Ann Surg Treat Res.
2022 Feb;102(2):100-109. 10.4174/astr.2022.102.2.100.
Comparison of oncologic outcomes of extrahepatic cholangiocarcinoma according to tumor location: perihilar cholangiocarcinoma versus distal bile duct cancer
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2525447
- DOI: http://doi.org/10.4174/astr.2022.102.2.100
Abstract
- Purpose
Extrahepatic cholangiocarcinoma is distinguished into perihilar cholangiocarcinoma (PHC) and distal bile duct cancer (DBC). The studies for each subtype have been conducted separately. This study compared oncological outcomes between PHC and DBC.
Methods
From 2001 to 2017, patients who underwent surgery at Seoul National University Hospital for PHC or DBC were enrolled. T stage was reclassified for tumor extent as ‘confined to’ or ‘beyond’ the bile duct (BD). In survival analysis, stage matching was performed based on tumor extent and lymph node (LN) metastasis.
Results
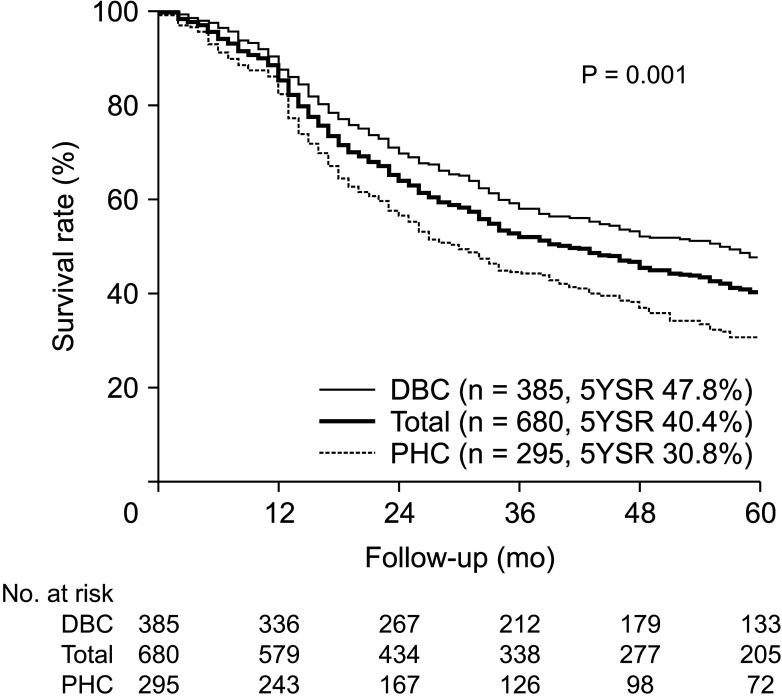
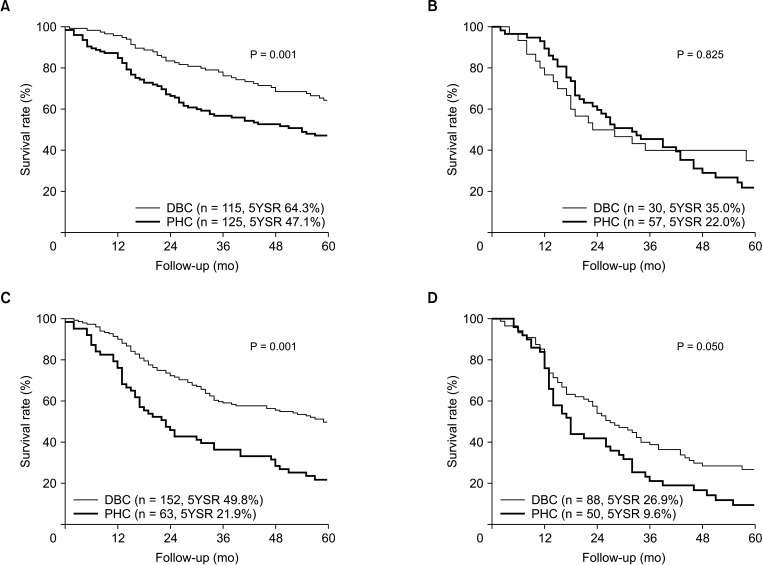
There were 680 patients enrolled: 295 with PHC and 385 with DBC. The R0 resection rate was higher in DBC (77.3% vs. 89.9%, P = 0.001). Tumors confined to BD were more common in PHC (61.7% vs. 37.7%, P = 0.001). The 5-year survival rate (5YSR) was higher in DBC patients (30.8% vs. 47.8%, P = 0.001). After stage matching, DBC patients showed better 5YSR for tumors confined to BD/LN(–) (47.1% vs. 64.3%), confined to BD/LN(+) (22.0% vs. 35.0%), beyond BD/LN(–) (21.9% vs. 49.8%), and beyond BD/LN(+) (9.6% vs. 26.9%). The overall recurrence rate was higher in PHC (59.7% vs. 51.9%, P = 0.045), with no difference in the recurrence types between two groups. Radiation therapy was effective for patients with advanced stage disease (5YSR: 35.8% vs. 29.5%, P = 0.022); adjuvant chemotherapy was effective for patients receiving R1 resection (5YSR: 37.3% vs. 13.2%, P = 0.040).
Conclusion
Differences were identified in oncological outcomes between PHC and DBC, including pathologic findings and survival outcomes.
Figure
Reference
-
1. Razumilava N, Gores GJ. Classification, diagnosis, and management of cholangiocarcinoma. Clin Gastroenterol Hepatol. 2013; 11:13–21. PMID: 22982100.
Article2. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID: 30207593.
Article3. Ke Q, Wang B, Lin N, Wang L, Liu J. Does high-grade dysplasia/carcinoma in situ of the biliary duct margin affect the prognosis of extrahepatic cholangiocarcinoma? A meta-analysis. World J Surg Oncol. 2019; 17:211. PMID: 31818290.
Article4. Tyson GL, Ilyas JA, Duan Z, Green LK, Younes M, El-Serag HB, et al. Secular trends in the incidence of cholangiocarcinoma in the USA and the impact of misclassification. Dig Dis Sci. 2014; 59:3103–3110. PMID: 25204668.
Article5. Akamatsu N, Sugawara Y, Hashimoto D. Surgical strategy for bile duct cancer: advances and current limitations. World J Clin Oncol. 2011; 2:94–107. PMID: 21603318.
Article6. Jang JY, Kim SW, Park DJ, Ahn YJ, Yoon YS, Choi MG, et al. Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg. 2005; 241:77–84. PMID: 15621994.
Article7. Seyama Y, Makuuchi M. Current surgical treatment for bile duct cancer. World J Gastroenterol. 2007; 13:1505–1515. PMID: 17461441.
Article8. Shin HR, Oh JK, Masuyer E, Curado MP, Bouvard V, Fang Y, et al. Comparison of incidence of intrahepatic and extrahepatic cholangiocarcinoma: focus on East and South-Eastern Asia. Asian Pac J Cancer Prev. 2010; 11:1159–1166. PMID: 21198257.9. Esnaola NF, Meyer JE, Karachristos A, Maranki JL, Camp ER, Denlinger CS. Evaluation and management of intrahepatic and extrahepatic cholangiocarcinoma. Cancer. 2016; 122:1349–1369. PMID: 26799932.
Article10. Reding R, Buard JL, Lebeau G, Launois B. Surgical management of 552 carcinomas of the extrahepatic bile ducts (gallbladder and periampullary tumors excluded). Results of the French Surgical Association Survey. Ann Surg. 1991; 213:236–241. PMID: 1705417.
Article11. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474. PMID: 20180029.
Article12. Blechacz B. Cholangiocarcinoma: current knowledge and new developments. Gut Liver. 2017; 11:13–26. PMID: 27928095.
Article13. Ercolani G, Dazzi A, Giovinazzo F, Ruzzenente A, Bassi C, Guglielmi A, et al. Intrahepatic, peri-hilar and distal cholangiocarcinoma: three different locations of the same tumor or three different tumors? Eur J Surg Oncol. 2015; 41:1162–1169. PMID: 26095704.
Article14. Waseem D, Tushar P. Intrahepatic, perihilar and distal cholangiocarcinoma: management and outcomes. Ann Hepatol. 2017; 16:133–139. PMID: 28051802.
Article15. Al Mahjoub A, Bouvier V, Menahem B, Bazille C, Fohlen A, Alves A, et al. Epidemiology of intrahepatic, perihilar, and distal cholangiocarcinoma in the French population. Eur J Gastroenterol Hepatol. 2019; 31:678–684. PMID: 30633038.
Article16. Murakami Y, Uemura K, Sudo T, Hashimoto Y, Nakashima A, Kondo N, et al. Prognostic factors after surgical resection for intrahepatic, hilar, and distal cholangiocarcinoma. Ann Surg Oncol. 2011; 18:651–658. PMID: 20945107.
Article17. DeOliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, et al. Cholangiocarcinoma: thirty-one-year experience with 564 patients at a single institution. Ann Surg. 2007; 245:755–762. PMID: 17457168.18. Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996; 224:463–473. PMID: 8857851.19. Yoshida T, Matsumoto T, Sasaki A, Morii Y, Aramaki M, Kitano S. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch Surg. 2002; 137:69–73. PMID: 11772220.
Article20. Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005; 137:396–402. PMID: 15800484.
Article21. Hu HJ, Mao H, Shrestha A, Tan YQ, Ma WJ, Yang Q, et al. Prognostic factors and long-term outcomes of hilar cholangiocarcinoma: a single-institution experience in China. World J Gastroenterol. 2016; 22:2601–2610. PMID: 26937148.
Article22. Bird N, McKenna A, Dodd J, Poston G, Jones R, Malik H. Meta-analysis of prognostic factors for overall survival in patients with resected hilar cholangiocarcinoma. Br J Surg. 2018; 105:1408–1416. PMID: 29999515.
Article23. Wellner UF, Shen Y, Keck T, Jin W, Xu Z. The survival outcome and prognostic factors for distal cholangiocarcinoma following surgical resection: a meta-analysis for the 5-year survival. Surg Today. 2017; 47:271–279. PMID: 27236779.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic Cholangiocarcinoma: Evolving Concepts and Medical Treatment
- Molecular pathogenesis and the role of tumor markers in cholangiocarcinoma
- Papillary Cholangiocarcinoma Located in the Distal Common Bile Duct
- The epidemiology and risk factors of hilar cholangiocarcinoma
- Parenchyma-preserving hepatectomy including segments I + IV resection and bile duct resection in a patient with type IV perihilar cholangiocarcinoma: A case report with video clip