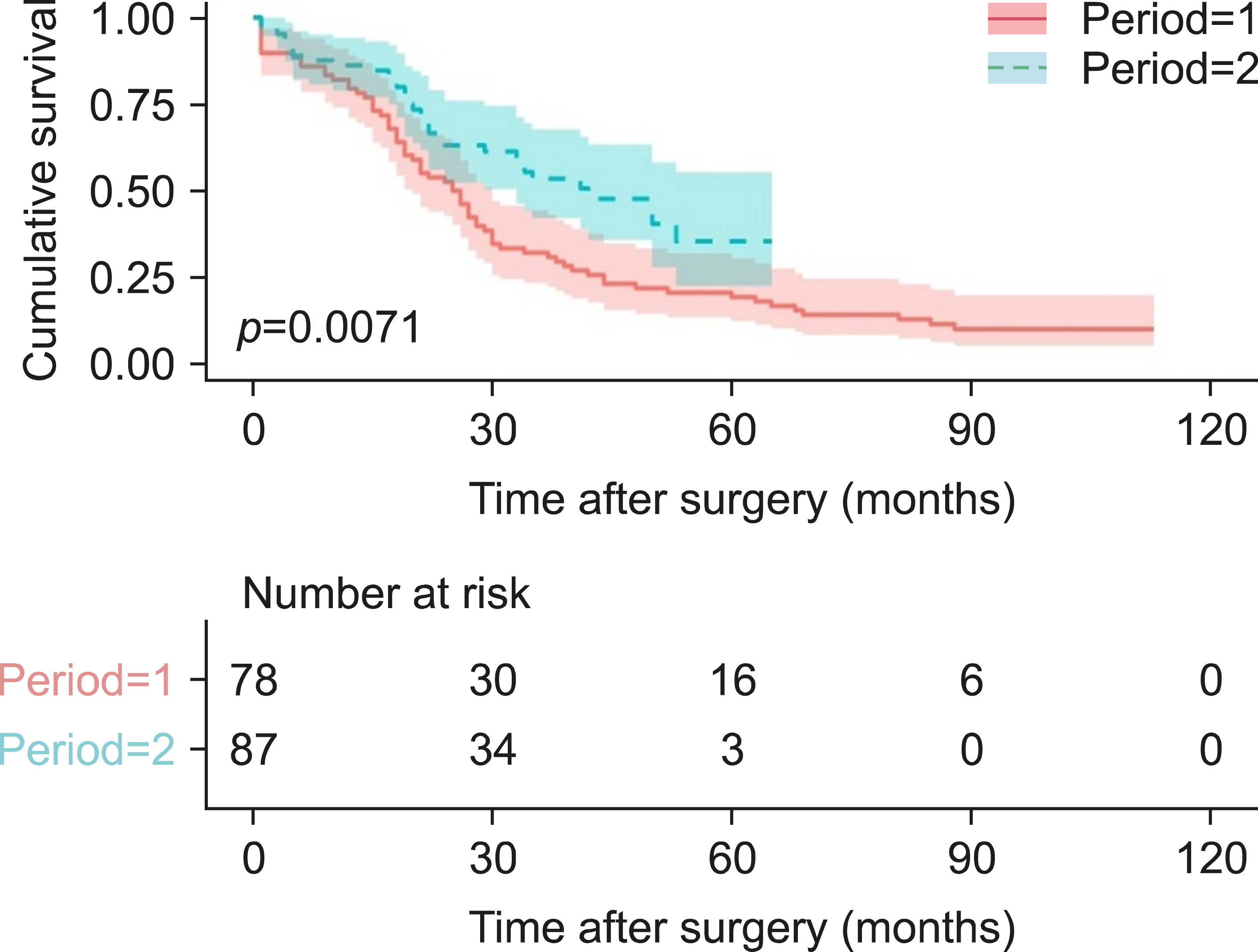
We retrospectively enrolled 165 patients with hilar cholangiocarcinoma who underwent liver resection with a curative intent. The patients were divided into groups based on the period when the surgery was performed: period I (2005-2011) and period II (2012-2018). The clinicopathological characteristics, perioperative outcomes, and survival outcomes were analyzed.
Results
The patients’ age, serum CA19-9 levels, and serum bilirubin levels at diagnosis were significantly higher in the period I group. There were no differences in pathological characteristics such as tumor stage, histopathologic status, and resection status. However, perioperative outcomes, such as estimated blood loss (1528.8 vs. 1034.1 mL, p=0.020) and postoperative severe complication rate (51.3% vs. 26.4%, p=0.022), were significantly lower in the period II group. Regression analysis demonstrated that period I (hazard ratio [HR]=1.591; 95% confidence interval [CI]=1.049-2.414; p=0.029), preoperative serum bilirubin at diagnosis (HR=1.585; 95% CI=1.058-2.374; p=0.026), and tumor stage (III, IV) (HR=1.671; 95% CI: 1.133-2.464; p=0.010) were significantly associated with poor prognosis. The 5-year survival rate was better in the period II patients than in the period I patients (35.1% vs. 21.0%, p=0.0071).
Conclusions
The surgical and oncological outcomes were better in period II. Preoperative serum bilirubin and advanced tumor stage were associated with poor prognosis in patients with hilar cholangiocarcinoma.`
Keyword
Figure
Reference
-
1. Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. 1999; Extended resections for hilar cholangiocarcinoma. Ann Surg. 230:808–818. discussion 819DOI: 10.1097/00000658-199912000-00010. PMID: 10615936. PMCID: PMC1420945.
Article2. Iwatsuki S, Todo S, Marsh JW, Madariaga JR, Lee RG, Dvorchik I, et al. 1998; Treatment of hilar cholangiocarcinoma (Klatskin tumors) with hepatic resection or transplantation. J Am Coll Surg. 187:358–364. DOI: 10.1016/S1072-7515(98)00207-5. PMID: 9783781. PMCID: PMC2991118.
Article3. Nimura Y, Kamiya J, Nagino M, Kanai M, Uesaka K, Kondo S, et al. 1998; Aggressive surgical treatment of hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 5:52–61. DOI: 10.1007/PL00009951. PMID: 9683755.
Article4. Mizuno T, Ebata T, Nagino M. 2020; Advanced hilar cholangiocarcinoma: an aggressive surgical approach for the treatment of advanced hilar cholangiocarcinoma: perioperative management, extended procedures, and multidisciplinary approaches. Surg Oncol. 33:201–206. DOI: 10.1016/j.suronc.2019.07.002. PMID: 31301935.
Article5. Kang MJ, Jang JY, Chang J, Shin YC, Lee D, Kim HB, et al. 2016; Actual long-term survival outcome of 403 consecutive patients with hilar cholangiocarcinoma. World J Surg. 40:2451–2459. DOI: 10.1007/s00268-016-3551-9. PMID: 27206402.
Article6. Tran TB, Ethun CG, Pawlik TM, Schmidt C, Beal EW, Fields RC, et al. 2019; Actual 5-year survivors after surgical resection of hilar cholangiocarcinoma. Ann Surg Oncol. 26:611–618. DOI: 10.1245/s10434-018-7075-4. PMID: 30539494.
Article7. Klempnauer J, Ridder GJ, von Wasielewski R, Werner M, Weimann A, Pichlmayr R. 1997; Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors. J Clin Oncol. 15:947–954. DOI: 10.1200/JCO.1997.15.3.947. PMID: 9060532.
Article8. Su CH, Tsay SH, Wu CC, Shyr YM, King KL, Lee CH, et al. 1996; Factors influencing postoperative morbidity, mortality, and survival after resection for hilar cholangiocarcinoma. Ann Surg. 223:384–394. DOI: 10.1097/00000658-199604000-00007. PMID: 8633917. PMCID: PMC1235134.
Article9. Liu CL, Fan ST, Lo CM, Tso WK, Lam CM, Wong J. 2006; Improved operative and survival outcomes of surgical treatment for hilar cholangiocarcinoma. Br J Surg. 93:1488–1494. DOI: 10.1002/bjs.5482. PMID: 17048280.
Article10. Han SS, Jang JY, Lee KU, Kim SW. 2008; Actual long-term outcome of Klatskin's tumor after surgical resection. Hepatogastroenterology. 55:1986–1992. PMID: 19260464.11. Bismuth H, Nakache R, Diamond T. 1992; Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 215:31–38. DOI: 10.1097/00000658-199201000-00005. PMID: 1309988. PMCID: PMC1242367.
Article12. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. 2009; The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 250:187–196. DOI: 10.1097/SLA.0b013e3181b13ca2. PMID: 19638912.13. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. 2011; Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 149:713–724. DOI: 10.1016/j.surg.2010.10.001. PMID: 21236455.
Article14. Nuzzo G, Giuliante F, Ardito F, Giovannini I, Aldrighetti L, Belli G, et al. 2012; Improvement in perioperative and long-term outcome after surgical treatment of hilar cholangiocarcinoma: results of an Italian multicenter analysis of 440 patients. Arch Surg. 147:26–34. DOI: 10.1001/archsurg.2011.771. PMID: 22250108.15. Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. 2013; Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg. 258:129–140. DOI: 10.1097/SLA.0b013e3182708b57. PMID: 23059502.16. Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. 2010; Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 17:476–489. DOI: 10.1007/s00534-009-0204-5. PMID: 19851704.
Article17. Furusawa N, Kobayashi A, Yokoyama T, Shimizu A, Motoyama H, Miyagawa S. 2014; Surgical treatment of 144 cases of hilar cholangiocarcinoma without liver-related mortality. World J Surg. 38:1164–1176. DOI: 10.1007/s00268-013-2394-x. PMID: 24305942.
Article18. Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. 2005; One hundred consecutive hepatobiliary resections for biliary hilar malignancy: preoperative blood donation, blood loss, transfusion, and outcome. Surgery. 137:148–155. DOI: 10.1016/j.surg.2004.06.006. PMID: 15674194.
Article19. Hwang HK, Jung MJ, Lee SH, Kang CM, Lee WJ. 2016; Adverse oncologic effects of intraoperative transfusion during pancreatectomy for left-sided pancreatic cancer: the need for strict transfusion policy. J Hepatobiliary Pancreat Sci. 23:497–507. DOI: 10.1002/jhbp.368. PMID: 27295957.
Article20. Kimura N, Toyoki Y, Ishido K, Kudo D, Yakoshi Y, Tsutsumi S, et al. 2015; Perioperative blood transfusion as a poor prognostic factor after aggressive surgical resection for hilar cholangiocarcinoma. J Gastrointest Surg. 19:866–879. DOI: 10.1007/s11605-014-2741-8. PMID: 25605416. PMCID: PMC4412428.
Article21. Young AL, Igami T, Senda Y, Adair R, Farid S, Toogood GJ, et al. 2011; Evolution of the surgical management of perihilar cholangiocarcinoma in a Western centre demonstrates improved survival with endoscopic biliary drainage and reduced use of blood transfusion. HPB (Oxford). 13:483–493. DOI: 10.1111/j.1477-2574.2011.00328.x. PMID: 21689232. PMCID: PMC3133715.
Article22. Jang JY, Kim SW, Park DJ, Ahn YJ, Yoon YS, Choi MG, et al. 2005; Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg. 241:77–84. DOI: 10.1097/01.sla.0000150166.94732.88. PMID: 15621994. PMCID: PMC1356849.
Article23. Capussotti L, Muratore A, Polastri R, Ferrero A, Massucco P. 2002; Liver resection for hilar cholangiocarcinoma: in-hospital mortality and longterm survival. J Am Coll Surg. 195:641–647. DOI: 10.1016/S1072-7515(02)01481-3. PMID: 12437251.
Article24. Pichlmayr R, Weimann A, Klempnauer J, Oldhafer KJ, Maschek H, Tusch G, et al. 1996; Surgical treatment in proximal bile duct cancer. A single-center experience. Ann Surg. 224:628–638. DOI: 10.1097/00000658-199611000-00007. PMID: 8916878. PMCID: PMC1235440.25. Todoroki T, Kawamoto T, Koike N, Takahashi H, Yoshida S, Kashiwagi H, et al. 2000; Radical resection of hilar bile duct carcinoma and predictors of survival. Br J Surg. 87:306–313. DOI: 10.1046/j.1365-2168.2000.01343.x. PMID: 10718799.
Article26. Jung JH, Lee HJ, Lee HS, Jo JH, Cho IR, Chung MJ, et al. 2017; Benefit of neoadjuvant concurrent chemoradiotherapy for locally advanced perihilar cholangiocarcinoma. World J Gastroenterol. 23:3301–3308. DOI: 10.3748/wjg.v23.i18.3301. PMID: 28566890. PMCID: PMC5434436.
Article27. Sumiyoshi T, Shima Y, Okabayashi T, Negoro Y, Shimada Y, Iwata J, et al. 2018; Chemoradiotherapy for initially unresectable locally advanced cholangiocarcinoma. World J Surg. 42:2910–2918. DOI: 10.1007/s00268-018-4558-1. PMID: 29511872.
Article28. Katayose Y, Nakagawa K, Yoshida H, Morikawa T, Hayashi H, Okada T, et al. 2015; Neoadjuvant chemoradiation therapy for cholangiocarcinoma to improve R0 resection rate: the first report of phase II study. J Clin Oncol. 33(3 Suppl):402. DOI: 10.1200/jco.2015.33.3_suppl.402.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is it time to define the scope of safety for robotic resection in perihilar cholangiocarcinoma surgery? A propensity score matching based analysis of a single center experience
- Gallbladder neck cancer and perihilar cholangiocarcinoma - siblings, cousins or look alikes?
- Surgery for Perihilar Cholangiocarcinoma
- Comparison of oncologic outcomes of extrahepatic cholangiocarcinoma according to tumor location: perihilar cholangiocarcinoma versus distal bile duct cancer
- Resection or transplantation for perihilar cholangiocarcinoma